Psoriasis is estimated to affect around 2.2% of the UK population and can transpire at any age; therefore, identifying the most effective treatment for the disease is paramount (National Institute for Health and Care Excellence (NICE), 2012). This article will endeavour to demonstrate strategic awareness of the policy drivers within health care and current legislature that have influenced the decisions on the treatment of psoriasis. With the growing responsibility for paramedics to discharge on scene, the increasing volume of primary care type calls to the ambulance service, and the minimal amount taught to undergraduate paramedics concerning dermatology, there is a greater need for rashes to be recognised in the pre-hospital setting. In particular, knowing when referral is necessary and how quickly this is required. Furthermore, for many people, psoriasis can result in functional, psychological and social morbidity, consequently having a huge impact on daily life (Basavaraj et al, 2011). This suggests the importance of determining which treatment option is best, although this can be extremely difficult. Additionally, one study has reported that individuals who suffer with severe psoriasis are at an increased risk of developing cardiovascular disease from the age of 20 years, further fortifying the need for adequate treatment (Parsi et al, 2012).
Pathophysiology
Psoriasis is a chronic inflammatory skin disease that is considered to have a genetic influence; however, Raychaudhuri (2013) suggests that the aetiology of psoriasis remains unknown, and that only a fraction of cases can be attributed to a genetic predisposition. Moreover, Ghazizadeh et al (2010) advise that research is still ongoing to determine the predisposing factors to the disease. This suggests that the environment and immunological factors can also play a part in the onset of psoriasis.
Psoriasis typically follows a relapsing and remitting course, and results from the abnormal activation of T cells and associated increase in cytokines in affected tissues. This then leads to excessive multiplication of keratinocytes producing the symptoms of the disease. This amplified rate of cellular proliferation leads to thickening of the dermis and epidermis, resulting in lesions beginning as small red papules that enlarge. A silvery plaque then develops but it still remains erythematous due to the inflammation and vasodilation.
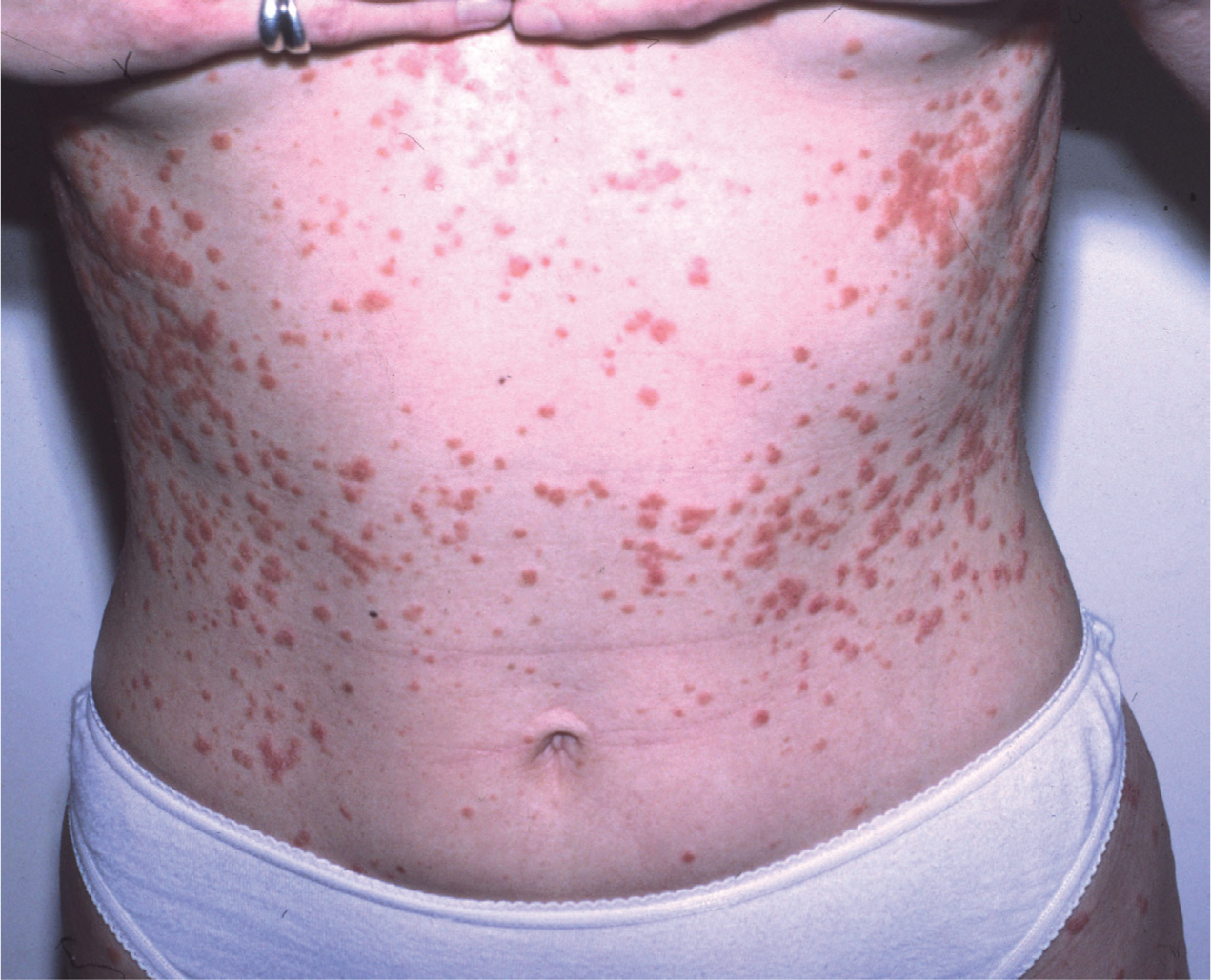
The lesions are most commonly found on the face, scalp, knees and elbows and will most likely produce a burning and itchy sensation (Gould and Dyer, 2011). There are different types of psoriasis, including plaque psoriasis (Figure 1), guttate psoriasis (Figure 2) and pustular psoriasis (Figure 3). Guttate psoriasis affects around 10% of all people who get the disease and is more common in childhood after getting a streptococcus infection, and appears as small dot-like lesions. Pustular psoriasis is characterised by white non-infectious and non-contagious pustules surrounded by red skin, most commonly found on the hands and feet. Plaque psoriasis is by far the most common type of the disease, making up 90% of all cases of the disease. For this reason, plaque psoriasis will be the type discussed within this article. Plaque psoriasis is characterised by an erythematous lesion with a build-up of silvery plaque of dead skin.


Treatment options
There are a considerable amount of treatment options available for psoriasis, and Murphy and Reich (2011) suggest that there is a substantial variance in practice in primary care, particularly concerning when a patient with psoriasis should be referred, appropriate drug monitoring and specialist nurse support. Mrowietz et al (2011) support this and identified from their study that psoriasis is undertreated. This suggests that due to practice being so varied, guidelines on treatment are lacking.
However, NICE (2012) offers a guideline to facilitate the delivery of high-quality health care and improve outcomes to the people who suffer with psoriasis. Some treatments are very expensive, of which some can only be accessed in specialist care, and all must be carefully monitored. For most people, psoriasis can be managed within primary care; however, specialist referral is required at some point for 60% of sufferers. Moreover, specialist tertiary care is required in a small minority of complex cases that are treatment resistant or have rare complications (Gould and Dyer, 2011). The NICE guidance (2012) for the treatment of psoriasis advocates a stepwise approach to treatment. NICE (2012) use randomised controlled trials (RCTs) for the evidence behind their guidance, making it very reliable. However, it can be argued that observational studies have an important role on measuring the long-term effectiveness in a more naturalistic environment. Therefore, it can be suggested that observational studies are advantageous in the treatment of psoriasis due to the severe psychological factors the disease can cause. Thus, both observational studies and RCTs will be used as evidence for this critical appraisal, and therefore identify the best treatment options for psoriasis.
Topical therapies
The first line of treatment used for psoriasis involves topical therapies, such as corticosteroids, Vitamin D analogues, dithranol and tar preparations. Topical therapies work using a variety of different mechanisms of action, including anti-inflammatory, cellular differentiation, immunosuppressive and antiproliferative effects.
It can be suggested that the long-term use of topical therapies, particularly corticosteroids, can develop cutaneous side effects, such as striae (Murphy and Reich, 2011). Although these side effects are not systemic, they can still result in psychological distress.
Additionally, Kragballe et al (2013) suggest that the efficacy of corticosteroids reduces over long-term use, and for this reason they are not commonly used long term. Contrary to this, the use of corticosteroids in the treatment of psoriasis has been proved to be clinically effective for mild to moderate psoriasis. This is apparent from one Cochrane review that compared the efficacy of a variety of topical therapies in the treatment of psoriasis with placebo. This review consisted of 131 randomised controlled trials that involved 21 488 participants (Mason et al, 2013). Of the multiple therapies examined in this study, Vitamin D analogues and corticosteroids showed the greatest efficacy, proving to be significantly better than placebo for the treatment of mild to moderate psoriasis. Furthermore, both corticosteroids and Vitamin D analogues were found to be equally effective; however, when they are used simultaneously, this proved to have the best results of all. Both Vitamin D analogues and corticosteroids were proved to be more effective than tar preparations and dithranol. Therefore, this study suggests a combination of Vitamin D analogue and corticosteroid is the best treatment for mild to moderate psoriasis.
Arguably, Kurian and Barankin (2011) propose that the Cochrane review has not taken into consideration patient choice. This suggests that patients may not adhere to the topical treatment given. Devaux et al (2012) agree and suggest that further clinical studies need to be completed, incorporating quality of life impact, to therefore enhance adherence to topical therapies, resulting in optimal management. This suggests that in order to measure the effectiveness of corticosteroids and Vitamin D analogues in the treatment of mild to moderate psoriasis, it may be necessary to mirror a real-world environment using an observational study. This will then increase external validity and identify patient adherence to the treatment.
Furthermore, as Kurian and Barankin (2011) propose, education of the disease to the patient is pivotal to ensure therapeutic success, as this is likely to increase patient adherence to treatment. Further to this point, Kurian and Brankin (2011) also suggest that having a greater understanding of the disease will motivate the patient to adhere to treatment. From all of this evidence, it can be suggested that the use of corticosteroids and Vitamin D analogues for the treatment of mild to moderate psoriasis is very promising. They provide a more cosmetic and efficient option compared to the previously used coal tar. However, it is clear that patient adherence is key to its success. Finally, another influencing factor for the use of corticosteroids and Vitamin D analogues for first-line therapy is that it is the most cost-effective treatment (Sawyer et al, 2013). Therefore, this suggests that this first-line treatment is both beneficial to the patient and the NHS, which is extremely important in the current climate.
Phototherapy, non-biological and biological treatment
For patients who suffer with moderate to severe psoriasis and require referral to a dermatologist, NICE (2012) advise a second line of treatment. This second line of treatment includes phototherapy and systemic non-biological therapies. Phototherapy includes broad or narrow band ultraviolet B light and psoralen plus UVA light (NICE, 2012).
Gelfand et al (2012) conducted a cross-sectional study comparing the effectiveness of commonly used phototherapy and non-biological therapies in the treatment of moderate to severe psoriasis. They identified that those receiving phototherapy showed no significant difference to those receiving methotrexate, and although there is a small benefit of methotrexate on clearing the skin, it may not be clinically significant. This suggests that the effectiveness of psoriasis therapies may be lower than what has been reported in previous clinical trials.
Arguably, Mudiganda et al (2011) write that UVB phototherapy can provide localised treatment without damaging the surrounding skin, and should be considered for second-line treatment of moderately severe psoriasis. Moreover, Menter et al (2009) suggest that traditional oral therapies such as methotrexate, acitretin and ciclosporin are extremely limited by patient intolerance, in addition to their toxic effects on organs with long-term use.
Rácz et al (2011) continue to advocate the use of phototherapy for the treatment of moderate to severe psoriasis, as their study identified that it repressed the Th17, type 1 and type 2 IFN signalling pathways which are critical in the pathogenesis of the disease.
Despite this, phototherapy has been shown to have adverse effects, including hyperpigmentation, blisters, burning and itching of the skin (Mudiganda et al, 2011). From analysing the literature, it appears that there is no significant evidence to determine which therapies are second-line and which are third-line treatment. This again suggests that there is a lack of guidance for healthcare professionals to determine the course of treatment for moderate to severe psoriasis, whereas it appears clear what is most beneficial for first-line treatment in mild psoriasis.
The treatment of severe psoriasis using third-line therapy has revolutionised in recent times with the approved administration of systemic biological therapies such as the tumour necrosis factor antagonists adalimumab and infliximab (NICE, 2012). Additionally, the more recent monoclonal antibody ustekinumab targets cytokines critical to the pathogenesis of psoriasis (NICE, 2012). These drugs should be used when there has been no response to non-biological drugs such as methotrexate (NICE, 2012). They have proved to be effective in the treatment of severe psoriasis in short-term studies, but they are very costly and have diminished effects with long term treatment (Gelfand et al, 2012). Mrowietz et al (2011) further suggest that dermatologists are often reluctant to administer the systemic biological therapies due to some reported extreme adverse effects. Reich et al (2012) support this and state that research is still ongoing, as risks of rare but serious adverse reactions are still being recognised.
As Gelfand et al (2012) compared non-biological treatments with biological treatments, it can be identified that the biological treatments, such as ustekinumab, proved to produce better results than the non-biological treatments, such as methotrexate.
Mrawietz et al (2010) suggest that treatment for psoriasis is very personal to the patient and can affect each individual differently. This suggests that it may be a case of trying different options to determine which treatment is most beneficial for that particular individual. Additionally, it emphasises the requirement of conducting further studies within a real-world environment. This is made clear when looking at the results from the CHAMPION trial, where the effectiveness of systemic biological therapies were found to be significantly higher than that identified within the real-world setting (Saurat et al, 2008). Despite it being an RCT, the rate of being clear of psoriasis was found to be much higher than in the cross sectional study conducted by Gelfand et al (2012) when using biological therapy.
Comparatively, Navinni et al (2014) also found that adalimumab therapy resulted in resolution of individual body regions of psoriasis, which was double that of methotrexate, showing similar results to the CHAMPION trial—both of which are RCTs. This suggests that it is critical to evaluate the effects of the therapies within real-world circumstances, and that there is a clear gap in comparative effectiveness research.
Barker et al (2011) identified from their randomised controlled trial that infliximab is extremely effective in the treatment of psoriasis compared to methotrexate, again suggesting that systemic biological treatment is more favourable. Therefore, it can be questioned why infliximab is not administered immediately, but this is likely due to cost-effective reasons as they are very expensive to the NHS (Sawyer et al, 2014).
As there are several different biological treatments existing for psoriasis it can be questioned which is best to use. One meta-analysis by Reich et al (2012) compared all of the different available biological agents to identify which is best to aid with the decision-making. Comparative effectiveness was made using the Psoriasis Area and Severity Index (PASI), where the study identified infliximab to have the best response. However, it can be argued that treatment for psoriasis is very personal to the patient, as Gelfand (2012) identified that there is a wide variety of results to different treatments.
Cardiovasular co-morbidities and psychological problems
Patients who have moderate to severe psoriasis are at a greater risk of developing cardiovascular co-morbidities and developing psychological problems, so even further treatment may be required (Ghazizadeh et al, 2010). Additionally, some of the treatments that are given for psoriasis can further increase the risk of cardiovascular disease (CVD) (Hugh et al, 2014). It has been identified that both methotrexate and phototherapy have beneficial impacts on CVD and are associated with a decreased morbidity and mortality. However, some authorities remain concerned about the effects of biological therapies such as ustekinumab (Hugh et al, 2014).
This suggests that clinical follow-up is essential for the patients who take these drugs for their psoriasis, in addition to further research being carried out. It is believed that the link between psoriasis and CVD is secretion of chemokines and cytokines that contribute to the inflammatory environment, resulting in the formation of atherosclerotic plaque (Zhou et al, 2009). This is supported by Ghazizadeh et al (2010), who advise that additional treatment of hyperlipidaemia improved the overall condition of the psoriasis. This suggests that both treatment and preventative strategies to reduce cholesterol and suppress inflammation improve both psoriasis and risk of CVD.
Ghazizadeh et al (2011) agree and suggest that drugs to treat hyperlipidaemia should be given additionally for the treatment of moderate to severe psoriasis, where they are at a greater risk of CVD. The authors go on to say that treatment with statins indicated a clinical improvement in the psoriatic condition, where the mechanism can be attributed to immunomodulatory and anti-inflammatory effects. A study by Maradit-Kremers et al (2013) found that there was no association between CVD and psoriasis. This suggests that the evidence is controversial and uncertainty still remains to whether CVD disease can be directly attributed to psoriasis. Moreover, as most studies have not adjusted for fundamental risk factors in psoriasis, this could affect the results.
As mentioned above, psoriasis also has a considerable psychological impact on sufferers. Basavaraj et al (2011) identified that 5.5% of patients are suicidal due to the condition, 51% feel depressed and 90% felt increased levels of stress. This then leads to a vicious circle as stress acts as a trigger and can then worsen the psoriasis. Treatments are then also needed for stress which often involves counselling, meditation, yoga, and self-help approaches (Basavaraj et al, 2011).
Kimball et al (2010) suggest that the psychological burden of psoriasis is poorly understood, compared to other chronic diseases. A study by Mattei et al (2013) showed a substantial increase in quality of life for patients taking systemic biological treatments for severe psoriasis as lesions decreased. This suggests that vulnerable patients need to be recognised quickly and referred for more appropriate treatment. Moreover, specialist referral should be considered where needed.
Conclusions
Despite the growing options of treatment for psoriasis, it still remains unclear what treatment should be given for moderate to severe psoriasis. Although certain treatments have proved to be efficacious in the short term, they are associated with high costs and risks of adverse reactions. Vitamin D analogues and corticosteroids have proved to provide encouraging treatment in mild psoriasis, and have replaced traditional therapy such as coal tar. More research is required to evaluate the effectiveness of second- and third-line therapies in the real-world setting.
It remains unclear whether statins are beneficial as an additional treatment for moderate to severe psoriasis, as there is a potential that psoriasis is linked to atherosclerosis; however, this is controversial as it is not clear whether this is independent of traditional risk factors. Additionally, more needs to done for the psychological well-being of patients who suffer with psoriasis, although with the advances in treatment of systemic biological treatment, improvements are being observed. Paramedics should be more conscious of the potential cardiovascular effects that psoriasis can have, therefore it may be necessary to do further checks, such as blood pressure and ECG, before discharge. Additionally, it is important for paramedics to recognise the importance of health promotion in patients who suffer with psoriasis, to reduce mortality rates. Health education is also key, and as a paramedic, it may be beneficial to ensure the patient is adhering to their treatment and explaining the importance of this. Finally, paramedics should be aware of the psychological effects that psoriasis may have and look for signs of this, arranging referral if necessary.

