From 1978 to 2008, the published survival rate of patients with out-of-hospital cardiac arrest (OHCA) averaged 7.6%. This has remained unchanged over the past three decades, despite recurring updates of resuscitation guidelines (Sasson et al, 2010).
As most patients with OHCA have little or no chance of survival, a better way of analyzing the effectiveness of one's response to OHCA is to focus on the subset of patients with a reasonable chance of survival—those with ventricular fibrillation (VF). However, even when this subset of patients is analyzed, the reported survival rate, while better (averaging 17.7% between 1980 and 2003 in the US), was also unchanged over the 23 year period— despite regular updates of the guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiac care (ECC) (Rea et al, 2004). The reported survival of VF arrests in Europe between 1980 and 2004 was 21% (Figure 1) (Atwood et al, 2005).
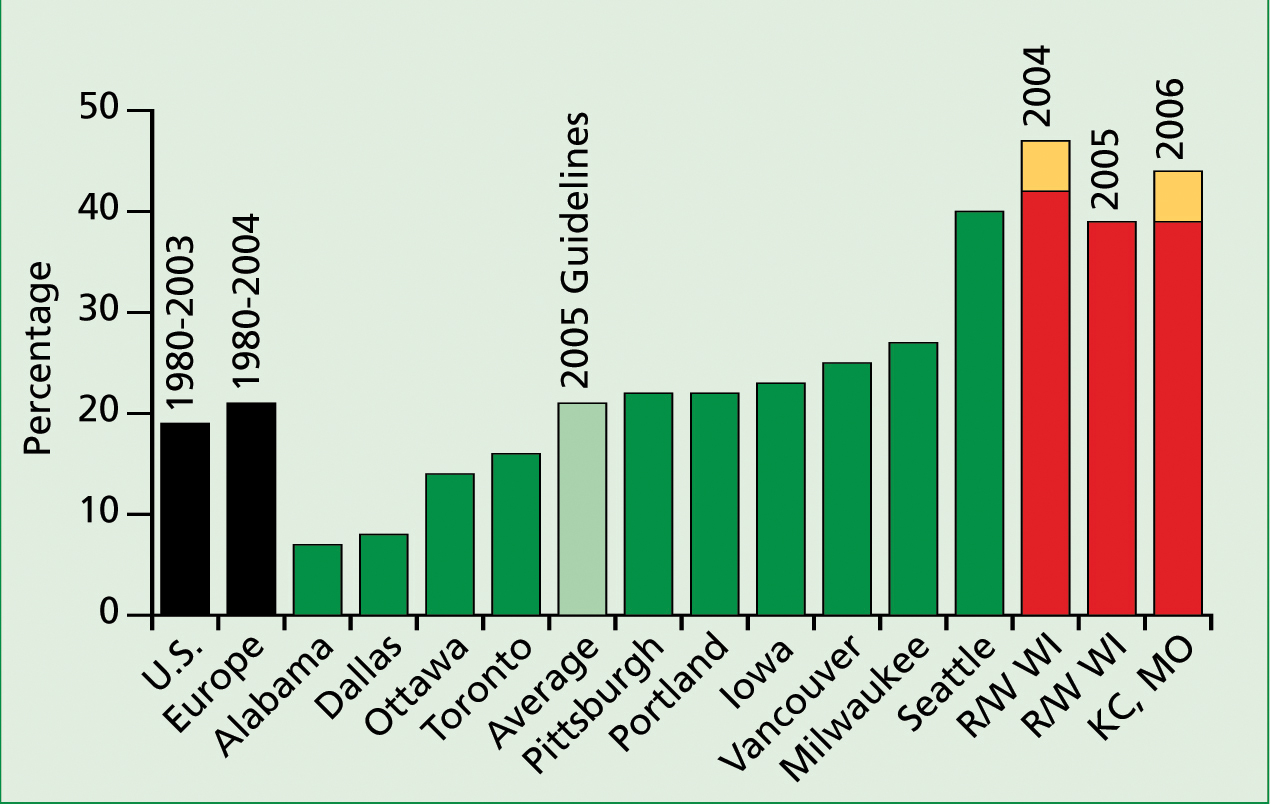
There is also marked variation in the survival of patients with OHCA depending on location. In a report where emergency medical systems (EMS) followed the 2005 American Heart Association (AHA) and the International Liaison Committee on Resuscitation (ILCOR) guidelines, survival of patients with OHCA with VF varied from 7.7% to 39.9% (Figure 1) (Nichols and Zawada, 2008). Such reports indicate that ‘one size does not fit all.’
The previous and current AHA resuscitation guidelines may be appropriate in the few locations that have a high rate of bystander CPR and a short EMS response time, such as in Seattle, Washington (Figure 1) (Becker et al, 2008). Unfortunately, survival rates have not improved in many other areas following periodically updated guidelines for CPR and ECC. This could be, in part, because of the low prevalence of bystander CPR and the prolonged arrival times of EMS. It could also be due to prolonged periods where patients with cardiac arrest were not receiving chest compressions and therefore not getting perfusion to vital organs (Valenzuela et al, 2005; Wik et al, 2005).
A non-guidelines approach might improve survival
Decades of research in our experimental animal resuscitation laboratory revealed that the most important intervention to improve survival of primary cardiac arrest, due to VF, was the early and uninterrupted generation of near continuous adequate arterial perfusion pressures by forceful chest compressions (Kern et al, 1988; Berg et al, 1997; Kern et al, 2002). This led us to develop a new approach to patients with primary cardiac arrest that we called cardiocerebral resuscitation (Ewy, 2005; Kern et al, 2005). We have always recommended guidelines for CPR and ECC for patients with secondary cardiac arrest—that is, cardiac arrest secondary to respiratory failure such as drowning or drug overdose. However, in the US, 70% to 75% of all OHCA are primary (Rea et al, 2004; Bobrow et al, 2010).
The Resuscitation Council (UK) arranged a meeting in London in 2002, led by Dr Douglas Chamberlain, to discuss promising experimental research suggesting that a new approach to the resuscitation of patients with OHCA should be considered. Some of the deliberations and evidence reviewed by this group were published (Ewy, 2003).
Convinced by the 24 to 48 hour neurological intact outcomes in our realistic experimental models of primary OHCA—where our emphasis was on near continuous chest compressions—and encouraged by our colleagues in the UK, in 2003 we announced our intention to institute a new, non-guideline approach to the treatment of patients with primary OHCA (Ewy, 2003). The article in which we announced our intentions of not following the decades-old guidelines for the therapy of patients with primary cardiac arrest was submitted with the title: ‘A new approach for out-of-hospital CPR.’ It was published with an addendum by Dr Chamberlain— ‘a bold step forward’ (Ewy, 2003).
We called this new non-guidelines approach ‘cardiocerebral resuscitation’ to emphasize that in treating primary cardiac arrest, the major goal is restoring circulation to preserve brain and other bodily functions (Ewy, 2005). A similar approach was advocated by Dr Chamberlain and his colleagues that they called ‘Protocol C’. Fortunately for patients with OHCA in the US, cardiocerebral resuscitation was instituted in Tucson in 2003, in two counties of Wisconsin in 2004, in several cities in Arizona in 2005, and in Kansas City, Missouri in 2006. Each location subsequently reported that cardiocerebral resuscitation in patients with OHCA and VF resulted in dramatic improvement in survival to hospital discharge (Kellum et al, 2006; Kellum et al, 2008; Bobrow et al, 2009; Garza et al, 2009) (Figure 1).
What led to cardiocerebral resuscitation for primary cardiac arrest?
As noted above, one of the major findings in our experimental laboratory was that, during prolonged resuscitation efforts for VF arrest, the major determinant of survival was the arterial pressures generated by chest compressions (Kern et al, 1988). The lack of chest compressions by bystanders because of the requirement for rescue breathing or mouth-to-mouth ventilation was then, and unfortunately still is, a major obstacle to survival of patients with OHCA. This led us, early on, to recommend chest compression-only CPR (CO-CPR) for all bystanders who witness primary cardiac arrest because it was better than no CPR at all (Ewy, 2000), as the vast majority of patients with OHCA were not receiving bystander CPR.
We found in our swine model of primary OHCA that the arterial blood was almost fully oxygenated, and remained so as long as there was no forward blood flow. In fact, arterial samples, taken 12 minutes after inducing VF, had oxygen saturations that were near normal.
The decades-old recommendation that the first step in resuscitation should be mouth-to-mouth ventilation was indeed unfortunate for it was not necessary in patients with primary cardiac arrest, and yet the resuscitation guidelines prevented most bystanders from initiating bystander CPR. These and other physiologic reasons for not requiring so called ‘rescue breathing’ have been reviewed elsewhere (Ramaraj and Ewy, 2009).
Soon after the 2000 AHA guidelines for CPR and EMS were published (AHA, 2000), an important discovery was made in Cardiff, Wales (Assar et al, 2000). An analysis of video recordings of lay individuals performing CPR, having just completed their certification training, showed that they interrupted each set of chest compressions an average of 16 seconds to deliver ‘two quick breaths’ between each set of 15 chest compressions, as recommened in the guidelines (Assar et al, 2000). We then studied the effect of this realistic interruption of each set of chest compressions by a single rescuer and found that CO-CPR resulted in significantly better survival (Kern et al, 2002).
We recommend CO-CPR for primary cardiac arrest treated by medical and certified health professionals. This recommendation was based on the fact that medical students, recently AHA certified in basic life support, interrupted chest compressions for 14 seconds, and paramedics 10 seconds between each set of chest compressions to provide the so-called ‘rescue breaths’ during single rescuer bystander CPR (Heidenreich et al, 2004; Higdon et al, 2006). Even when certified, professional individuals are not likely to perform bystander CPR (Swor et al, 2006), especially if mouth-to-mouth ventilations are required (Brenner et al, 1996).
Cardiocerebral resuscitation
Cardiocerebral resuscitation was instituted in Tucson, Arizona in 2003 (Ewy, 2005; Kern et al, 2005). At that time, cardiocerebral resuscitation had only two components—the ‘community’ and the ‘prehospital’ (Figure 2). These two components are of critical importance as the battle for life or death of the patient with OHCA is most often won or lost in the field—long before the patient is hospitalized. The third or ‘hospital’ component, pioneered in Europe and Australia, was added statewide in Arizona in 2008 (Bobrow and Kern, 2009) (Figure 2).
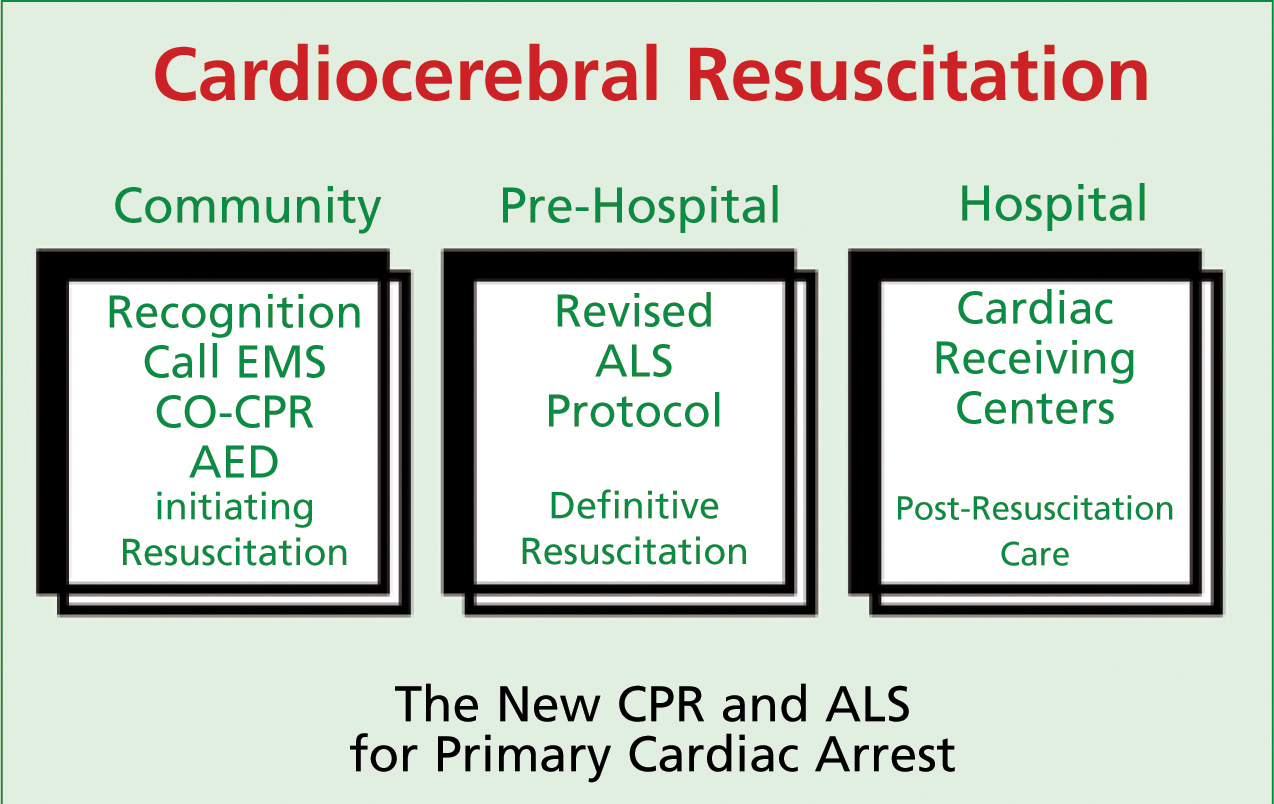
The community component of cardiocerebral resuscitation
The community component of cardiocerebral resuscitation (Figure 2) encourages early recognition of primary cardiac arrest by defining it as an unexpected, witnessed (seen or heard) collapse in an individual who is not responsive. Rarely, patients with primary cardiac arrest will present with seizures. Notice that this definition does not mention anything about the presence or absence of arterial pulsations, or the presence or absence of respiration. In contrast to conventional wisdom, the majority of patients with witnessed primary cardiac arrest, gasp. Gasping or agonal breathing is a sign of cardiac arrest. Clark et al (1992) reported that 55% of patients with primary cardiac arrest gasp.
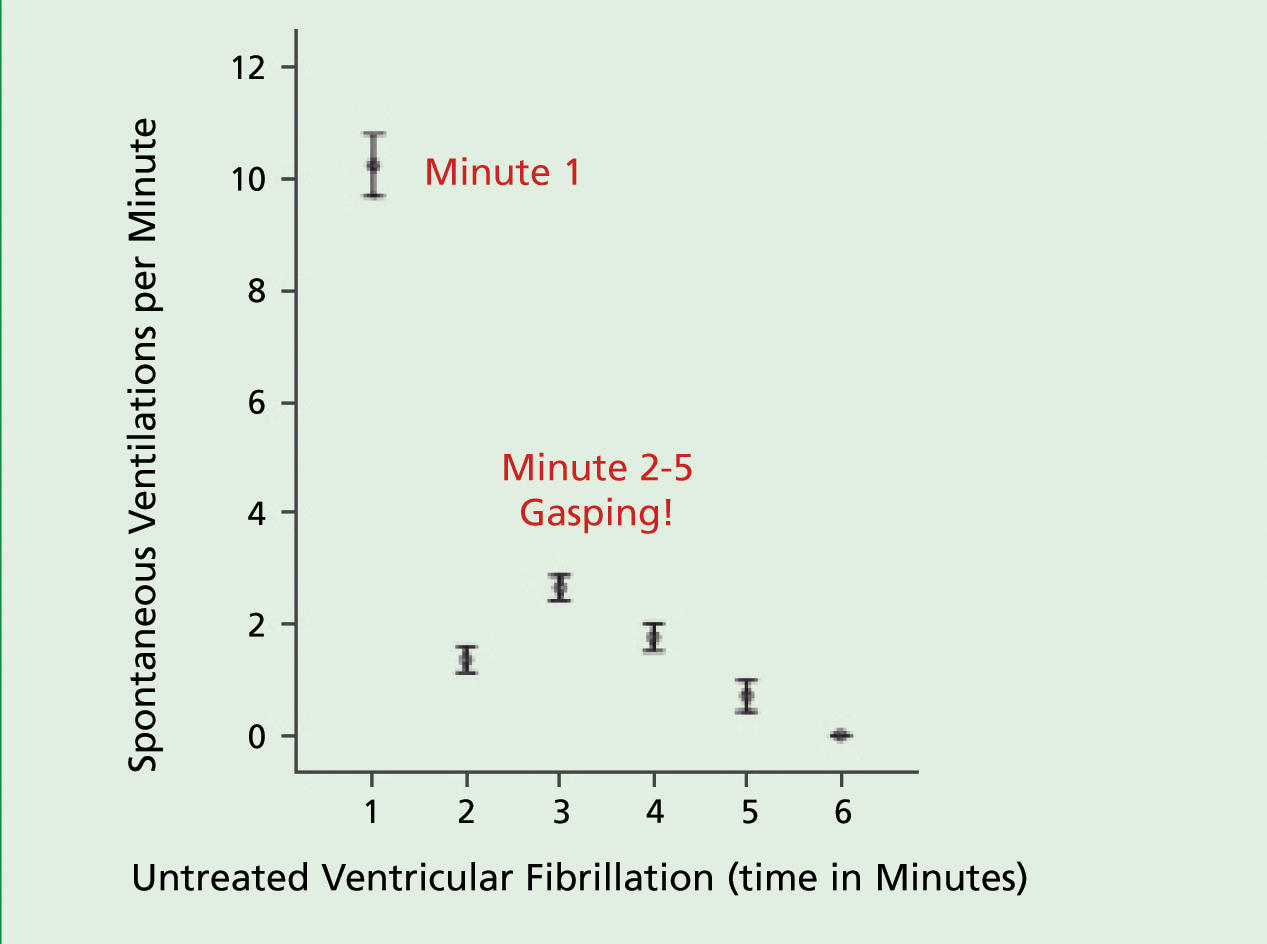
We found that if resuscitation efforts are initiated early, gasping is likely to begin or continue and such patients are most likely to survive (Bobrow et al, 2008; Zuercher et al, 2010). The recognition that gasping occurs in the majority of patients with OHCA is critical, as emergency dispatchers contacted by phone often ask if the person is breathing. Since most bystanders, under the stress of the event, cannot distinguish between ‘breathing’ and ‘gasping or agonal breathing’, the answer, even in patients with primary cardiac arrest, is often in the affirmative. The result is that the cardiac arrest is often not recognized until several minutes later when the arrested individual stops gasping, greatly diminishing the chance of survival.
As shown in Figure 3, gasping is common in our experimental swine model of VF OHCA, occurring one to three times a minute in the previously described crescendo-decrescendo frequency pattern (Zuercher et al, 2011). We found that for the first minute of VF arrest, the subjects continued to breathe normally (Zuercher et al, 2011).
Critical to the ‘community’ component of cardiocerebral resuscitation (Figure 2) is CO-CPR for primary cardiac arrest (Ewy, 2005). The reason for this is that with primary cardiac arrest, the arterial blood is oxygenated at the time of the arrest. The most effective intervention is continuous chest compressions, as during cardiac arrest each chest compression is the victim's ‘heart beat’ and interruptions for any cause, interrupts blood flow to the brain, decreasing the chance of survival. However, continuous chest compressions are difficult and tiring. If another person is available, they should take up a position on the opposite side of the chest and the two take turns providing rapid forceful chest compressions with full release after each compression.
Advocating and teaching CO-CPR
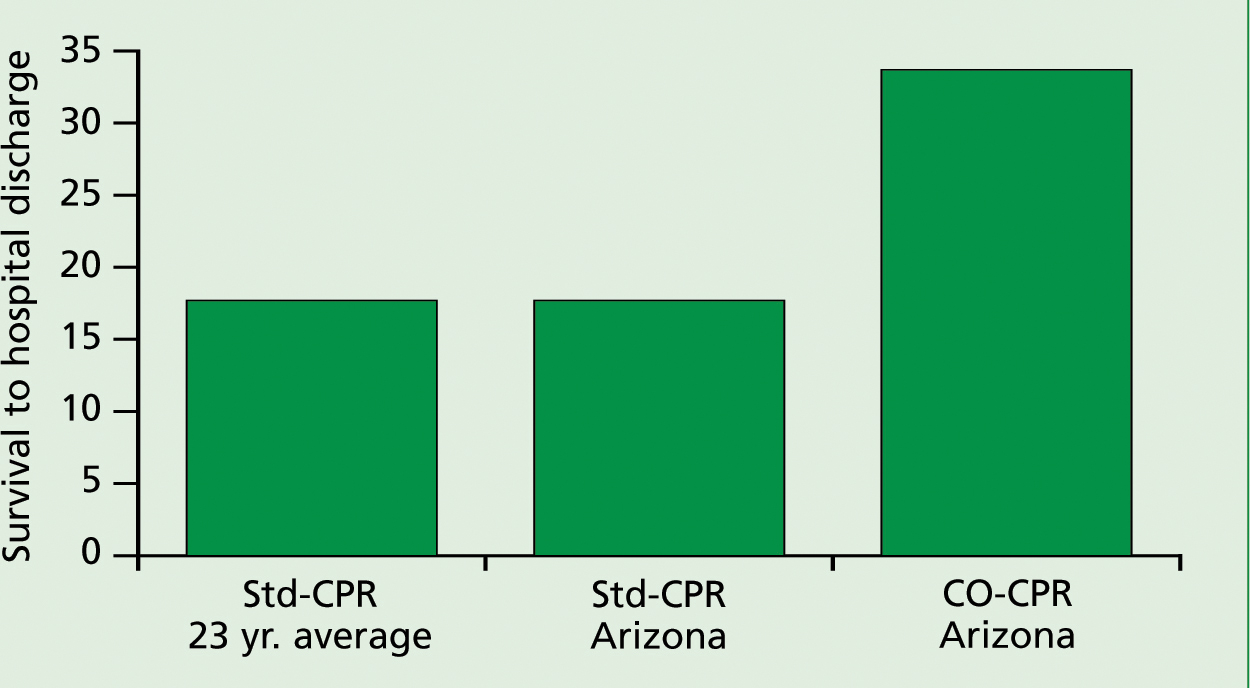
CO-CPR by lay individuals has now been shown, when advocated and taught, to be associated with significantly better survival of patients with OHCA (Figure 4) (Bobrow et al, 2010). We advocated and began teaching CO-CPR in Arizona in 2004. Analysis of our near statewide experience found that the overall survival of patients with OHCA was 7.8%, with conventional CPR and 13.3% for CO-CPR (Bobrow et al, 2010).
In this study, we identified two other important findings: when advocated and taught, there was a significant increase in the rate of bystander CPR for patients with OHCA, from 28% in 2005 to 40% in 2009; and an increase in the likelihood of bystanders performing CO-CPR vs conventional CPR (20% in 2005 to 76% in 2009) (Bobrow et al, 2010).
As co-authors, the most important finding to us was that the subset of patients with the greatest chance of surviving—those with a witness collapse and VF arrest—had a survival rate of 17.7% for the conventional CPR group (identical to the average survival for such patients published between 1980 and 1993 in the US (Rea et al, 2004), but was 34% for patients with VF who received chest compression only by bystanders (Figure 4) (Bobrow et al, 2010).
The lay public can learn CO-CPR by accessing a 6 minute instructional video created by the University of Arizona Sarver Heart Center: http://tinyurl.com/23m6sk9. We encourage you to use and to recommend this link as you encourage the lay public to help improve survival in patients with OHCA.
Dispatch directed CO-CPR for cardiac arrests
The first randomized trial of dispatch directed bystander CPR was reported by Hallstrom et al (2000). While survival was better in those who received CO-CPR, the difference was not statistically significant. Two additional randomized trials of dispatch directed CO-CPR vs standard CPR were published in 2010 (Rea et al, 2010; Svensson et al, 2010). A meta-analysis of these three trials reported that survival was statistically better when bystanders of patients with OHCA were given dispatch phone instruction in performing chest CO-CPR, as compared to chest compressions plus mouth-to-mouth ventilations (Hupfl et al, 2010). These findings should encourage all emergency dispatch systems to focus on advocating CO-CPR for all OHCA. This is a more practical approach to increase the lay public's willingness to perform bystander CPR, and it has been proven to save lives.
Encouraging the use of automated external defibrillators
The final component of the community phase of cardiocerebral resuscitation (Figure 2) is the recommendation to use an automated external defibrillator (AED) if available. The general public can be encouraged and familiarized with the use of AED by referring them to a training video on the University of Arizona Sarver Heart Center website: http://www.heart.arizona.edu.
Prehospital component of cardiocerebral resuscitation
The second component of cardiocerebral resuscitation is the prehospital component for the EMS (Figure 2). The prehospital component is an altered approach to advanced life support (ALS) therapy (Figure 5) by EMS that has resulted in improved survival of patients with OHCA (Figure 1) (Ewy, 2005; Kern et al, 2005; Kellum et al 2008; Garza et al, 2009; Bobrow et al 2009).
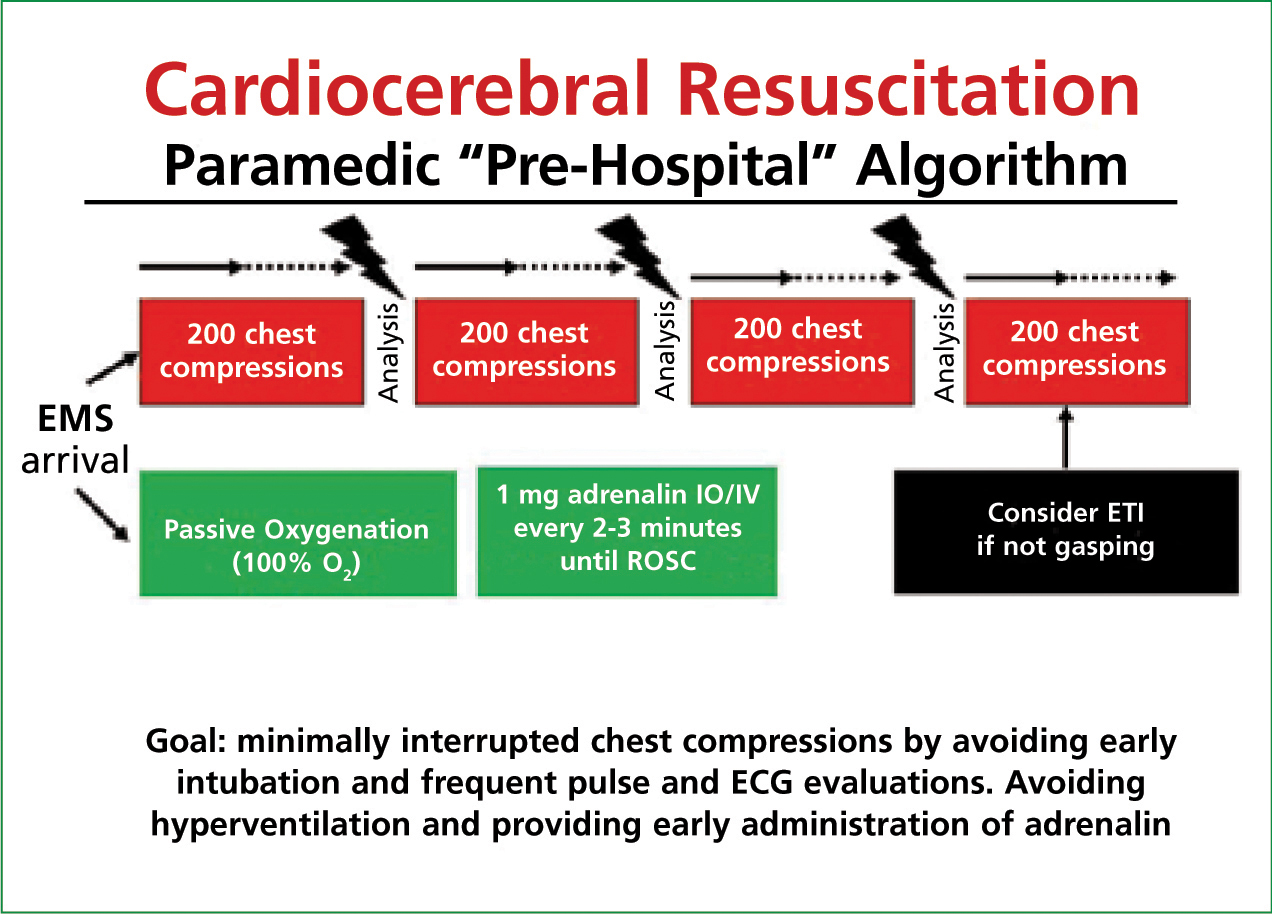
For primary cardiac arrest due to ventricular fibrillation, it advocates a series of near continuous chest compressions before and after a single defibrillation, passive ventilation, and the early use of epinephrine (adrenaline) (Figure 5).
If the patient is observed to develop VF after their arrival, they immediately defibrillate. For the vast majority of patients, the paramedics did not witness the primary cardiac arrest, and it is assumed that the patient is not in the ‘electrical phase’ of ventricular fibrillation (VF) arrest—the early phase of untreated VF where the patient is most likely to respond to a defibrillation shock with a perfusing rhythm (Weisfeldt and Becker, 2002). Therefore, the initial intervention is the prompt initiation of 200 uninterrupted chest compressions at 100 compressions per minute, with rhythm analysis followed by a single defibrillation shock when indicated, followed immediately by another 200 post-shock chest compressions before pulse check or rhythm reanalysis (Figure 5) (Ewy, 2005; Kellum et al, 2006; Kellum et al, 2008).
The technique of chest compressions is taught with a metronome to emphasize the importance of a compression rate of 100 per minute. Forceful chest compressions followed by full chest recoil after each compression is stressed. In the field, a metronome is attached to defibrillators (Kellum et al, 2008). If a single rescuer arrives with an AED (some police cars are equipped with AEDs), the electrode pads are placed first to limit the duration between discontinuing of the chest compressions and delivering the shock.
Resuming chest compressions immediately after the defibrillation shock without an analysis of the electrocardiogram (ECG) or searching for a pulse is a crucial step (Figure 5). It was (and probably still is in most areas), a common scenario for physicians and paramedics, upon seeing QRS complexes on the ECG monitor after the electrical shock, to halt chest compressions to search for a pulse. However, while they are searching for a pulse, the ECG of the arrested subject with post-defibrillation pulseless electrical activity (PEA), who do not receive chest compressions, will usually deteriorate into asystole. The attempted resuscitation is restarted, but now for a non-shockable rhythm. Patients who receive immediate chest compressions following a successful defibrillator shock are more likely to have an augmented arterial pressure and gradually develop a perfusion rhythm (Ewy, 2005).
Endotracheal intubation delayed
Endotracheal intubation (ETI) is initially prohibited by cardiocerebral resuscitation as this procedure interrupts chest compression for such a prolonged period of time that it often precludes survival. This component of cardiocerebral resuscitation, initiated in 2003, was based on our in-hospital experience of observing physicians, requiring the cessation of chest compressions for prolonged periods of time, while performing ETI for individuals undergoing resuscitation for an inhospital cardiac arrest. We assumed that this was also a problem with EMS systems.
Wang et al (2009) reported the duration that paramedics interrupted chest compressions for ETI in 100 patients with OHCA. The median duration of interruption of chest compressions was 47 seconds, one third exceeded 1 minute, and one quarter exceeded 3 minutes (Wang et al, 2009). This duration of no cerebral blood flow, late in a cardiac arrest, practically precludes a neurologically intact survival. A recent report confirmed that the elimination of ETI following a cardiac arrest is associated with improved survival. Studnek et al reported that individuals with OHCA who did not have ETI attempted were 5.5 times more likely to be discharged alive (Studnek et al, 2010).
Many paramedic supervisors are concerned that cardiocerebral resuscitation, with its delay in ETI, will result in the loss of experience of paramedics performing ETI. Cardiocerebral resuscitation does not eliminate the need for ETI, as most patients with return of spontaneous circulation (ROSC) undergo ETI prior to transportation. However, post-ROSC ETI does not decrease the survival of patients with cardiac arrest. ETI is recommended for all patients with OHCA whose initial rhythm is asystole, and in patients with a shockable rhythm after three sequences of 200 chest compressions, followed by attempted defibrillation in those patients who are not gasping (Kellum et al, 2008).
Positive pressure and excessive ventilations
Why the recommendation for passive ventilation? Why not bag valve mask ventilation? The interruption of chest compressions is not the only adverse effect of positive pressure ventilation. During resuscitation efforts, the forward blood flow from chest compressions is so marginal that providing excessive positive pressure ventilation (rescue breathing, bag-valve-mask, or via endotracheal intubation) increases the pressure inside the chest, decreasing blood return and survival (Aufderheide et al, 2004). To make matters worse, during the resuscitation efforts of patients with cardiac arrest, hyperventilation was and in many areas, probably still, is very common. Dr Aufderheide's editorial, ‘Death by Hyperventilation’ focused attention on this important issue (Aufderheide et al, 2004). If positive pressure ventilation is indicated, a metronome to limit the number of ventilations is recommended.
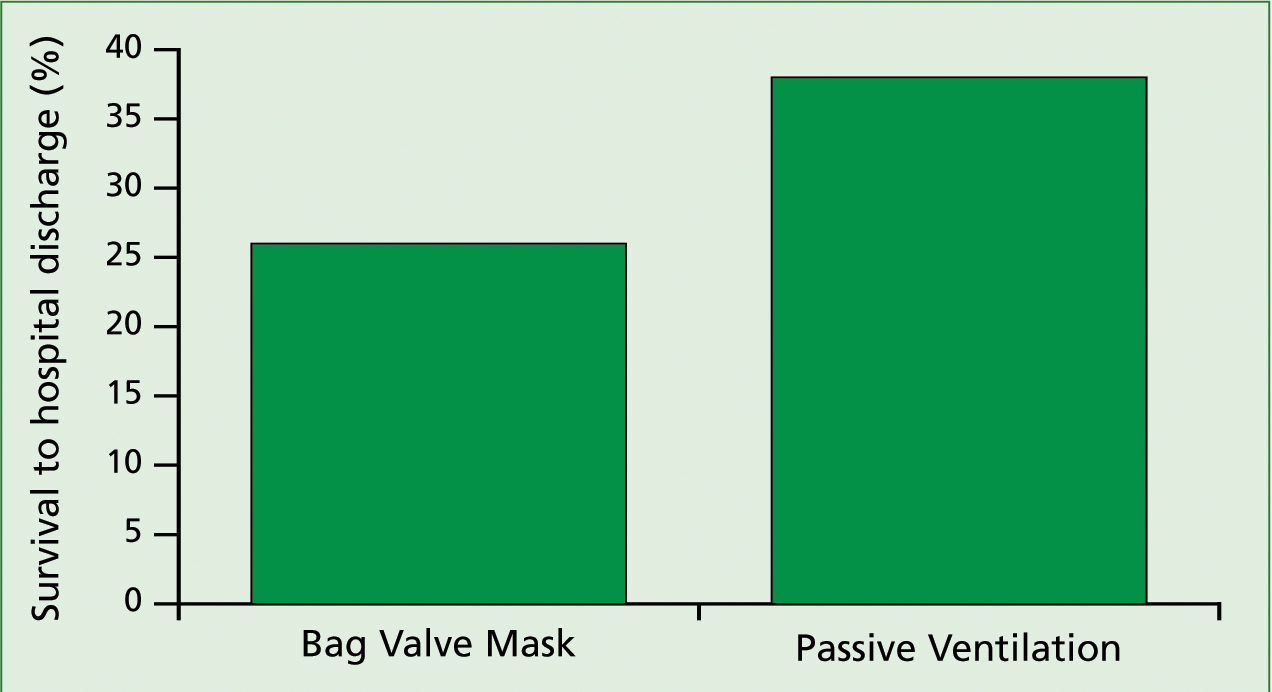
Survival in patients with primary cardiac arrest due to ventricular fibrillation when treated with passive ventilation
To limit ‘death by hyperventilation’, when we instituted cardiocerebral resuscitation in Rock and Walworth counties of Wisconsin in 2004, where the ‘prehospital’ component of cardiocerebral resuscitation was first instituted, the paramedics were instructed to use passive ventilation. When we advocated cardiocerebral resuscitation to the medical directors of the paramedic/firefighter EMS systems in the cities in the greater Phoenix area in 2005, those who selected to institute cardiocerebral resuscitation were, unbeknown to us, given the choice of using either passive ventilation (oropharyngeal airway insertion and high-flow oxygen by nonrebreather facemask, without assisted ventilation), or bag-valve-mask ventilation (by paramedics at 8 breaths/min).
When the results were analysed, we found that neurologically intact survival was significantly better (38.2%) in those who received passive ventilation than in those who received bag-valve-mask ventilation (25.8%) (Bobrow and Kern, 2009) (Figure 6).
Epinephrine during resuscitation
Cardiocerebral resuscitation advocates the early administration of epinephrine (Figure 5). The role of epinephrine in patients with OHCA was recently reviewed (Attaran and Ewy, 2010). In summary, the effect of epinephrine is due to its alpha-adrenergic or vaso-constrictive effects, as epinephrine with beta blockage facilitates resuscitation, but epinephrine administered with alpha adrenergic blockage is ineffective. A randomized trial of drug or placebo administration for patients with OHCA by Olaseveengen et al (2009) in Europe found that epinephrine administration was associated with an increased ROSC, but that this did not translate into improved survival to hospital discharge. However, in their study, epinephrine was administered quite late. The time of administration was not published, but the response times were late, suggesting that epinephrine was administered some time after 20 minutes.
In our experimental swine model of OHCA, the model on which we used to determine the best approach to subjects with OHCA and a shockable rhythm, we found that if effective chest compressions are begun very early, a reasonable arterial pressure can be obtained. The later chest compressions are initiated, the lower the arterial pressure achieved.
Finally, if chest compressions are begun very late, adequate arterial pressures cannot be obtained. Epinephrine, either intravenous (IV) or intraosseous (IO), may not be needed extremely early (first few minutes) of OHCA and is not effective when given late (i.e. later than 20-25 minutes), as in the study by Olasveengen et al (2009). However, epinephrine is effective if given soon after the EMS services arrive, assuming their arrival time is somewhere between 6 and 10 minutes. To accomplish early administration in patients with OHCA administration, IO administration is probably required (Zuercher et al, 2011).
Legality of a non-guidelines approach
It must be emphasized that guidelines are just that—guidelines. There are a number of concerns with the current system for developing resuscitation guidelines, not least as they recommend the same approach to two entirely different pathophysiological conditions; primary and secondary cardiac arrest. Another problem is that they involve so many individuals worldwide that they are only considered every 5 years. As a result, some of their recommendations are out-of-date almost as soon as they are published. The AHA and ILCOR did not come to the same scientific conclusion concerning bystander CPR. The senior author has other concerns about the AHA Guidelines process that have previously been published (Ewy, 2009).
Rather than following the Resuscitation Guidelines, we advanced the science of resuscitation by collecting data to know our results; made changes based on realistic animal studies; instituted these changes in areas, many where the outcomes of resuscitation for OHCA were poor, and then collected data to determine the effect.
Psychological effects of instituting cardiocerebral resuscitation
Sometime after cardiocerebral resuscitation was instituted in Tucson, Dr Kern was giving a talk to his son's grade school teachers at their faculty development programme about this new approach to resuscitation. He emphasized that this approach was only for primary cardiac arrest (unexpected witnessed collapse in an individual who is not responsive), and that standard CPR was indicated for collapse secondary to drowning or respiratory arrest. He nonetheless shared that our new approach (cardiocerebral resuscitation) was being used by the paramedic/firefighters in Tucson.
Aterwards, three teachers came forward and with some emotion thanked him for his efforts. All three of them were married to paramedics, and with this new approach, each of them has changed— one said, ‘they are excited about their job, their attitudes are different. For the first time in their 15 to 20 years of work they have had a successful resuscitation!’
Conclusions
Cardiocerebral resuscitation has changed many lives, and it has the potential to change many more—not only the lives of those suffering cardiac arrest, but the lives of those who provide the community, the prehospital, and the hospital components of cardiocerebral resuscitation (Figure 2).
