Historically there has been very little published on the pre-hospital identification and care of sepsis. Herlitz et al (2012) found only 12 papers dealing with the pre-hospital care of sepsis in a search conducted in 2011. Recently there have been a growing number of articles on pre-hospital sepsis focused at paramedics (Boardman et al, 2009; Barrett and Dikken, 2011; Langley and Langley, 2012; Small, 2012) and also within the wider media (Daniels et al, 2011; Hall et al, 2011; Herlitz et al, 2012). Across the UK there are a number of initiatives being implemented to improve the pre-hospital detection and care of this group of patients. Data from a recent study in Scotland showed that the majority (88%) of patients with sepsis arrive at hospital via ambulance (Gray et al, 2013). The numbers of sepsis cases seen by paramedics are increasing, so the ability of paramedics to spot this potentially life-threatening condition and act appropriately is vital (Seymour et al, 2012; Guerra et al, 2013).
Following a review of the use of lactate in the pre-hospital environment (McClelland et al, 2012), sepsis was identified as an area where the addition of lactate monitoring could potentially have an impact. This led to the authors trying to establish figures on the patients seen by ambulance clinicians with a suspected or confirmed diagnosis of sepsis. This search for local figures proved difficult, but national figures such as 36 000–64 000 deaths from severe sepsis annually in the UK (Daniels, 2011) were widely quoted.
The authors' initial objective was to establish baseline figures for the numbers of patients with sepsis being attended by ambulance crews within the North East of England. It was thought that these figures could be used as a reference point against which new interventions, such as lactate, could be compared. During the development period of this project a pre-hospital Sepsis Screening Tool (SST) (see Figure 1) was introduced into practice within the North East so the study became a method of establishing baseline figures and trying to estimate the impact of the newly introduced SST. The SST introduced is based on a tool adapted from the UK Sepsis Trust and modified for pre-hospital use.
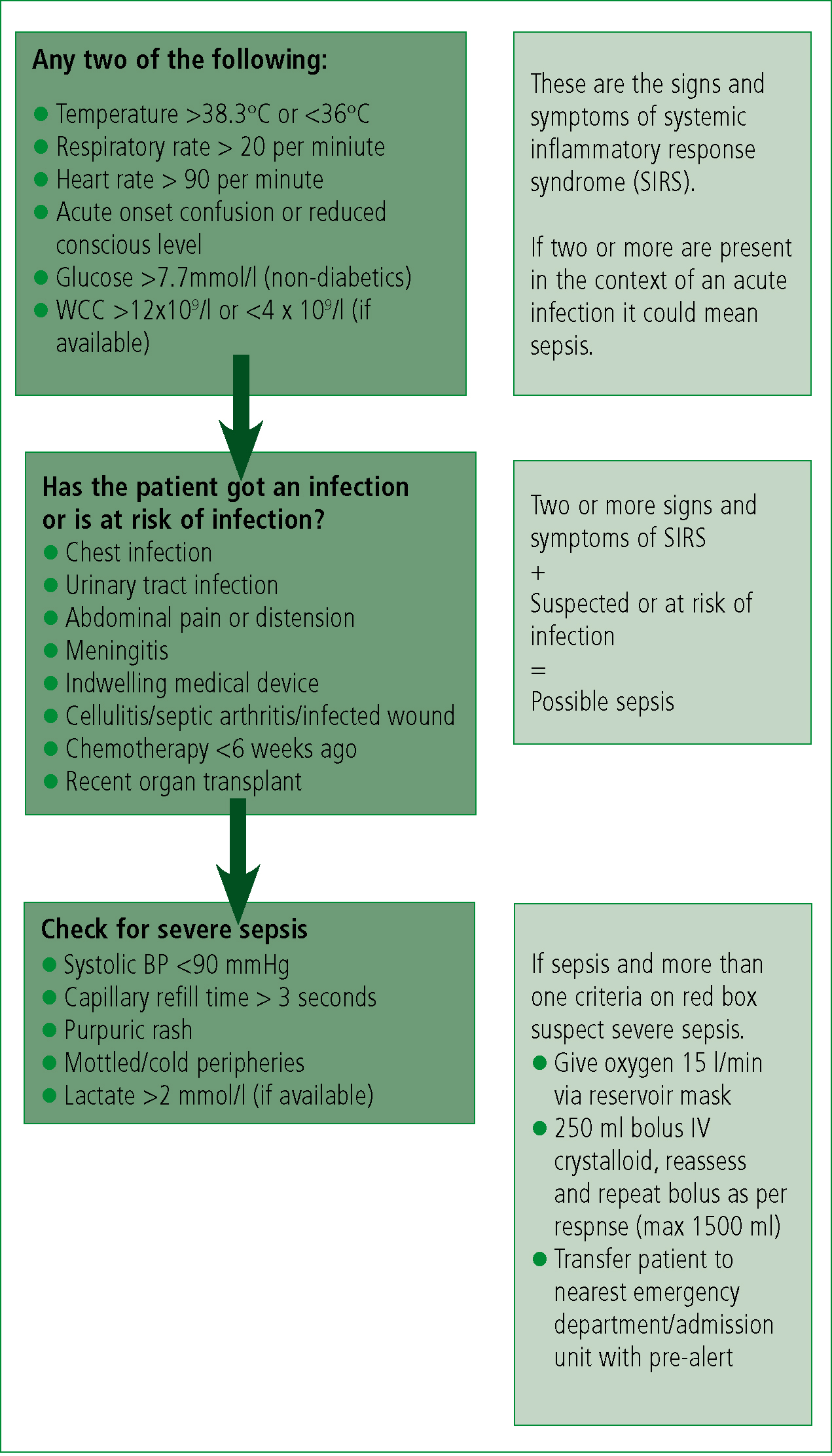
The SST was introduced in the North East Ambulance Service NHS Foundation Trust (NEAS) in the 2012–13 statutory and mandatory training programme which runs from April to March each year. The programme was front loaded, with efforts being made to get the majority of staff through the programme in the early months, in anticipation of winter pressures disrupting training. Correspondence with the training department indicates that around 1 hour was spent discussing and teaching the SST, and that all operational staff should receive this training within the year. In addition to the gradual roll out via the statutory and mandatory training, the SST and supporting information was circulated to all staff via a Patient Care Update (PCU) that went out on the 6 July 2012.
Prior to the introduction of the SST there was no guidance, or local protocol, in place for the identification and treatment of sepsis. Since the move to higher education, sepsis may be included in the material taught to student paramedics depending on their educational institution. Historically sepsis did not feature in the paramedic training syllabus in NEAS.
The Joint Royal Colleges Ambulance Liaison Committee (JRCALC) guidelines used by ambulance services have recently been revised. The latest JRCALC guidelines (2013) clarify and expand upon the previous definition of sepsis, with clinical signs and specific treatments, including recommendations for fluid therapy. The previous version (2006) had little specific guidance on sepsis. Sepsis was mentioned as a potential diagnosis for abdominal pains and was also included under meningococcal septicaemia. Septic shock received a brief mention in the section discussing headaches but this was focused around the identification of meningitis.
Methods
The authors explored a number of options for collecting data on the incidence of pre-hospital sepsis within their area. In the Electronic Patient Report Form (EPRF) used in NEAS there is no category for sepsis so it needs to be documented in the free text section. This free text documentation leads to inconsistencies in the way sepsis is recorded, which initially made electronic searches of the full patient database impractical.
Due to the challenges encountered when trying to identify all the recorded cases of sepsis from the complete patient records, it was decided to use only the cases that were pre-alerted to hospital. The authors used this subset of the population as pre-alerts are recorded by control staff in a standard format as opposed to the variety of ways that septic, or potentially septic, patients are recorded by ambulance clinicians and pre-alerting is specified in the treatment algorithm in the SST. The authors acknowledge that using this subset of the population will only identify the patients recognised as either time critical or as meeting the SST by the attending clinician, but information on this cohort of patient would be informative in the absence of any other figures.
The authors initially intended to collect data for 6 months starting in March 2012, as they thought that 6 months of data would allow them to establish baseline figures and detect any changes in practice attributable to the SST. During the course of this study the authors extended the pre-SST data collection period to 6 months and the post-SST data collection period to one year. The authors believe this range gives them a better baseline pre-SST to judge any difference made by the introduction of the SST and that a year's data post-SST allows all staff to receive the training. One year of complete data may also point towards any seasonal variations.
The authors used an automated daily report that identified all cases with pre-alerts. The report was run retrospectively for the early months then collated monthly on a continuing basis. The relevant data was extracted by removing duplicates and any calls related to patients below the age of 16 years. This age cut-off was selected as it is specified in the SST as the physiological parameters are based on adults. The remaining cases were searched for any mention of sepsis by experienced paramedics working in the research department. EPRFs were analysed on a month by month basis. Paper based Patient Report Forms (PRFs) were collected later in the process, due to the time taken to collect, scan and access, and added in to the relevant months.
As a final stage, the authors looked at all the cases where sepsis is recorded in the pre-alert and compared the treatment given to the treatment bundle included within the SST—this data was only collected where the authors had access to the full ambulance notes. Due to the population being considered, all cases were already pre-alerted so the authors recorded whether the patient was given oxygen, cannulated and any fluids. As part of the study the crews' impression of sepsis was compared to the SST to explore the correlation between the crews' documented impression and the SST criteria. During this stage the authors collected basic demographic data including age and gender.
At a late stage in the data collection process two additions were made. Firstly, due to changes in IT capabilities, the ability to search all call notes recorded in the contact centre merged with crew notes from the EPRF as a single process became available. This new facility was used retrospectively to search for any mention of sepsis in the data recorded, in order to include calls other than pre-alerts. Secondly, it was decided to contact the Office for National Statistics (ONS) to ask for any relevant information they had. This was used due to historical data being uncovered which indicated that the ONS collected regional figures for sepsis mortality.
Results
Results: patient characteristics
The authors were able to access either PRF or EPRF for 96% of the sample (n=472/490). The demographic data collected showed a fairly even split based on gender (54% male) and a predominantly elderly population with an average age of 73 years (range 18–101). These demographics are largely in line with what the authors would expect based on previously published work on sepsis (Daniels et al, 2011; Hall et al, 2011; Seymour et al, 2012; Gray et al, 2013).
Results: numbers of sepsis cases
The authors collected three sets of data/information that inform us about the number of cases of sepsis encountered by paramedics in the North East.
| Total patients transported to acute A&E | Pre-alerts to North East hospitals | Pre-alerts as % of total | Sepsis pre-alerts | Sepsis pre-alerts (%) | |
|---|---|---|---|---|---|
| Oct-11 | 17 516 | 760 | 4.3% | 7 | 0.9% |
| Nov-11 | 16 549 | 813 | 4.9% | 7 | 0.9% |
| Dec-11 | 18 423 | 911 | 4.9% | 10 | 1.1% |
| Jan-12 | 17 175 | 817 | 4.8% | 12 | 1.5% |
| Feb-12 | 16 470 | 782 | 4.7% | 8 | 1% |
| Mar-12 | 17 824 | 837 | 4.7% | 7 | 0.8% |
| SST introduced | |||||
| Apr-12 | 16 821 | 825 | 4.9% | 13 | 1.6% |
| May-12 | 17 709 | 781 | 4.4% | 24 | 3.1% |
| Jun-12 | 17 584 | 810 | 4.6% | 20 | 2.5% |
| Jul-12 | 19 434 | 859 | 4.4% | 33 | 3.8% |
| Aug-12 | 17 717 | 807 | 4.6% | 26 | 3.2% |
| Sep-12 | 17 568 | 846 | 4.8% | 31 | 3.7% |
| Oct-12 | 18 617 | 853 | 4.6% | 26 | 3% |
| Nov-12 | 18 041 | 892 | 4.9% | 39 | 4.4% |
| Dec-12 | 20 338 | 1191 | 5.9% | 66 | 5.5% |
| Jan-13 | 18 506 | 994 | 5.4% | 50 | 5% |
| Feb-13 | 16 707 | 1 184 | 7.1% | 50 | 4.2% |
| Mar-13 | 18 971 | 974 | 5.1% | 61 | 6.3% |
| Urgent cases mentioning sepsis | Emergency cases mentioning sepsis | Total calls mentioning sepsis | |
|---|---|---|---|
| Oct-11 | 54 | 39 | 93 |
| Nov-11 | 51 | 33 | 84 |
| Dec-11 | 50 | 49 | 99 |
| Jan-12 | 35 | 46 | 81 |
| Feb-12 | 55 | 47 | 102 |
| Mar-12 | 39 | 46 | 85 |
| SST introduced | |||
| Apr-12 | 54 | 41 | 95 |
| May-12 | 57 | 69 | 126 |
| Jun-12 | 47 | 62 | 109 |
| Jul-12 | 59 | 79 | 138 |
| Aug-12 | 51 | 76 | 127 |
| Sep-12 | 57 | 64 | 121 |
| Oct-12 | 54 | 91 | 145 |
| Nov-12 | 60 | 99 | 159 |
| Dec-12 | 65 | 125 | 190 |
| Jan-13 | 49 | 94 | 143 |
| Feb-13 | 63 | 90 | 153 |
| Mar-13 | 69 | 117 | 176 |
Results: introduction of the SST
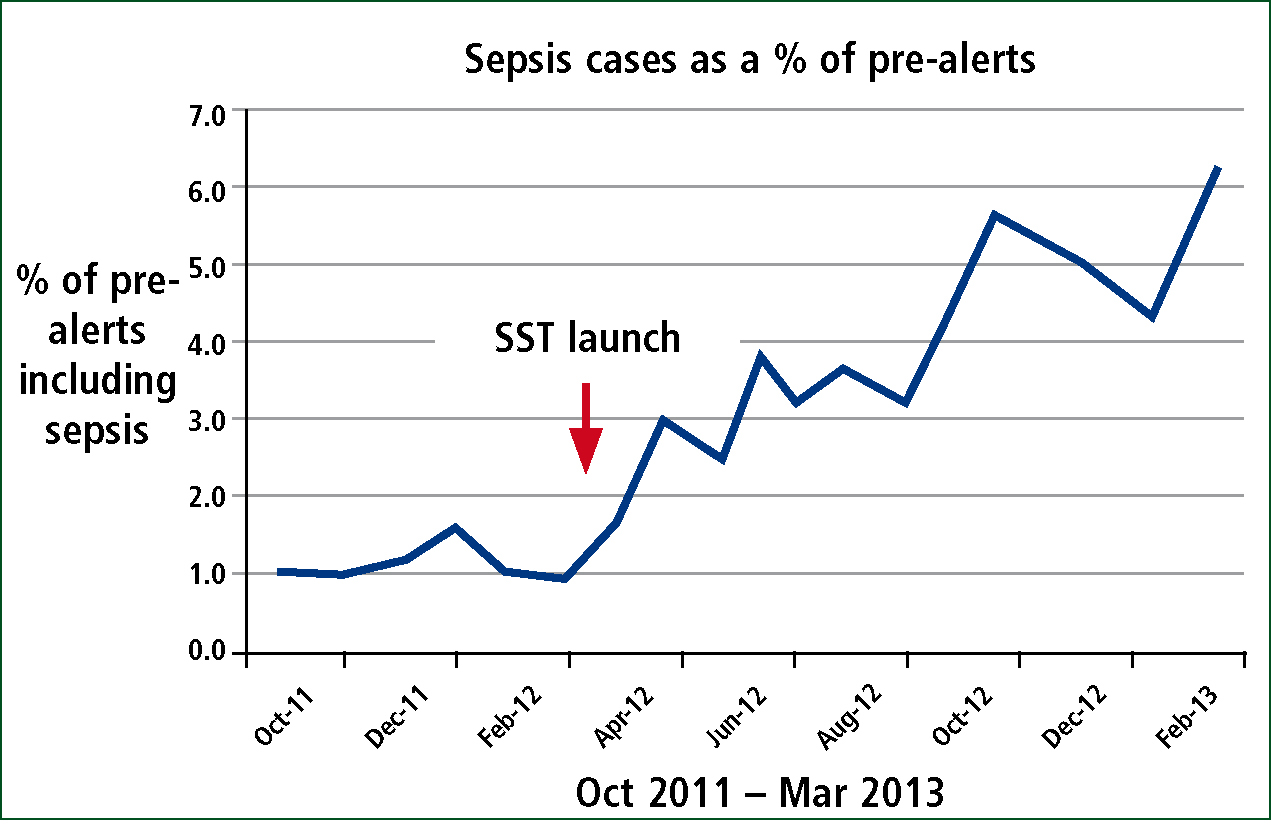
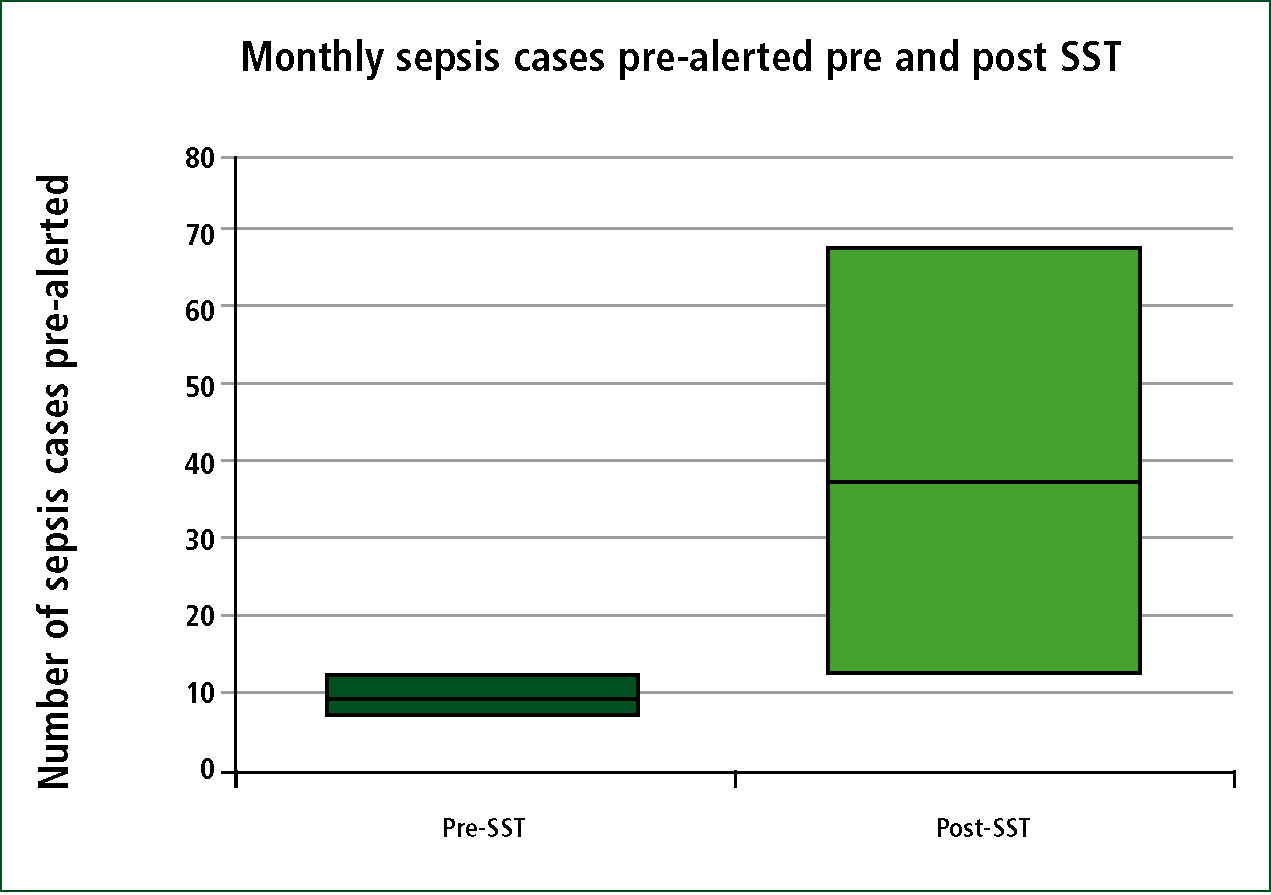
The results of introducing the SST on the numbers of sepsis cases pre-alerted can be seen in Table 1 and Figure 2. The number of cases pre-alerted for sepsis rises steadily in the months from April 2012 onwards and the number of sepsis pre-alerts as a percentage of the total pre-alerts rises steadily as well. The authors compared the number of pre-alerts for sepsis in the months pre-SST against the number of pre-alerts for sepsis in the months post-SST and found that there was a significant difference (Mann-Whitney Test conducted in SPSS19, P=0.001).
Results: treatment administered
The majority of patients identified received oxygen therapy (average per month 85%, range 70–94%), but less than half of all patients received intravenous (IV) fluids (average per month 44%, range 29–71%) and around a third of patients received both oxygen and fluids (average per month 38%, range 17–63%). These three measures showed a noticeable difference with the introduction of the SST. The authors found that the majority of patients were cannulated (average per month 69%, range 43–92%) with 84% of all cases reporting at least one attempt at cannulation.
Results: correlation of SST and documented observations
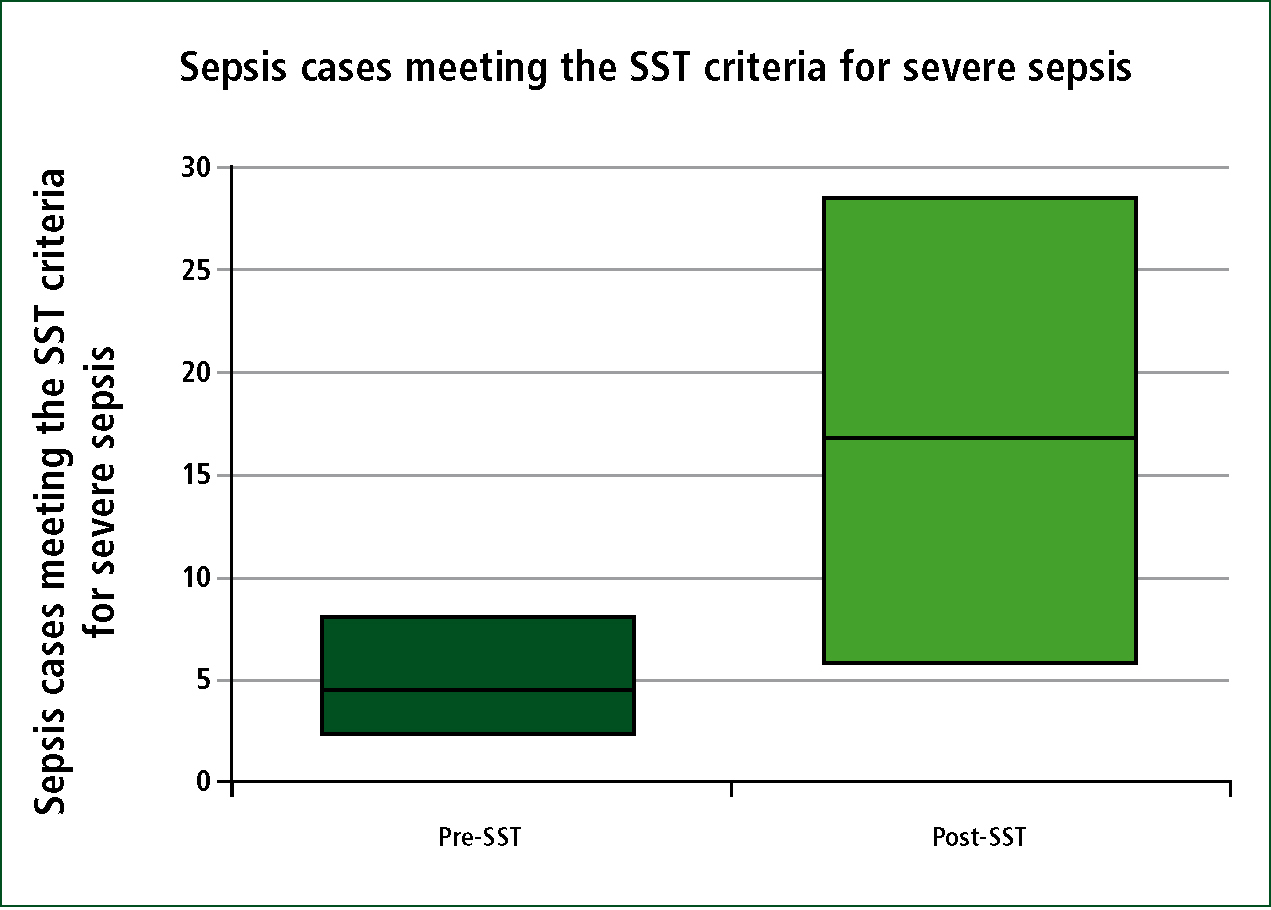
The observations documented in cases that were reported as sepsis were compared to the SST criteria. It was found that introducing the SST reduced the number of cases that did not match the criteria for sepsis (13% pre-SST vs 6% post-SST) and that the number of cases that matched the sepsis and severe sepsis criteria increased (87% pre-SST versus 94% post-SST).
Statistical analysis was carried out using SPSS19 with a Mann-Whitney test, comparing the number of suspected sepsis patients matching the SST severe sepsis criteria before, and after the introduction of the SST. There was statistically significant increase (P=0.001) in the number of patients with severe sepsis according to the SST criteria after the introduction of the SST and the sepsis education program (Figure 3).
Discussion
The introduction of the SST has changed sepsis from a vague and nebulous concept to a defined, therefore measurable, condition with a specified treatment bundle. This change allows us to measure our treatment of this patient group for the first time, which in turn allows us to focus on areas where we can improve.
The total number of pre-alerts is shown in Table 1 and displays slight month on month variations, with a gradual upward trend which was expected due to the increasing volume of calls. The data in Table 1 is encouraging as it shows an upward trend in both the number of cases pre-alerted as sepsis and also this as a percentage of the total pre-alerts as shown in Figure 1. This trend does not change noticeably with the service-wide patient care update that went out in July. This implies that large numbers of staff had already encountered the SST prior to July or that the training in the two day statutory and mandatory training was more effective than the blanket email.
It appears that prior to the introduction of the SST and sepsis education there was some knowledge and understanding of sepsis, as 87% of patients pre-alerted before April 2012 meet the criteria of the SST. This figure is based on a low number of cases and may be due to a number of factors, such as individual training and education, awareness from literature, or learning from other healthcare providers. After the introduction of the SST and sepsis education the percentage of patients meeting the SST criteria for sepsis was 94%.
The authors interpret the rising trend in pre-alerts to mean that the education around sepsis is raising the awareness amongst paramedics, so patients that may not have been pre-alerted previously are now being pre-alerted. Although the numbers of patients recognised as septic and pre-alerted has improved, the pre-hospital treatment administered to these patients does not show similar trends. The percentage of patients receiving oxygen, fluids and both treatments shows no obvious improvement since the introduction of the SST (Table 3). The data for patients receiving fluids and those receiving both treatments follow very similar trend lines, so it appears that patients rarely receive fluids in isolation but are much more likely to receive oxygen in isolation.
| Oxygen | Fluids | Oxygen and fluids | Cannulated | |
|---|---|---|---|---|
| Oct-11 | 86% | 43% | 43% | 86% |
| Nov-11 | 71% | 71% | 57% | 86% |
| Dec-11 | 90% | 40% | 40% | 70% |
| Jan-12 | 83% | 42% | 42% | 83% |
| Feb-12 | 88% | 63% | 63% | 63% |
| Mar-12 | 71% | 29% | 295 | 43% |
| SST introduced | ||||
| Apr-12 | 92% | 62% | 62% | 92% |
| May-12 | 87% | 33% | 17% | 75% |
| Jun-12 | 80% | 45% | 35% | 70% |
| Jul-12 | 91% | 48% | 45% | 73% |
| Aug-12 | 85% | 38% | 35% | 46% |
| Sep-12 | 93% | 30% | 23% | 70% |
| Oct-12 | 70% | 38% | 24% | 54% |
| Nov-12 | 82% | 42% | 29% | 63% |
| Dec-12 | 91% | 40% | 37% | 58% |
| Jan-13 | 82% | 44% | 28% | 76% |
| Feb-13 | 94% | 45% | 43% | 70% |
| Mar-13 | 87% | 36% | 30% | 64% |
The authors' findings of the low numbers of patients receiving fluids echoes the findings of Seymour et al (2010a) and may be due to a number of factors. Some patients will have been attended by crews who are unable to administer IV fluids, although the high percentage of cannulated patients shows most patients were attended by paramedics. Sepsis may have been one of multiple potential diagnoses so fluids may not have been appropriate for the primary concern.
The authors believe there is ongoing uncertainty around the use of pre-hospital fluids and potential confusion around what volume of fluid to administer and towards what target point. The widely accepted use of a systolic blood pressure of 90 mmHg as an indicator, and target, for fluid administration, and confusion between medical and trauma guidelines, may have some influence here. The impression of confusion was reinforced during a training session attended by one of the authors where a discussion was witnessed amongst the paramedics and trainers about fluid administration and no clear conclusion was reached. Whatever the reasons behind the low numbers of patients receiving fluids, it is a cause for concern given the importance placed on fluid resuscitation (Small, 2012).
The SST is constructed so that only patients who are positive for severe sepsis trigger the treatment bundle, and in the authors' data less than half of the cases met the criteria for severe sepsis. During the study the term sepsis was observed to be used interchangeably for severe sepsis and sepsis. This finding is supported by Erwin et al (2011) who found that paramedics are able to identify when a patient has sepsis, but they may not be able to differentiate sepsis and severe sepsis. Studnek et al (2012) demonstrated that the simple act of reporting an impression of sepsis by EMS crews led to a reduction in time to treatment, so identifying sepsis in any form should be beneficial for the patient.
The figures generated from the call and crew data at the end of the study show a more complete picture of the number of pre-hospital sepsis encounters (Table 2). The number of urgent cases stays virtually static throughout the study period whereas the number of emergency calls rises noticeably, especially from the introduction of the SST. This shows that the introduction of the SST has led to the identification of new patients in the emergency population but had little effect on the group of patients who are being transported into hospital as non-emergency cases.
Seymour et al (2012) published data on the incidence of severe sepsis using a large US based sample. They concluded that the ‘crude incidence rate of severe sepsis was 3.3 per 100 EMS encounters.’ The authors' data showed that less than 1% of all cases transported to hospital mentioned sepsis. This difference may be due to a large proportion of sepsis cases going undetected or it may reflect differences in the scope of service or another undetermined factor.
Reflecting on the experience of the authors, there were concerns that a significant percentage of patients with sepsis were not being identified and therefore not treated as time critical patients. Hopefully the growing awareness of sepsis, both within the paramedic profession and among other healthcare professionals, and the introduction of identification tools and treatment packages will change this. Discussions within NEAS with clinicians involved in using NHS Pathways revealed that any call received from a healthcare professional that specifies septicaemia will automatically generate a high priority (8 minute response) call unless manually overridden. This allayed fears that calls for patients with sepsis may be getting under-triaged at the contact centre.
Currently the ambulance services have no standardised criteria for pre-alerting patients to receiving hospitals, which is interesting considering the authors' data shows that nearly 5% of all calls transported involved a pre-alert. This leads to variability between practitioners as to when, or why, a patient would be pre-alerted. The introduction of the SST clarifies this issue for this condition. There has been discussion of the introduction of the National Early Warning Score (NEWS) type system to measure the severity of a patient's condition, but this has yet to be widely adopted in the pre-hospital setting (Roland and Jahn, 2012).
The SST training is delivered at an appropriate level for a mixed audience of paramedics and other ambulance staff. Perhaps there needs to be more than a one hour session and perhaps it should focus more training specifically on the paramedics, who will be the lead clinician and who can deliver needed interventions such as fluids. An extended skills training programme has recently been introduced within NEAS for a small cohort of paramedics, which includes focused sessions on sepsis, but it is too early to see what impact this will have. If paramedics with extended skills and treatment options can be shown to have a measurable impact on mortality, morbidity and all the associated costs of extended hospitalisation, then these initiatives may need support from commissioning groups.
Weaknesses
One of the main weaknesses with this study is that the authors have been unable to obtain a single comprehensive data set to establish the number of sepsis cases seen by paramedics within the North East. This weakness could be partially overcome with a more in-depth study of the call and crew data, but due to time constraints this was not possible.
The lack of patient follow up and linking with hospital records to confirm suspected cases of sepsis leaves us unable to comment on the accuracy of pre-hospital sepsis identification for both the pre-alert and the call and crew data. The ONS data is mortality data which is linked to a confirmed diagnosis of sepsis but is not linkable to ambulance records within the scope of this project. The authors are unable to determine in each case whether the attending paramedic used the SST as the diagnosis is documented but not the process of reaching it. As training on the SST was a phased process during the period of the study the authors cannot assume it was used in every case.
The changes to the methods of recording pre-hospital data during the study period is another weakness in this study and will be an issue with any research of a similar nature. Within NEAS the authors currently use both paper PRF and EPRF. The absence of easy, rapid access to the paper based section of the data is not an easy obstacle to overcome. Internal reporting shows that approximately 60% of all cases are recorded on EPRF. Within this study the number of pre-alerted sepsis patients recorded on EPRF was 79%. The reason for this sample including a higher than average number of cases recorded electronically may be due to paramedics being more likely to record a pre-alerted case on EPRF, and also that patients who are not conveyed are often recorded on PRFs, effecting the statistics as all of the patients in this sample were transported.
There are problems with the electronic reporting system used to generate the data that was used in this study in that the authors do not have access to a good set of tools to interrogate the data. Paramedics record a vast amount of information on each patient that they attend. Without the ability to easily interrogate this vast pool of data by a wide range of parameters we are always going to be limited in what results we can produce. Hopefully the necessary tools will be developed in the near future which should facilitate faster, easier and more accurate research using pre-hospital care data.
There are acknowledged problems with all medical records, and certainly paperwork completed in the pre-hospital environment, in that if it isn't written down, it didn't happen. In analysing all the data there are numerous examples of where interventions are not written down but may have taken place and an improvement in documentation may reveal different patterns. After the introduction of the SST and sepsis education, the awareness of the parameters may have led to crews recording more of the observations needed for the SST. Therefore, more patients may have been detected with sepsis or severe sepsis during the comparison due to better data recording.
Suggestions for further research
In the authors' opinion, this data only represents the tip of the iceberg as far as pre-hospital sepsis identification and treatment are concerned, so there are many avenues that need further work, including:
Conclusions
The introduction of the SST and the associated training has increased paramedics awareness of sepsis. The increased awareness has led to greater identification and reporting of sepsis, but has not led to significant changes in the pre-hospital treatment delivered. The importance of fluid resuscitation in septic patients is an area that needs reinforcement.
The authors have failed to establish definitive figures for the numbers of patients with sepsis encountered by paramedics in this region. Their study indicates that the true figure lies above the 1% of all transported cases obtained from their data.
Initially there was a low level of awareness, and therefore recognition and treatment, of sepsis so the improvements that the authors have shown are to be welcomed. The education of paramedics about sepsis needs to be maintained, expanded upon and the lessons learnt shared.
