LEARNING OUTCOMES
After completing this module, the paramedic will be able to:
Despite the many milestones achieved in modern medicine, the pathophysiology of many rashes remains unknown. The anatomy and physiology of the skin offer a foundation from which to draw understanding about what is actually happening within the dermal layers (Marieb and Hoehn, 2015). The integumentary system includes the hair, skin, and nails, each having a variety of functions to protect internal layers, provide a waterproof covering, regulate temperature and provide sensory function. An anatomical understanding of this system is an important, but seemingly overlooked, part of paramedic education. While outside the scope of this introductory CPD article, an awareness of the pathophysical responses within this system would greatly assist the reader.
History-taking
An accurate evaluation of dermatological complaints can only be made in the context of a thorough history (McKay, 1990). When taking a social history, it is good practice to ask about the patient's occupation, their recent movements and any recent foreign travel—all of which may suggest exposure to known occupational, geographic or parasitic risks. Contact with water, especially hot tubs, may indicate a fungal aetiology, while ingestion of plants or medicated drugs could indicate a systemic reaction. Pay close attention to a patient who complains of an itching sensation but has no presenting rash as further tests are often required—these may be to diagnose potential hepatic issues or malignant conditions.
Age and skin
Age is also an important consideration. The immature physical developmental stage of an infant's skin tells us that they are not as efficient at heat regulation as their parents. This means that the alarming rash that occurred when a child was in the bath will have subsequently disappeared by the time the worried parent presents them to you (Foster et al, 1969). With age, the dermal (especially subcutaneous) layers, become thinner and are therefore prone to dryness, flakiness and a longer healing time (Farage et al, 2013).
Physical examination
A thorough physical examination should focus on the appearance of the rash, the distribution across the body, the symmetry and any excoriation marks that will have indicated pruritus (itching) (Onselen, 2016). This should also help to ensure that any associated features are quickly identified, and determine if the rash is a primary problem, a secondary reaction to an allergen, or a sign of a more sinister systemic disease.
Describing the rash
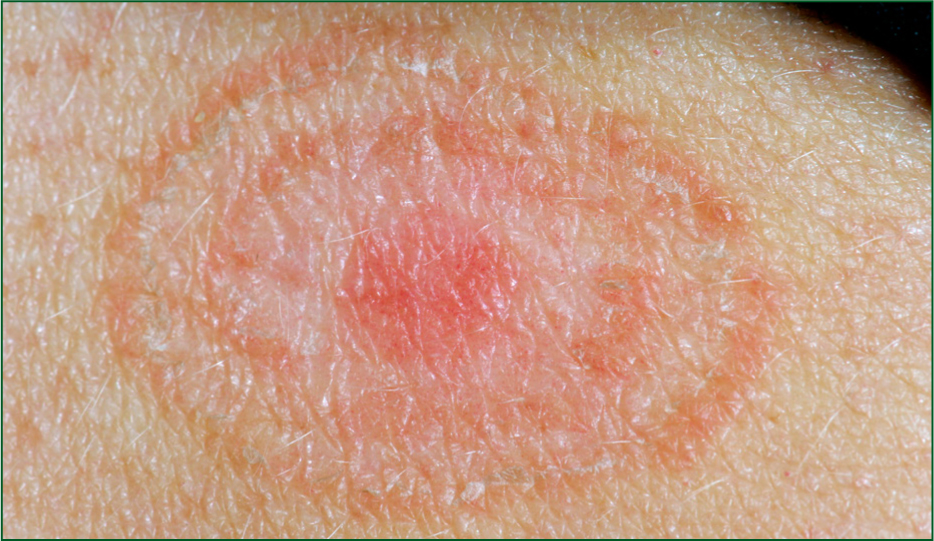
The diagnostic terms of most skin conditions describe the appearance, history and location of the rash (Onselen, 2016). For example, dermatitis (Figure 1) is a term used to describe inflammation of the dermis and therefore broadly describes an inflammatory skin reaction. Used with other terminology, such as seborrhoea, it can describe a specific condition, such as seborrhoeic dermatitis. Seborrhoea describes an overactivity of the sebaceous glands, which result in an oily coating, crusts, or scales on the skin. Together, the term seborrheic dermatitis relates commonly to scalp presentations which are very itchy and present with scaly dry deposits. Exanthema (meaning to break out) is another term commonly used to describe skin conditions and relates to any eruption or rash that is present on the skin—just like chicken pox (Figure 2). However, describing a rash alone is not the same as reaching a diagnosis. Box 1 outlines the basic descriptive terminology for rashes that may be used during the reflective CPD activities within the current article.


Case study 1
You respond to a 999 call to attend to an elderly male who had a mechanical fall at home several hours ago. He was found in the bathroom by his daughter who managed to assist him with a walking frame back to his favourite chair. The frame and rubber ferrules of the walker are in good condition and he has new slippers which give adequate support. The house is warm and tidy with no trip hazards. His daughter states he has been struggling with everyday tasks over the last 7 days as his hands have been sore. He has been unable to get an appointment to see his general practitioner (GP), although there are two large packages of medications unopened on the kitchen table. The patient declares they do not work well so he does not take them.
On examination
Head-to-toe examination shows no major bruising, wounds, nor deformity. His skin is very erythematous and dry on his finger webs as well as over his trunk, with signs of scratching (excoriation) (Figure 3). The neck, wrists, elbow and knee folds show greater inflammation. There are no open wounds. His skin demonstrates poor hydration with a slightly reduced skin turgor, but maintains regular urine volumes.

Eczema
Given the drug history, it is fairly apparent that this patient is not complying with medication prescribed for his eczema. Emollients are an incredibly safe and effective treatment option for those who have eczema (National Institute for Health and Care Excellence (NICE), 2018a). Coupled with a good skincare routine, using emollients can soothe, moisturise and protect the skin, helping to reduce the number of eczema flares—which this patient is experiencing.
Patients often do not apply enough emollient, and so find it does not work. Hydrocortisone 1% is often prescribed in addition to emollients to help reduce inflammation (NICE, 2018b). It should be applied sparingly twice a day, avoiding application to open wounds and around the eyes where the skin is thinnest. Antihistamines are ideal for reducing mast cell reactions in the skin and thus reduce itching (NICE, 2018c)—one of the biggest treatment goals for people with eczema is to stop scratching (National Eczema Society, 2018).
Case study 2
You have been called to a 50-year-old female who has known diabetes. Her husband is well rehearsed in managing her hypoglycaemic events and, as you arrive on scene, she is responding to the buccal glucose gel given by her husband. She was reviewed 3 months ago by the diabetes nurse specialist but has not seen her GP since then. Once alert and fully orientated, she also complains of a rash underneath her breasts and groin area.
On examination
Examination of breast and groin reveals an erythematous asymmetrical rash with no open lesions evident. It is present along the mammary folds of her breasts with a reflected pattern seen on the trunk (Figure 4). A similar rash is identified in the inguinal folds of the abdomen, thighs and buttocks. Smaller isolated circular patches of approximately 3 cm in diameter are evident on the forearms; they are slightly raised with a clearly defined silver border, and scaly in appearance. She states that these rashes have been present for several weeks now and are not resolving.
Ringworm (Tinea corporis)
There is little evidence on the best way to treat patients with multiple sites of ringworm. This patient demonstrates an extensive version of the disease, with tinea corporis (arms or legs), tinea cruris (groin, inner thighs, or buttocks), and tinea pedis (feet) (Sahoo and Mahajan, 2016). This is often called ‘ringworm’ due to the itchy, red rash—and is a fungus but nothing to do with worms! While a topical antifungal cream often presents the first line of treatment for a mild form of the disease, more extensive forms require oral antifungals (NICE, 2018d). Generally, fungal infections can take weeks to months to improve, and it is important to assess the impact of the rash on the person's overall wellbeing.
Case study 3
A 6-year-old female has been seen by the out-of-hours (OOH) clinician with her worried mother 3 days ago, and presents to you in the GP practice. The clinical notes state that the child previously had a pyrexia of 39oC and had been complaining of sore throat symptoms for the past 5 days. The mother has been giving regular doses of paracetamol and ibuprofen and the OOH record states that the child was alert, well perfused and well hydrated. Her CENTOR score was 4/5, and so oral Penicillin V was started. The mother was advised to see their own practice if there were any further concerns. Since this appointment, the patient has developed an erythematous, non-pruritic rash which has progressed proximally from both feet to thighs (Figure 5) and upper extremities including palms and soles. She had a restless night last night due to right ear pain, and today, mum has noted that her feet have become swollen. She also has a new onset of generalised abdominal pain.

On examination
Henoch-Schönlein Purpura
Paramedics may most often associate purpura with a clinically unwell child, and a sign of meningitis (Brown et al, 2016). This is quite correct, but the child in this case study presents as clinically well. This is Henoch-Schönlein Purpura (HSP). Many children with HSP initially present clinically well with a purpuric rash, but observations and further investigations will reveal that, systemically, they are showing signs of decline and haemorrhage (McCarthy and Tizard, 2010).
In this scenario, the initial management is an urgent referral to the paediatric specialist in a nearby receiving hospital. This common childhood vasculitis manifests across numerous organ systems, including glomerulonephritis. Patients with more severe HSP-associated glomerulonephritis may develop chronic renal failure, and it is important that this is found and rectified as soon as possible (Flynn et al, 2001). Ongoing management of such cases is usually achieved in primary care and generally involves regular urinalysis to monitor any ongoing haematuria, as well as regular blood pressure assessments.
Case study 4
Anxious parents had initially called 111 for advice regarding a rash on their 3-week-old baby girl. They had been waiting for a call back from the duty doctor but have now decided to attend the local walk-in centre because the baby seems to be less responsive.
On their arrival, the baby is wrapped in a blanket as well as a vest and baby grow. Mum states she was not initially concerned about some small spots which had appeared around the nose several days ago, but these have now multiplied and spread to the cheeks, forehead and around the eyes (Figure 6). The baby had not fed as much today, which has added to her mother's anxiety and fear that something is wrong.

On examination
Further history obtained advises gravida 4 para 1 conceived by in vitro fertilisation (IVF) and baby was born at 41 weeks via normal vaginal delivery.
Millia
Eccrine glands are responsible for sweat production. Because of their immaturity, eccrine glands in an infant respond at higher temperatures compared with adults. As a result, the infant has a reduced ability to sweat, and becomes prone to overheating (Foster et al, 1969). This can account for a relatively high temperature in a neonate, as babies are small, and there is an increased skin surface area in relation to body mass. Eccrine glands are closer together and function irregularly, hence overheating.
Milk spots, or milia, are tiny pearly white spots that occur around the eyes, nose, cheeks and forehead. More specifically, they're sealed, seed-like sacs under the skin filled with keratin (a protein) (Primary Care Dermatological Society, 2018). They're common, harmless and should disappear after baby's first few weeks. While they might look sore, they are not itchy, nor do they cause discomfort. While they look like whiteheads, they cannot be squeezed as there is no pore to release the keratin, so this will break the skin and lead to scaring and infection. Treatment is simply a gentle cleanse with water or a mild baby wash, and it will self-resolve. Reassuring the parents, ruling out any systemic infection or illness, and providing clear advice in the case that it worsens, is fundamental for any child with a temperature.
Conclusion
Characteristics of a rash can indicate much of its aetiology, and careful attention to a person's history may also yield an accurate diagnosis. While the diagnostic name may not be familiar to paramedics new to this area, clearly recording the presentation and associated symptoms of the rash is fundamental.
Treatment for many rashes is simple, following a guided treatment plan (such as the NICE Clinical Knowledge Summaries (CKS))—however, it is important to be aware of the sinister causes of rashes and be able to notice and manage critical presentations.

