Paramedics in the UK working in traditional land ambulance roles do not frequently attend critically ill or injured patients (Henderson et al, 2019).
Following the peak of the COVID-19 pandemic, extended waiting times outside hospitals have occurred at emergency departments across the UK (Royal College of Emergency Medicine, 2022), which have caused knock-on delays for ambulance services (British Medical Association, 2022).
This has created a situation where ambulance crews are often waiting for hours to hand patients over, reducing the number of incidents attended during a shift and therefore reducing exposure to a variety of clinical situations and, potentially, the number of clinical skills they are using.
In addition, student paramedics and newly qualified paramedics need to gain exposure to a wide variety of patients; this can enable them to meet the Health and Care Professions Council (HCPC) (2023) standards of proficiency as well as individual ambulance trust requirements. Regular exposure to skills in the context where they are normally used is needed to maintain performance (Godden and Baddeley, 1975; Ericsson, 2008; Pusic et al, 2012).
The potential reduction in clinical exposure could damage the competence of students, graduates and experienced paramedics alike, impacting negatively on their wellbeing and clinical practice (Health Education England, 2018).
This discussion led the authors to consider the competency levels of paramedics practising in the traditional role who are potentially getting less patient exposure because of current pressures on the NHS.
Aims and objectives
The aim of this study was to observe the performance of clinical skills of paramedics ranging in complexity and frequency of exposure. This was done to achieve the following objectives:
Method
The study investigated whether paramedic competence was affected by the frequency of use and/or complexity of a clinical skill being practiced, it also explored selected demographic factors in relation to this. Participants were also asked what skills they thought were easiest/most difficult to perform. Ethical approval for this study was obtained from the Health Research Authority as well as the University of Plymouth.
Sample, recruitment and participant characteristics
Qualified paramedics were recruited from one ambulance service in the south west of the UK, via an advertisement in the local ambulance service bulletin and subsequent snowballing. Interested paramedics were provided with a participant information sheet and invited to a data collection day. Upon arrival on the day, after a discussion regarding participation, a consent form was completed.
The paramedics were then assigned a participant number to guarantee their anonymity after taking part, and informed of their right to withdraw at any point before data analysis without penalty.
The following characteristics were assessed: biological sex; age; years as a paramedic; length of career breaks; training/education route; and whether they were in a practice educator role. These were considered to be a broad selection of characteristics that could offer insights regarding confidence, competence and perception of competence within the profession.
Procedure
Participants took part in a short clinical scenario where they used clinical skills that fell within the scope of practice for a paramedic operating in a traditional (non-specialist) ambulance service role.
Skills were selected based on their frequency as established in a previous study (Henderson et al, 2019) and complexity, which was informed by local ambulance service clinical role descriptors (e.g. emergency care assistant and paramedic) to differentiate between simple and complex (Table 1).
| Simple | Complex | |
|---|---|---|
| Frequent | Oxygen administration | Intravenous cannulation |
| Infrequent | Basic airway maintenance: manual manoeuvres and basic airway adjuncts | Intermediate/advanced airway maintenance: supraglottic airway devices and endotracheal tubes |
The clinical scenario was set up in a skills lab at the local university. It began with a patient experiencing cardiac chest pain (actor; intravenous (IV) cannulation performed on a simulation arm and oxygen delivery (simulated by the use of a modified non-rebreathing mask) before deteriorating into cardiac arrest (a manikin positioned behind a screen during the first part of the scenario).
The scenario ran continuously for each participant and was managed as a single-person paramedic response. This allowed clinical skills to be assessed throughout the scenario; these were oxygen administration and IV cannulation during the pre-arrest phase, followed by basic and intermediate airway management in the post-cardiac arrest phase. All clinical skills were clearly indicated based on the patient's presentation, history and observations. Each participant was recorded using a camcorder; performance was evaluated in real time but recordings could be reviewed if there was any uncertainty about events.
Participant performance was measured using a rubric scoring tool aligned to local ambulance service and national practice guidelines. While this focused on the technical aspects of skills, it also included elements of communication, including explanation of procedures and consent. In addition, the lead researcher (TH) made notes about participant performance during the clinical scenario, which provided some deeper insight into actions taken.
The rubric was developed using local university examples that had been tried and tested for its paramedic degree; before data collection, it was piloted with four local, final-year student paramedics.
Analysis
Demographic data and clinical scenario observation scores were summarised using descriptive statistics. Overall mean scores for individual skills during the scenario were found to have a skewed distribution and therefore Friedman's test was used for their analysis. Scores for differences in performance between educator roles (practice educator (PEd) versus non-practice educator) were assessed using the Mann-Whitney U test.
Results
Participant characteristics
Sixty-nine paramedics took part in this study. There were 18 women and 51 men and the median age range was 20–29 years, accounting for almost 50% of participants. An average of 4.14 years (range 0.08–25 years) as a paramedic had been spent in clinical practice. Participant characteristics collected are shown in Table 2.
| Demographic | Value | Frequency |
|---|---|---|
| Sex (biological) | Male | 73.91% (n=51) |
| Female | 26.09% (n=18) | |
| Age (years) | 20–29 | 47.83% (n=33) |
| 30–39 | 26.09% (n=18) | |
| 40–49 | 21.74% (n=15) | |
| 50–59 | 4.35% (n=3) | |
| >60 | 0% (n=0) | |
| Years as a paramedic | Average (mean) | 4.14 years |
| Range | 0.08–25 years | |
| Career breaks | Number of participants | 10.14% (n=7) |
| Years (mean) | 1.14 | |
| Training/education route | Non-university | 18.84% (n=13) |
| University | 81.16% (n=56) | |
| Practice educator | Yes | 15.94% (n=11) |
| No | 84.06% (n=58) |
Observed performance scores
The mean performance scores for each skill during the scenario rated by the researcher are summarised in Table 3.
| Ranking: |
Mean % score | % range | |
|---|---|---|---|
| Basic airway maintenance | 1 | 79.30 | 14.29–100 |
| Intravenous cannulation | 2 | 77.40 | 44.44–100 |
| Intermediate/advanced airway maintenance | 3 | 74.32 | 0–100 |
| Oxygen administration | 4 | 58.37 | 0–80.94 |
The Shapiro-Wilk test showed that performance scores had a skewed distribution so comparisons were made using a non-parametric test. Friedman's test showed there were significant differences between the scores: chi-squared (3; n=69) =67.260; P<0.001.
The scores were highest (indicating better performance) for basic airway maintenance followed by IV cannulation and then intermediate/advanced airway maintenance, with the lowest score achieved for oxygen administration.
Oxygen administration is a key result (Table 3). It is a simple and frequent skill but ranked the lowest of all four skills in terms of mean score. This was largely down to 16% (n=11) of participants not administering it at all or doing so without consent.
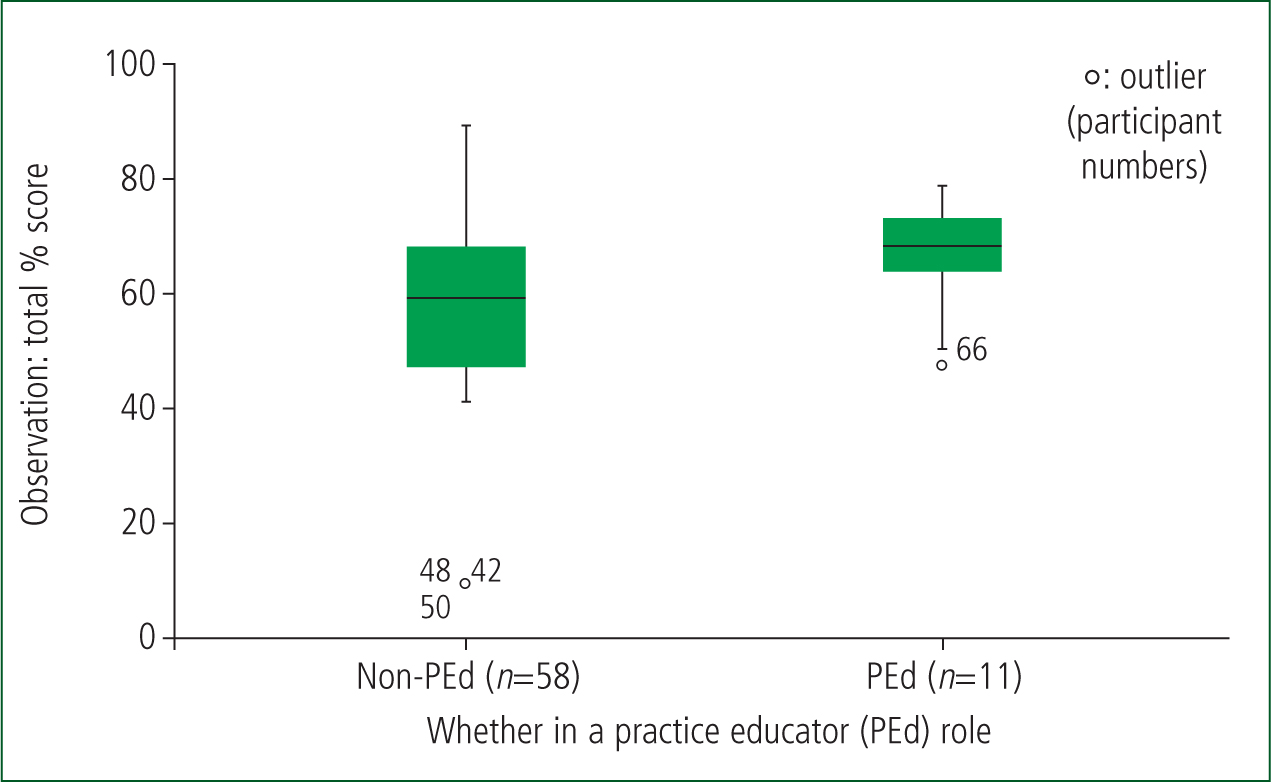
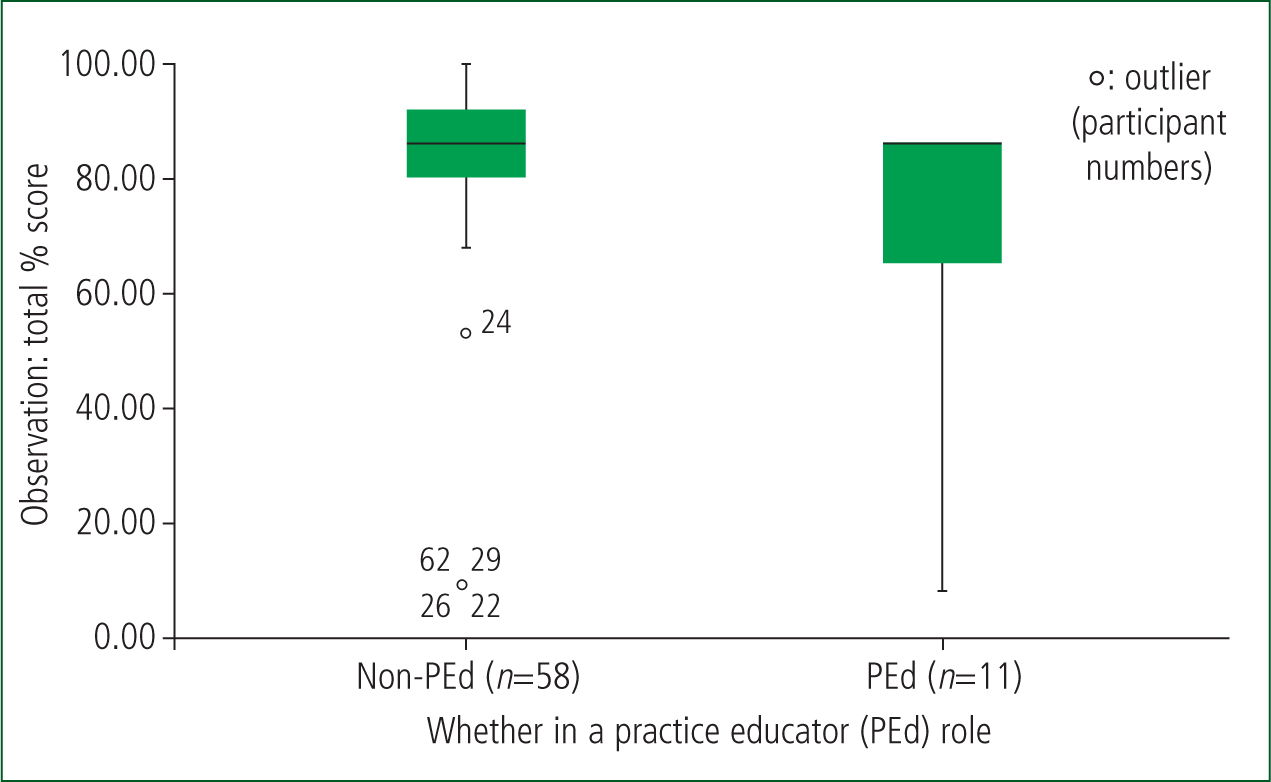
PEds scored higher on the oxygen administration element of the scenario and lower on intermediate/advanced airway management.
The above findings were explored further using a Mann-Whitney U test. This identified a significant difference in oxygen administration observation scores between PEds and non-PEds: PEd (Md=66.67; n=11); non-PEd (Md=57.14; n=58); U=185.000; z=−2.209; P<0.05. In relation to intermediate/advanced airway maintenance, a significant difference was also found when a Mann-Whitney U test was applied: PEd (Md=83.33; n=11) and non-PEd (Md=83.33; n=58); U=198.00; z=−2.055; P<0.05.
Figures 1 and 2 show boxplots for mean oxygen administration and intermediate/advanced airway maintenance respectively. These demonstrate the difference and detail across the scores, despite, for example, the median scores for intermediate/advanced airway management and PEd/non-PEd being the same.
Participants were asked which of the skills they found the easiest and which they found the most difficult to perform (Table 4).
| Skill | Easiest | Ranking: 1: easiest | Most difficult | Ranking: 1: hardest |
|---|---|---|---|---|
| Oxygen administration | 52.17% (n=36) | 1 | 11.59% (n=8) | 4 |
| Intravenous cannulation | 24.64% (n=17) | 2 | 31.88% (n=22) | 2 |
| Basic airway maintenance | 10.14% (n=7) | 4 | 20.29% (n=14) | 3 |
| Intermediate/advanced airway maintenance | 11.59% (n=8) | 3 | 33.33 (n=23) | 1 |
| Not recorded | 1.45% (n=1) | 2.90% (n=2) | ||
More than half of participants deemed oxygen administration as the easiest skill to perform; however, this was not reflected in the researcher-observed performance scores, where it was the lowest-scoring skill.
Discussion
Procedural skills
Infrequent practice of airway management (including the use of supraglottic airways) by paramedics in the UK has been highlighted by Younger et al (2016). Similarly, research by Henderson et al (2019) established that paramedics infrequently attended critically ill or injured patients. In this context, the mean scores for all skills were impressive and to be commended.
The results showed no significant difference in performance between graduate and non-graduate paramedics on the skills assessed in this study. Similarly, differences regarding sex, age and time practising as a paramedic were not associated with significant variation between performance.
Cooper (2005), in a now dated but geographically relevant qualitative study, interviewed ambulance staff of various clinical grades to elicit their opinions and feelings about training and education within the context of developing roles and skills. Concern from clinicians regarding de-skilling in interventions infrequently practised (such as those above) was highlighted. This concern is reflected with participants in this study rating intermediate/advanced airway management as the most difficult of this set of skills. In terms of their competence, participants performed well in this skill (mean score 74.32%), although it came third overall regarding performance score out of the four skills assessed. A mean of 74.32% indicates a good level of performance, although the wide range (0–100%) may indicate individuals had some specific issues.
Despite basic airway maintenance (manual manoeuvres and basic airway adjuncts) being the skill with the highest score, participants sometimes opted not to carry out each individual step of escalation (i.e. manual manoeuvres to basic adjuncts) during the scenario, saying that this was so they could progress to a more advanced method of airway management more quickly. Although this provides a potentially acceptable explanation for the absence of basic airway steps, it does not explain why manual airway manoeuvres would be missed out in some cases, given that they would be required to open the airway initially to check the ventilatory status of a patient. This may indicate a lack of working knowledge. More experienced clinicians may demonstrate a willingness to deviate from guidelines (Wyatt, 2003).
Benner's (1982) work on the journey from novice to expert highlighted that experts would sometimes deviate from guidelines and cut corners; furthermore, this work highlighted that experts were often unable to provide a rationale for decisions or practice, often qualifying it as ‘something they just felt or did’.
Some elements were completed out of sequence. Specifically, this concerned IV cannulation, where the tourniquet was not released before the cannula stylet was removed. This sequence in practice would mean the stylet was removed while there was still increased pressure in the vein, thus risking haemorrhage; although unlikely to be life threatening, this could damage patient confidence in the clinician, raise questions about professional standards and is contradictory to the bioethical principle of non-maleficence (Beauchamp and Childress, 2001).
The IV cannulation procedure finding is confusing. There does not seem to be an identifiable rationale for completing the exercise in this order, nor does it offer a time or a clinical benefit; in addition, it was an error made by participants with both educational backgrounds and with a range of experience. The lead author (TH) felt it might demonstrate a lack of deeper understanding; the order in which these elements are completed is dictated by a mechanical knowledge of what each individual step achieves.
It was initially considered possible that a ‘surface learning’ approach from non-graduates may have explained a lack of understanding with this procedure (Bradley, 2005; Cooper, 2005; Association of Ambulance Chief Executives, 2011; Ryan and Halliwell, 2012; Lovegrove and Davis, 2013); however, there was not a significant difference in performance between graduates and non-graduates so this is not supported by the results.
During intermediate/advanced airway maintenance (supraglottic airway device and endotracheal tube), no students opted to perform endotracheal intubation, perhaps a reflection of contemporary practice in the local area, where it is a skill practised by paramedics with enhanced/specialist skills.
Elements of the supraglottic airway device procedure were commonly missed; these included a lack of auscultation and failing to tie the device in place. The design of the scenario rubric meant that justification for this was often explored with the candidate in a scenario debrief. In contrast to the situation with IV cannulation, candidates generally cited speed of practice as the reason for postponing auscultation. This is perhaps clinically justifiable when considering post-placement auscultation because of the design of the scenario (single-person response) and the anatomical positioning of a supraglottic airway. Again, this may link back to the work of Benner (1982), where expert clinicians may make decisions to streamline practice. When describing the rationale for not tying the device in, participants often cited evidence in relation to avoiding any interruption to chest compressions (Soar et al, 2015).
In some cases, defibrillation or chest compressions were delayed, or chest compressions were suboptimal. Although these aspects were not measured for this study, they are linked inextricably with airway maintenance as part of cardiopulmonary resuscitation. These observations often seemed to be connected to points of high cognitive demand during the scenario, for example immediately following the cardiac arrest when decisions around managing a failing airway had to be made in conjunction with ensuring early defibrillation and effective, timely compressions. The ability to make effective decisions in these situations is often connected to knowing and understanding current evidence around management of the cardiac arrest patient (Carley, 2007). However, paramedics must also take into account the situation at hand—a single-person response with a challenging clinical situation—where it is not possible to satisfy best practice.
An American observational study (DeAnda and Gaba, 1991) looking at experience and performance in simulated clinical scenarios found anaesthetists sometimes made errors in managing critical incidents; it suggested that more experience and exposure to stressful situations enabled clinicians to be more cognisant of their performance, identifying issues as they occurred and rectifying them at the time. Almost half the participants in this study were aged 20–29 years and had a mean length of practice of 4.14 years. Being relatively young and new to practice perhaps explains the difficulty in correcting issues arising during the scenario while trying to manage an evolving situation.
Mean scores for oxygen administration and intermediate airway management indicated significant differences between performances of practice educators and non-practice educators. Practice educators scored higher for oxygen administration and lower for intermediate airway management. Practice educators are likely to be more experienced and therefore this finding may be explained by a willingness to deviate from guidelines (thus scoring less) as a result of experience, as mentioned above (Wyatt, 2003). As stated previously, Benner's (1982) work on the journey from novice to expert highlighted that experts will sometimes deviate from guidelines and cut corners.
Consent for oxygen administration/intravenous cannulation
During the observed clinical scenario, consent for administration of oxygen and IV cannulation was often incomplete and, in some cases, absent; the simulated patient was often asked by the participant if they could cannulate them but rarely gave the pertinent risks/benefits of this or the opportunity to ask questions about the procedure. Sometimes in an emergent situation, clinicians need to make best-interest decisions without seeking consent; however, this is more often done where the patient lacks capacity (Gaisford, 2017; Griffith, 2009). The skills mentioned above (oxygen administration and IV cannulation) were performed at a point in the scenario where the patient had clear capacity, suggesting this was not a best-interest decision by paramedic participants.
An Australian review, which included case studies, acknowledged the difficulty experienced by practitioners working in emergency care when seeking consent; it listed various reasons for this, such as time pressure, emotion, information deprivation, conflict, stress and fatigue (Steer, 2007). It highlighted the difficulties in trying to address consent when in an uncontrolled, dynamic environment. The lack of consent during the scenario may be linked to the desire of participants to make progress with assessment and treatment when they know the presentation is time-sensitive.
Another possible factor in this observation are the findings of a UK questionnaire study by Evans et al (2007), which examined the knowledge of doctors, nurses and ambulance staff around consent and capacity. This concluded that knowledge in this area was lacking; ambulance staff failed to record any correct answers for some questions. This study is now over 10 years old and undertaken before the introduction of widespread higher education for the paramedic profession. Degree programmes are now rightly expected to include consent and capacity in their curricula (College of Paramedics, 2019; HCPC, 2023).
The literature relating to the law and consent was reviewed by Griffith (2009). The focus of the review was the need to achieve valid consent, and the author acknowledged that the patient needed ‘sufficient’ information based on the intervention that was to be undertaken. Subsequently, Gaisford (2017) explored the concept of consent and informing the patient of risks that are so significant they should be mentioned; this was not done by participants in this study. Gaisford (2017) acknowledges the difficulty in doing this and the subjectivity that exists when considering such detail.
Stress, anxiety and performance
The author observed that some participants found the scenario progression stressful and/or anxiety-inducing. This was particularly apparent during management of a failing airway in the recently arrested patient.
There is significant overlap between anxiety and stress. Anxiety is heightened vigilance, with limited control over worrying thoughts, giving greater attention to the negative (Lukasik et al, 2019). Stress, on the other hand, can be a positive factor for performance, depending on its level (Yerkes and Dodson, 1908; Lukasik et al, 2019).
Although participants generally performed well, some made questionable management decisions. Anxiety is associated with a reduction in working memory, reducing the ability to make decisions and reason (Lukasik et al, 2019). The same authors identified that stress did not have the same negative effects. An earlier review of the literature found, similarly, that anxiety is linked to poor performance (Moran, 2016). This would give weight to the observation that, under the pressure of the scenario, some participants became anxious, often verbalising what they felt was going wrong and subsequently struggling to make sound decisions—a vital skill in paramedic practice.
As mentioned previously, a seminal study by Yerkes and Dodson (1908) proposed that, although some stress can improve performance, if the stress becomes too great, it to can begin to have a negative impact. This has been further established in emergency care by Lauria et al (2017); specifically, the authors suggested that people under high stress may adopt behaviours to cope, and this may explain some of the adjustments to practice that have been previously discussed.
An Australian literature review highlighted the benefits on performance of using psychological skills training to overcome excess stress/anxiety and improve performance (Lauria et al, 2016). Specifically mentioned by Lauria et al (2016) is the benefit of stress inoculation training; this process involves exposing clinicians to small amounts of stress, which builds their confidence and enables performance for a time when they are put under higher levels of stress in practice (LeBlanc, 2009). The concept of stress inoculation training leads us back to the importance of regular exposure to experiences to build confidence and performance.
Conclusion
Participants from the study were largely young (aged 20–29 years), university-educated paramedics, with a mean of 4.14 years in practice. They felt they would be most competent in oxygen administration and least competent in intermediate/advanced airway management. Contrary to this, although all skills performance scores were good, the highest were in basic airway management followed by IV cannulation, then intermediate/advanced airway management and, lastly, oxygen administration. This suggests that frequent, simple skills will not always be the best performed by paramedics. There was no significant difference in performance by sex, age group and education route.
Within the scenario, elements of certain skills were missed by some participants; there was sometimes a pattern to this, such as differences between PEd and non-PEd practitioners. It is difficult to say whether some of the missed elements were conscious, informed actions taken by an expert to streamline practice and speed up treatment or the result of a lack of understanding or knowledge.
Anxiety and particularly high stress levels also probably had a negative impact on performance.
In addition, participants commonly neglected to achieve valid consent, something recognised in the literature and perhaps a result of the complex nature of prehospital care in conjunction with the desire to treat the patient quickly.

