Chronic obstructive pulmonary disease (COPD), believed to be the fifth most common cause of death in the UK (National Clinical Guidelines Centre (NCGC), 2010), is a long-term and incurable lung condition. In the UK alone there are an estimated 3 million people (2-4% of the population) with COPD, up to two thirds of whom remain undiagnosed (NCGC, 2010). Its cost is significant; each year approximately 30 000 people die from COPD and it costs the UK £982 million (Britton, 2003).
Pathology and diagnosis of COPD
COPD, most often caused by smoking (NCGC, 2010; World Health Organization (WHO), 2011), has a complex pathology. The disease results in either hypertrophy of the mucus-secreting glands of the bronchial tree (in the case of bronchitis), or a destruction of the alveoli walls (in the case of emphysema) (Tortora and Derrickson, 2011). Often, however, both conditions coexist with one or other being the more dominant (Porth, 2005; Kumar and Clark, 2009). One of the key features of COPD is the progressive and irreversible nature of the condition (NCGC, 2010). A diagnosis of COPD is considered in individuals with certain risk factors who have signs and symptoms that are supported by spirometry (NCGC, 2010) (Table 1).
| Diagnosis of COPD considered in patients over the age of 35 who have a risk factor (generally smoking) and present with:
|
| Individual clinical signs are not helpful in making a diagnosis of COPD and in some patients there may be no abnormal physical signs. The following signs may be present:
|
| Where post bronchodilation the forced expiratory volume in one second (FEV1)/Forced Vital Capacity (FVC) is < 0.7 (i.e. 70%) and FEV1 < 80% predicted. |
Understanding the pathological changes of COPD requires a knowledge of the normal chemical control mechanism for respiration. In health, the stimulus to breath is triggered by either a slight rise in carbon dioxide (CO2) where the partial pressure of CO2 (PCO2) exceeds 40 mmgH, or when the partial pressure of oxygen (PO2) falls below 100 mmHg (Tortora and Derrickson, 2011).
The pathological changes of advanced COPD include a combination of mechanical compromise and impaired ventilation/perfusion (V/Q) matching. These changes lead to chronic retention of CO2 which, over time, results in the blunting of the CO2 chemoreceptors: they become desensitised to the high levels of CO2 (Porth, 2005). Individuals with COPD then come to rely only on hypoxaemia as a form of ‘back up’ breathing trigger (Porth, 2005; Tortora and Derrickson, 2011). In individuals with COPD, the balance of CO2 and O2 is therefore fragile. A relatively simple infection may lead to an acute exacerbation of their condition, the onset of acute respiratory failure and the inevitable ambulance call out.
Respiratory failure
Respiratory failure has been defined by British Thoracic Society (BTS) (2002) as a failure of the maintenance of adequate gas exchange and can be classified as either ‘Type I’ or ‘Type II’. Type I respiratory failure can occur in most pulmonary diseases. It occurs when the PO2 in arterial blood falls below 60 mmHg (8kPa) on air and is a consequence of insufficient oxygen for effective metabolism, CO2 levels are normal or slightly lower; here the patient is hypoxaemic (BTS, 2002). Type II respiratory failure occurs where the PCO2 in arterial blood exceeds 45 mmgH (6kPa) (BTS, 2002). The individual becomes hypercapnic as a consequence of the respiratory systems inability to remove CO2 quickly enough. Respiratory failure can be acute, chronic or acute on chronic. Table 2 demonstrates expected blood gas levels in each of these categories.
| Respiratory failure | Blood gases CO2 | HCO3 | pH | Explanation |
|---|---|---|---|---|
| Acute hypercapnic respiratory failure | High | Normal | Low | Low pH is due to a sudden rise in CO2 before HCO3 has been able to increase. Frequently seen in patients, with for example, opiate overdose and severe life-threating asthma |
| Chronic hypercapnic respiratory failure | High | High | Normal | This pattern would be expected in a patient with stable COPD where the kidneys have had time to produce enough HCO3 (the buffer) to ensure pH remains within normal parameters |
| Acute on chronic hypercapnic respiratory failure | High | High | Low | This pattern would be expected in a patient presenting with acute exacerbation of COPD (AECOPD) and would most likely require urgent medical intervention. An additional insult, such as infection, exacerbates the condition leading to worsening hypoxaemia. |
| NB. HCO3 is produced by the body to convert strong acids into weak acids and is an essential element used to counter the effects of acidosis (Tortora and Derickson, 2011). | ||||
‘Arterial blood gases should be measured in all individuals with severe COPD on arrival in the emergency department’
Acute on chronic respiratory failure can occur when an individual with Type II (hypercapnic) respiratory failure become acutely unwell secondary to, for example, a respiratory tract infection. As the body is already at its physiological limits of compensation, these individuals can rapidly deteriorate. Coma may occur where PCO2 rises to between 90-120 mmHg (12-16kPa) (O'Driscoll et al, 2008). Typical signs of CO2 retention include-vasodilation; bounding pulse; drowsiness; flapping tremor; confusion; and coma (O'Driscoll et al, 2008).
According to current guidance (NGCE, 2010) arterial blood gases should be measured in all individuals with severe COPD on arrival in the emergency department (ED). Arterial blood gas analysis enables the concentrations of the ‘buffer’ bicarbonate (HCO3), blood pH and PCO2 (BTS, 2002) to be measured and are useful in determining whether respiratory failure is acute, chronic or acute on chronic. These results will help determine a treatment strategy; particularly for those with Type II respiratory failure (O'Driscoll et al, 2008).
Prehospital treatment of acute exacerbation of COPD
Current prehospital treatments for patients with either ‘type’ of respiratory failure are guided by oxygen saturation level, patient condition and history (O'Driscoll et al, 2008; JRCALC, 2009). For those experiencing an acute exacerbation of COPD, the current guidelines recommend titrating oxygen therapy to maintain oxygen saturations between 88-92% (JRCALC, 2009; NCGC, 2010). Table 3 outlines key treatment recommendations during exacerbation. This controlled therapy is achieved via the use of venturi entrainment devices (Figure 1), or nasal cannula, and can be supplemented by nebulised bronchodilators such as P-agonists (salbutamol) and/or an antimuscarinics (ipratopium bromide) (JRCALC, 2006). However, it is the subgroup of patient, those with acute on chronic Type II respiratory failure, that are particularly vulnerable to the dangers of hyperoxygenation. Considerable care must therefore be taken to avoid hyperoxygenation during their treatment.
|
|

Hyperoxygenation in COPD
The potential for adverse effects as a result of hyper-oxygenation of individuals with COPD was described in the literature over half a century ago (Donald, 1949). In a letter to The Lancet Donald (1949) described the case of a male with severe emphysema who demonstrated significant hypercapnia and coma after treatment with prolonged oxygen therapy.
When oxygen therapy was discontinued, the patient made a full recovery. Donald (1949) explained that the patient's chemoreceptors had become desensitized to CO2 due to chronically elevated levels. This resulted in the respiratory center becoming reliant on hypoxaemia as a stimulus to breathe. When the patient was administered oxygen, the stimulus to breathe was removed resulting in hypercapnia, hypoventilation and coma.
Since 1949, the relationship between hypercapnea and hyperoxygenation in COPD has been attributed to a number of other mechanisms (O'Driscoll et al, 2008; Calverley, 2000). One of the most frequently described, and arguably most important, is hypoxic pulmonary vasoconstriction (HPV). HPV occurs in patients with COPD where chronic hypoxaemia triggers a degree of localized pulmonary vasoconstriction.
This compensatory mechanism maintains the V/Q ratio to ensure enough oxygen is available to saturate the pulmonary blood. When oxygen is administered to these patients, the pulmonary vessels dilate causing a drop in intravascular pressure. This creates a V/Q mismatch and an increase in dead air space, resulting in further hypercapnia, respiratory acidosis and a general deterioration of the patient's condition (Madison and Irwin, 1998).
In November 2010, 61 years after the case report by Donald (1949), the first randomized controlled trial measuring prehospital oxygen therapy in patients with an acute exacerbation of COPD was published (Austin et al, 2010). It concluded that, during an acute exacerbation of COPD, titrated oxygen treatment reduces mortality, hypercapnia and respiratory acidosis when compared to those receiving high flow oxygen.
Mortality was more than 50% greater (9% (21 deaths) compared to 4% (7 deaths)) in the high dose oxygen group, suggesting the ambulance clinicians may have been inadvertently killing with their care. Evidence of the danger of high flow oxygen was also demonstrated by Roberts et al (2011) who evidenced that high flow oxygen can significantly increase acidosis, the need for ventilator support and mortality in this patient group. Roberts et al (2011) demonstrated that high flow oxygen increases in-hospital mortality by almost 4% (11.1% vs 7.2%). While there continues to be discussion and debate over the relative importance of the physiological mechanisms, there can be little disagreement regarding the correlation between hyper-oxygenation and hypercapnia (O'Driscoll et al, 2008).
Clinical guideline update
Regardless of aetiology, the dangers of prehospital hyperoxygenation have been highlighted in a number of papers (Denniston et al, 2002; New, 2006; Gooptu et al, 2006; Hale et al, 2008; Austin et al, 2010). Evidence-based clinical guidelines have been developed to clarify the assessment and treatment of patients with COPD (JRCALC, 2006; O'Driscoll et al, 2008; JRCALC, 2009; NCGC, 2010). These national clinical guidelines make recommendations relating to all aspects of diagnosis and care but the elements that are of particular interest and relevance to prehospital care practitioners are those that relate to the treatment of patients with an acute exacerbation of COPD.
Earlier clinical guidelines recommended that such patients should receive supplementary oxygen therapy titrated to ensure an oxygen saturation of no greater than 93% or between 90-92% respectively (NICE, 2004; JRCALC, 2006). In 2008, the BTS guidelines on the emergency use of oxygen in ambulances, community and prehospital settings were published (O'Driscoll et al, 2008). In 2009, JRCALC adopted these guidelines recommending titrating oxygen levels to between 88-92%, or to a range already specified by a patient's respiratory service (JRCALC, 2009).
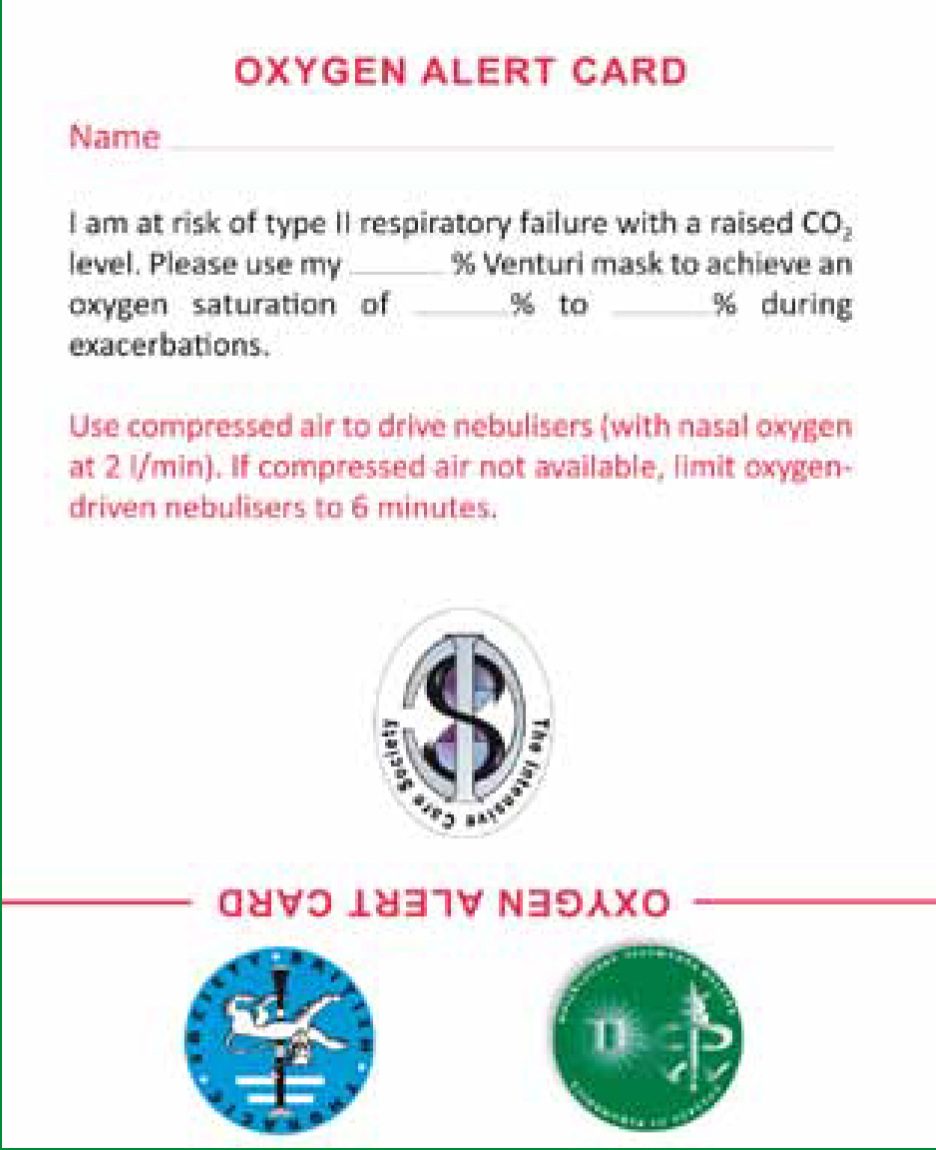
The most recent guidance from NCGC (2010) further emphasize an individualized approach to oxygen titration and mark another shift away from the earlier provision of a standard oxygen saturation level. It is now recommended that all patients receiving oxygen therapy have saturations that are maintained ‘within the individualized target range’ (NCGC, 2010) and are provided with an oxygen alert card. (Figure 2). However, adherence to guidelines is often poor. One recent study demonstrated only a 19.2% increase in adherence to COPD protocols post introduction (from 34.6 to 53.8%) (Bosse, 2011). While such guidance is intended to reduce the likelihood of prehospital hyper-oxygenation, several factors make implementation challenging in practice.
Availability of oxygen delivery equipment
Accurate titration of oxygen can only be achieved when suitable equipment is available. One recent study (Hale et al, 2008) examined the prehospital oxygen treatment for patients with COPD in an English ambulance service. They found that the mean oxygen flow rate for patients experiencing an acute exacerbation was >5 litres/min, delivering an oxygen concentration in excess of 40% (Hale et al, 2008). No patients received controlled oxygen therapy via a venturi entrainment device, which the authors stated may ‘lead to harmful outcomes’ (Hale et al, 2008).
The cause of hyperoxygenation was related to the lack of appropriate oxygen delivery equipment available to the ambulance clinicians within the study area. This is concerning as an earlier study demonstrated that the provision of venturi masks could reduce the number of COPD patients receiving high flow oxygen therapy (Durrington et al, 2005). However, provision of appropriate oxygen delivery equipment alone is insufficient; other factors also contribute to the hyperoxygenation of patients.
Lack of belief that oxygen is harmful
New (2005) suggests there may be a ‘mistrust’ by ambulance clinicians of the hypoxic drive theory and its association with COPD and states that excessive prehospital oxygen prescription stems in part from a poor understanding of the consequences and presentation of hypercapnia. It is possible that this mistrust partly explains the hyper-oxygenation of patients with COPD by ambulance clinicians (Denniston et al, 2002; Hale et al, 2008). Perhaps this is due to the fact that ambulance clinicians hand over their patients before the effects of hyperoxygenation become apparent, and do not observe the consequences of their actions.
Identification of patients with COPD and oxygen alert cards
If ambulance clinicians were provided with appropriate oxygen delivery equipment and received education reflecting current evidence, would this then solve the problem of hyper-oxygenation? The answer is, unfortunately, probably not. Why? because ambulance clinicians are not always able to identify patients with COPD and identifying patients with COPD can be challenging in the prehospital emergency environment (Denniston et al, 2002; Hale et al, 2008).
In one study, ambulance clinicians identified only 32% of COPD patients correctly (Denniston et al, 2002) and in another, a slightly more encouraging 58% of cases (Hale et al, 2008). There is some evidence too that the practice of hyperoxygenation continues into the emergency department, after hand-over. Joosten et al (2007) demonstrated that 80% of patients received oxygen therapy in excess of 2 litres/minute after admission to the emergency department.
One soloution is to distribute oxygen alert cards to high risk COPD patients (O'Driscoll et al, 2008). In addition to providing detail on normal oxygen saturation levels, the cards should also include information recommending that when nebulization occurs, it should be limited to 6 minutes when using an oxygen driven nebulizer unit. This reduces the risk of hypercapnic respiratory failure but enables most of the drug dose to be delivered. However, the issuing of these cards is not mandatory and their distribution and usage in the UK is unknown. Two studies have looked at the effectiveness of oxygen alert cards (Wolstenholme et al, 2003; Gooptu et al, 2006). Wolstenholme et al (2003) found the oxygen alert card system to be relatively ineffective; only 26% of patients (n=5) presented their card to the health care professional during treatment.
Gooptu et al (2006) demonstrated that even when they were presented to ambulance clinicians, they were only moderately successful in achieving their aim; only 62% of patients (n=33) were managed by ambulance clinicians according to the guidance provided on the card. The oxygen alert card system is therefore, at best, only part of the solution—card-based systems alone do not resolve the problem of prehospital hyperoxygenation. When they are used, it is suggested that both patient and staff education be incorporated as an essential element of the intervention (Wolstenholme et al, 2003).
A multi-modal solution?
It is clear that all prehospital care and emergency department practitioners would benefit from knowing which patients have COPD and are therefore at risk of poor clinical outcome from hyperoxygenation. As card-based systems alone appear insufficient in achieving this, other solutions need to be developed and evaluated. O'Driscoll, Howard and Davison (2008) recommend that a multidisciplinary and multimodal oxygen alert system is implemented to share patient specific information between respiratory specialists and prehospital care personnel. This system should include:
With the exception of the alert cards, whose limitations have already been discussed, these recommendations are based on ‘Level D’ evidence; that is, evidence from expert committee reports or opinions and/or clinical experience of respected authorities. Furthermore, the recommended system focuses on patients with known hypercapnic reparatory failure—individuals who have already been hyperoxygenated and experienced ill-effects—they do nothing to protect vulnerable but previously undetected individuals.
It seems sensible to expand the criteria to include all patients who present to ambulance clinicians with COPD. It also remains the case that the effectiveness of this system remains unknown. Would such a system result in significantly more patients with COPD being identified and appropriately treated in the prehospital emergency setting? The answer is, we do not know. Rigorous high quality implementation research is therefore urgently required to evaluate this system in practice.
Conclusion and recommendations
COPD is a long-term, incurable lung condition, and ambulance clinicians frequently deal with its acute exacerbations in the prehospital environment. Patients are dying or experiencing increased length of stay in hospital as a result of difficulty in identifying and delivering optimal oxygenation.
To overcome these issues, ambulance services and clinicians need to ensure appropriate oxygen delivery equipment is available to treat this vulnerable group. While there is a need to ensure that ambulance clinicians receive education on best practice for patients with COPD, education alone is unlikely to be sufficient to facilitate a change in practice. Additional methods for the sharing of individualised patient information should also be sought to ensure that ambulance clinicians receive vital clinical information. This article has outlined one such method, the multimodal oxygen alert system. This aims to ensure high risk COPD patients receive appropriate concentrations of oxygen from the earliest point in their care.
Robust evidence to support the effectiveness of this system is lacking and an evaluation of this intervention is now urgently required. Until effective methods of communicating individualized patient information are implemented nationally, there is an ongoing danger that ambulance clinicians may continue to unintentionally kill with care. This article has several focused recommendations for clinical practice and further research:
