Placental transfusion (the transfer of blood from the placenta to the neonatal circulation after birth) can improve blood volume by up to 30% and decrease overall neonatal mortality (Backes et al, 2014). Currently, only vigorous (healthy) babies are treated via this strategy (Mercer Erickson-Owens, 2014; Song et al, 2017). Worldwide, 5% of babies born will require some form of resuscitation to promote adequate ventilation (Blank et al, 2018). Despite the potential benefit that placental transfusion can bring, a need to resuscitate can often interfere with the prehospital clinician's ability to perform transfusion.
When a newborn is delivered in a compromised state, the current prehospital guidelines from the Resuscitation Council UK (2015) and the Joint Royal Colleges Ambulance Liaison Committee (JRCALC) (2019) advocate cutting the umbilical cord immediately so the newborn can be moved to an appropriate setting to initiate resuscitation. The resuscitation algorithm accepted internationally for newborns is quite different from that for adult or child life support. The focus is on optimising airway management and inflating the lungs as, for most babies, this will be all that is needed (Resuscitation Council UK, 2015). It is widely accepted that placental transfusion by delayed cord clamping (DCC) or umbilical cord milking (UCM) should be undertaken for all vigorous newborns and this is reflected in current guidelines.
DCC is the practice of waiting for the umbilical cord to stop pulsating before clamping and cutting it; UCM is clamping and cutting the cord, then immediately milking the cord towards the neonate to expel leftover volume. Standard care for the ambulance service in the UK is DCC, or to cut the cord immediately if resuscitation is required (JRCALC, 2019). The reasons for this are predominantly practical, such as because the cord is short or there are concerns that leaving the cord intact may delay or negatively impact resuscitation efforts because of space confines and human factors.
In an empirical study, paramedic skills and knowledge of neonate resuscitation were shown to improve significantly following education (Mileder et al, 2019). However, skills fade within this field with a lack of exposure, which leads to a poorer decision-making ability because of stress (McLelland et al, 2014). There is a significant lack of evidence regarding prehospital use of transfusion strategies and current guidelines are based on consensus opinion.
In a systematic review of placental transfusion strategies, Rabe et al (2012) and Backes et al (2014) found placental transfusion in hospital versus none significantly decreased mortality, lowered the need for blood transfusions and reduced the likelihood of intraventricular haemorrhage. Incidences of necrotising enterocolitis, sepsis and length of stay have been found to be significantly lower in neonates receiving longer DCC (Chiruvolu et al, 2018). Placental transfusion is thought to decrease mortality by increasing the circulating blood volume, which may contribute to stabilising the cardiovascular system and increasing end-organ perfusion. Mercer et al (2014) discuss how increasing organ perfusion reduces the severity of the inflammatory response and prevents damage from ischaemia.
Little is known about transitioning neonatal blood volumes as placental transfusion strategies are considered too invasive and have therefore not been ethically approved for human studies. Studies in newborn lambs show that DCC improved blood volume during the transition from placental to neonatal circulation (Mercer and Erickson-Owens, 2014; Blank et al, 2018).
Prehospital resuscitation of newborns does not happen often, but can be an overwhelming situation for clinicians to be in. In view of the benefits that have been proven, the potential negative impact of DCC and UCM on resuscitation attempts should be evaluated.
Research question
The research question was developed using PICO (Table 1). As many reviews have already found them to be equally effective, DCC and UCM were used together to consider both strategies for placental transfusion rather than compare them (Backes et al, 2014). For comparison, immediate cord clamping was used, as this is what is recommended. Park et al (2018) found that Apgar score at 5 minutes was the best predictor of mortality in neonates, and this was used to accurately measure an outcome. This is an internationally accepted method to assess a newborn that considers Appearance, Pulse, Grimace, Activity and Respiration, and yields a score out of 10. A score of 10 is associated with a healthy newborn, and 0 with no signs of life. To establish whether there was a delay to resuscitation efforts with placental transfusion, the time to resuscitation starting and time to first inflation breath were also included as an outcome; this allowed comparison with the control group.
| PICO was used to develop the research question as shown below | |
|---|---|
| Population | Newborn babies requiring resuscitation |
| Intervention | Placental transfusion by either delayed cord clamping (DCC) or umbilical cord milking (UCM) |
| Comparison | Immediate clamping of the umbilical cord |
| Outcome | Time to initiating resuscitation/time to first inflation breath/impact on Apgar score at 5 minutes |
Aims
The current study aimed to determine whether placental transfusion is practical for prehospital clinicians to undertake in the community, and whether it negatively impacts resuscitation by delaying the start of treatment or has any impact on infant mortality.
Objectives
Methodology
Search strategy
CINAHL (Cumulative Index to Nursing and Allied Health Literature), MEDLINE, AMED (Allied and Complementary Medicine Database) and the British Nursing Index (BNI) were searched on 10 March 2019. These databases were chosen as the intention was to capture all relevant studies across a range of medical specialties that may be involved in the resuscitation of newborns.
Background reading and pilot searches were used to identify search terms, which are shown in Table 2. Titles were screened for relevance and abstracts read for suitability. Not all studies included in the review had time to resuscitation Apgar at 5 minutes as primary outcomes, but these were each recorded as a secondary outcome so were picked up during abstract examination.
| Resuscitation | AND | Umbilical cord |
| OR | ||
| Umbilical cord clamping | ||
| OR | ||
| Umbilical cord milking |
| Inclusion | Exclusion |
|---|---|
| Studies that compared placental transfusion to immediate cord clamping | Full text not available |
| Studies that included neonates requiring resuscitation | Not written in English |
| Randomised controlled trials and cohort studies | Direct comparisons of delayed cord clamping and umbilical cord milking |
| Published between 2017 and 2019 | Animal studies |
Exclusion/inclusion criteria
The databases were filtered for peer-reviewed articles published during 2017–2019. Using a limited timescale ensured that the most recent research was captured. Articles involving animals were excluded because the present review focuses on humans and it can be difficult to apply animal data to human outcomes owing to differences in physiology. Expert opinion and low-grade research, as described by Aveyard (2014), were excluded as the current review looks specifically at time outcomes, which require a level of statistical analysis from reliable data.
As a large amount of research compares DCC and UCM, articles were excluded if they did not directly measure either time to first breath or time to starting a resuscitation attempt. Because of the financial limitations of the lead researcher, papers not written in English were excluded.
Results
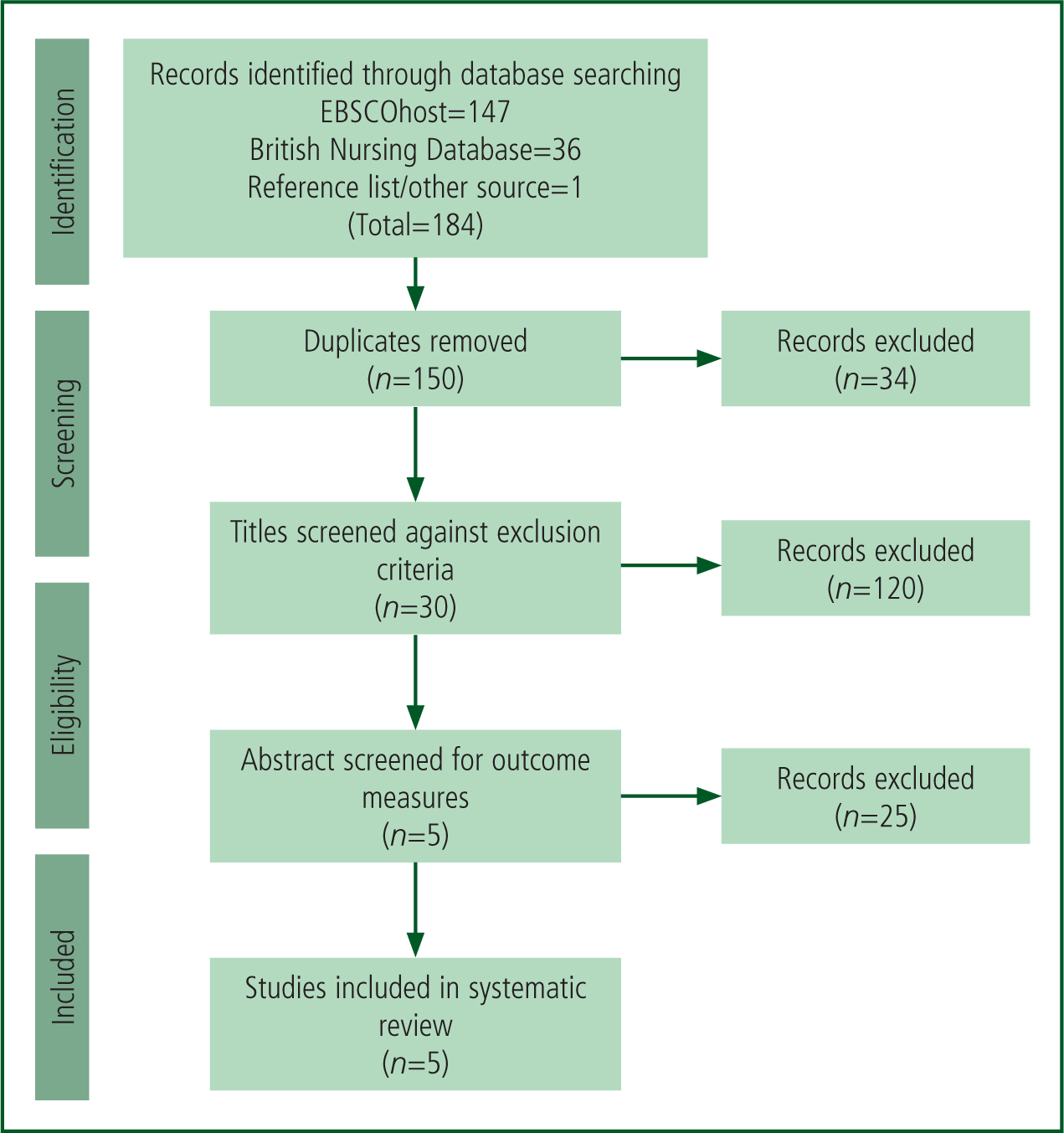
The outcome of the search is shown in the PRISMA diagram (Figure 1) (Moher et al, 2009). Five papers including all of the set criteria were found and selected for critical analysis. Three were randomised controlled trials (RCTs) and two were cohort studies. It was appropriate to analyse them separately according to level of evidence to obtain the most efficient comparison. A critical appraisal tool (Joanna Briggs Institute, 2018) was applied to each category of evidence to allow systematic appraisal.
Analysis
Randomised controlled trials
RCTs are level 2 evidence and often used to investigate whether something is effective or feasible (Aveyard, 2014). Both Girish et al (2018) and Anup et al (2017) conducted feasibility trials on placental transfusion techniques with resuscitation, while Ram Mohan et al (2018) evaluated the effectiveness of cord milking, measuring time to resuscitate as a secondary outcome.
Anup et al (2017) and Ram Mohan et al (2018) used true randomisation in the form of random number generators and opaque envelopes while Girish et al (2018) randomised neonates by month of birth. This quasi-randomised technique can be criticised for not concealing treatment groups as they are not randomised at the point of intervention so bias could arise. Similarly, because of the nature of the intervention, the clinicians involved in all the trials could not be blinded; however, both Anup et al (2017) and Ram Mohan et al (2018) blinded their researchers during follow-up, which may limit any potential bias in data collection. As Girish et al (2018) blinded neither the clinician nor the researcher, the results risk being influenced by behavioural bias depending on the individuals’ own opinions regarding the trial.
The similar exclusion criteria of the three trials possibly affected the validity of their results, but allowed for better baseline characteristic comparison. In all three studies, a selected group of health professionals were enrolled to provide the intervention but Ram Mohan et al's (2018) paper was the only one to record exactly how they were trained and to have allocated a principle investigator to ensure adherence to the policy. Two studies were conducted in India, with Girish et al (2018) collecting data across two sites.
Patient demographics and confounding factors may influence the generalisability of the results. Girish et al (2018) hypothesised that placental transfusion could be used as an alternative treatment for hypoxic-ischaemic encephalopathy (HIE). In developed healthcare systems, neonates experiencing HIE are treated with targeted temperature management (therapeutic hypothermia), which may not always be accessible in developing countries and is not always successful in these regions (Girish et al, 2018). The results of the present study may therefore apply more to healthcare-deprived countries.
Follow-up was completed in all three trials other than in two patients in Ram Mohan et al's (2018) study, where parents discharged a neonate against medical advice.
Girish et al (2018) found no significant difference between the groups receiving UCM compared to immediate cord clamping with regard to time to resuscitation. Despite having the largest sample size, it was the only trial with no power percentage to observe a relevant statistical difference recorded.
Anup et al (2017) were comparing specific timing of an intervention, so data were collected at a single point, primarily by calling out the numerical values and recording these in the delivery room. Data collection in this manner is subject to human error and could be less reliable as continuous measurement may yield a different result (Anup et al, 2017). To mitigate this risk, data were also downloaded from the medical equipment. Anup et al (2017) observed no significant difference in timing to resuscitation in both groups but did find a trend towards improved Apgar scores and less resuscitation required in the intervention arm.
Comparably, Ram Mohan et al (2018) did not find any statistically different value for time to resuscitation or resuscitation interventions between the control and intervention groups. They used the same team for resuscitation and follow-up, introducing a strong potential source of bias, which may have affected the results positively or negatively dependent on how the collective team viewed the study and any bias they had for or against it.
Cohort studies
Cohort studies are observational studies and often used to understand causation links; they are valuable when an RCT might not be ethical or possible (Aveyard, 2014). Benefits can be financial and can include an easier ethical committee approval process owing to their non-interventional nature, as well as establishing links where it would have not been possible to undertake an RCT.
Blank et al (2018) and Lefebvre et al (2017) undertook feasibility cohort studies, both with specific aims. Although the sample size is similar in both studies, it is difficult to compare their designs as Lefebvre et al (2017) recorded a study length of 4 years whereas the study length of Blank et al (2018) is not recorded; this may be because Lefebvre et al (2017) recruited patients with a specific disease profile. Nevertheless, the outcome measures were similar with time to resuscitation recorded and Apgar score at 5 minutes documented.
Blank et al (2018) recorded data using a colorimetric device to indicate when pulmonary gas exchange had begun. This allowed them to standardise the intervention for participants. Video cameras placed on the machines strengthened data collection by recording exact timings. Lefebvre et al (2017) relied on human counting to record when intubation took place.
As all participants in the Lefebvre et al (2017) study had a congenital diaphragmatic hernia, they all received intubation as standard, so the two groups can still be compared on time to resuscitation. However, the data collection was subject to human error as the times were recorded predominantly by the researchers. As they were not blinded and were aware of whether each neonate was to receive intact cord resuscitation or not, there is a bias risk.
Other sources of bias in both cohort studies were selection bias and financial support, although Blank et al (2018) state the funders had no role in the study design, outcomes or publishing.
Baseline characteristics of both mothers and babies were similar in all groups and none were lost to follow-up. Because of the number of variables in treatment after intervention, both cohort studies used similar statistical tests, such as the Bonferroni significance test, to account for variables. Although Blank et al (2018) recorded time to first cry as an outcome, they did not statistically analyse that data. They found no significant difference between Apgar scores at 5 minutes between vigorous and non-vigorous neonates, demonstrating that UCM did not negatively impact resuscitation results.
| Study | Anup et al (2017) | Girish et al (2018) | Ram Mohan et al (2018) |
|---|---|---|---|
| Aim | Identify the benefit of resuscitation with intact umbilical cord | Feasibility and safety of UCM in neonates depressed at birth | Evaluate effect of UCM on short-term morbidity in preterm neonates requiring resuscitation |
| Study length | July 2016-Sept 2016 | Jan 2015-0ct 2016 | Feb 2015-Mar 2016 |
| Population | San Diego, California. Not stated | Two sites in India. 18000 deliveries a year | Bangalore, India. 542 premature births during study period |
| Intervention | Randomised to receive either <1 min or >5 minutes DCC | Quasi-randomised to receive UCM x3 or immediate cord clamping | Randomised to receive either UCM X 3 or no milking |
| Outcome | Safe to perform 5-minute DCC without compromising resuscitation | UCM is feasible for late preterm and term neonates and did not cause any significant delay to resuscitation | Can be used as a placental transfusion strategy with no adverse effect on resuscitation attempts |
| Results | |||
| Number of patients | 60 | 101 | 60 |
| Mean gestation | 39 weeks in both groups | 38.3 weeks | 33 weeks |
| Delivery room deaths | 0 | 0 | Not stated |
| Mean Apgar score at 5min (/IO) | Control: 8; DCC: 9 | 8 in both groups | 8 in both groups. |
| Mean time to resuscitation/first inflation breath | Control (1484min): 36s DCC (5 min): 25 s | Resuscitation started within 30 s in both groups. | Control: 60s UCM: 60s |
Abbreviations: DCC=delayed cord clamping; UCM=umbilical cord milking
Lefebvre et al (2017) found that, although time to intubation was shorter in the intact cord resuscitation group, it was not significantly different. Apgar score at 5 minutes, however, was significantly higher in the intact group. This has little generalisability to the wider population because the cohort all had a specific condition; however, the incidence of this disease is high (8% of all major neonatal congenital abnormalities) so the results are considered by the researchers as significant (Lefebvre et al, 2017).
Discussion
In relation to the research question of this review, placental transfusion does not appear to have a negative impact on neonatal resuscitation timing or efforts but, equally, has no significant effect on the Apgar score at 5 minutes; Apgar was used as a crude measure of infant mortality. The question remains around the proven multifaceted benefit of placental transfusion to these infants (Backes et al 2014; Mercer Erickson-Owens, 2014; Song et al, 2017; Chiruvolu et al, 2018) in the prehospital environment; therefore, further research should be carried out before making changes to practice for prehospital clinicians.
There has been a shift away from ‘scoop and run’ within the ambulance service; introducing placental transfusion may have a positive impact on clinicians doing the basics well before transporting to hospital. Basile et al (2019) have demonstrated in a meta-analysis that UCM has as much benefit as DCC so prehospital clinicians, first responders and midwives could still remove the neonate to a suitable platform for resuscitation while allowing the infant to benefit from placental transfusion by UCM which takes only 20 seconds (Basile et al, 2019). The term DCC can have negative connotations when used as part of a resuscitation strategy as it suggests ‘delay’; encouraging the use of ‘intact’ cord resuscitation instead may help promote a more positive culture around its use in this scenario.
The main reported barrier to placental transfusion considered in all five studies was a lack of appropriate equipment. This is likely to be similar for prehospital use of placental transfusion along with establishing enough space to start resuscitation. Different equipment was used in each of the five studies, so no comparison could be made; some used tailor-made resuscitation trolleys and some used only a radiant heater mattress. Difference in equipment is a variable in both space available to the clinicians and radiant heat available to the newborn. This is a significant limitation to the current review in that the specific equipment used is likely to have affected outcomes. As the kit used in hospital is very different to that used out of hospital, outcomes arising from equipment type could not be applied.
| Study | Blank et al (2018) | Lefebvre et al (2017) | |
|---|---|---|---|
| Aim | Feasibility of baby-directed DCC technique | Evaluate feasibility and safety of ICR on infants born with congenital diaphragmatic hernia | |
| Study length | Not stated | January 2012-April 2016. | |
| Population | Royal Women's hospital, Melbourne, Australia. 7 500 deliveries a year | Lille University hospital, Calais, France. Not stated. | |
| Cohort observations | Vigorous cohort received 2 min DCC. Non-vigorous cohort >60 s after colorimetric CO2 detector turned yellow | Cohort 1 received Immediate cord clamping before intubation. Cohort 2 received initial resuscitation including intubation with intact cord | |
| Outcome | Feasible to provide resuscitation during DCC. Clamping only when the infant is ready. | It is feasible to intubate and mechanically ventilate patients with an umbilical cord intact | |
| Results | |||
| Number of patients | 44 | 40 | |
| Mean gestation | 39 | ICC group 39. ICR group 38. | |
| Delivery room deaths | Not stated. | Not stated. | |
| Mean Apgar score at 5min (/10) | 9 in both groups | ICC group 6. ICR group 9. | |
| Mean time to resuscitation/first inflation breath | 60s | All patients underwent intubation as per guidelines for congenital diaphragmatic hernia ICC group 2.5 min; ICR group: 1.7 min | |
DCC: delayed cord clamping; ICC: immediate cord clamping ICR: intact cord resuscitation
Thomas et al (2014) conducted a trial using a new piece of equipment for in-hospital use that allowed bedside resuscitation. This mobile trolley was a miniature resuscitaire, which allowed an output of radiant heat to be brought to the mother's side, equivalent to that delivered by less mobile units, allowing for intact cord resuscitation. Heat and working conditions, particularly height, are important factors when considering using such equipment in the prehospital environment. The introduction of similar equipment with forward planning and collaboration between community midwives and ambulance services to address issues such as thermoregulation may increase the ability to perform neonatal resuscitation and decrease the risk of resuscitation being carried out on a kitchen or bathroom floor. Radiant heat mattresses could be considered and are already used by some advanced paramedics across the UK.
Bedside resuscitation in this way allows parents to witness resuscitation efforts, which has been proven to have a largely positive effect on the families’ coping and functioning after the event (Maxton, 2008). Bedside resuscitation with the cord intact would therefore facilitate parents to watch first responders perform the resuscitation, potentially limiting the distress felt when a newborn is immediately taken away to be resuscitated.
All papers analysed in the present review defined resuscitation similarly, using a non-crying or non-breathing neonate at birth as the criteria. All papers recorded Apgar at 5 minutes and found either no statistical difference between the intervention and control groups or an increase in Apgar with placental transfusion. As a result of their study, Anup et al (2017) and Blank et al (2018) believe that placental transfusion yielded a greater blood volume, which increased pulmonary circulation and cardiac output, leading to greater oxygen delivery and a need for less resuscitation effort. This corresponds with the practice of fluid resuscitation in severely depressed neonates, in which intravascular volume is increased. Fluid replacement in the form of UCM was therefore suggested by Girish et al (2018) to prevent brain injuries associated with reduced cerebral blood flow at birth when resuscitation with the cord intact was impractical.
Resuscitation Council UK (2015) guidelines are scheduled to be updated in 2020, and prehospital practice may change following a review of all the available evidence. It can be difficult to find strong evidence on which to base prehospital guidelines, so these often follow best hospital practice.
DCC and UCM have not been trialled in the prehospital environment, and challenging environmental factors may influence the suitability of this practice in the community. Although an RCT would allow for the highest grade of evidence, a cohort study may be a better way to evaluate prehospital placental transfusion because of the unpredictability of out-of-hospital neonatal resuscitation. Advanced practitioners, who are more likely to attend prehospital high-risk births and therefore be exposed to higher rates of neonatal resuscitation, could undertake this study and the initial introduction of the procedure. A balanced, proportionate view of the importance of the procedure should be taken, weighed against considerations such as neonatal thermoregulation and maternal management.
Ethical approval was gained in all studies included in this review. However, future studies may find it challenging to gain institutional agreement. Anup et al (2017) acknowledge it is unclear if neonates already in asystole would benefit, or whether it would contribute to increased foetal blood loss. This would be beneficial to study but would be invasive to undertake. Human factors influence the practice of ambulance clinicians and this patient group triggers a highly emotional reaction (McLelland et al, 2014). This may cause first responders to preemptively cut the umbilical cord in panic. UCM could be an alternative to intact cord resuscitation, especially in environments with little space. To promote placental transfusion among first responders, education would be needed and appropriate equipment (such as heat mattresses) considered. McLelland et al (2012) recommend the development of specific protocols in this field, which could be tailored into a flowchart to reduce stress and aid clinician decision making to facilitate use of the procedure when introduced.
Limitations
The many limitations of this review include having only one person searching the literature, which potentially leads to selection bias regarding papers chosen.
Researcher and clinician bias were evident in some of the studies and must be taken into consideration. The data available are sufficient to allow a meta-analysis but time, educational and financial constraints prevented this.
The studies were all conducted in hospitals with hospital equipment so are difficult to apply to the prehospital setting. The majority of the studies took place outside the UK, which limits their generalisability to UK practice. Babies born in developing countries who require resuscitation may have a different aetiology because of the health of the mothers and confounding factors such as socioeconomic wellbeing.
Conclusion
The current review identified five papers that promote the use of placental transfusion with no adverse effects on resuscitation attempts or outcomes. This demonstrates that there is evidence to suggest prehospital clinicians should be looking to change practice. Further research, considerations and consultations are required to ascertain the best way to implement these procedures in the prehospital environment.

