Emergency Medical Service (EMS) providers were dispatched to the scene of a rollover injury accident involving a single vehicle on a rural highway. An Advanced Life Support (ALS) ambulance staffed with a paramedic and Emergency Medical Technician-Basic (EMT-B), responded under emergency conditions. Upon arrival at the scene, the EMS crew saw a car lying on its side with minimal external damage on the side of the roadway. Bystanders reported that the car was driving on the highway and suddenly veered off the road. Further questioning of bystanders and closer inspection of the vehicle revealed that the car had merely tipped onto its side and did not actually rollover. Responders initially believed the patient may have experienced either a syncopal episode or may have fallen asleep while driving.
Approaching the vehicle, pre-hospital providers found the lone occupant, an adult female, sitting in the driver's seat of the vehicle that was tipped on its side. The patient was a 67-year-old-female who was awake, alert and answering questions appropriately and did not appear to be in any distress. She stated that she was the restrained driver of the vehicle and prior to arrival of EMS responders had removed her seat belt restraint in an attempt to extricate herself from the vehicle. Her only complaint to providers was minor hip pain. She denied headache, neck or back pain, loss of consciousness, difficulty breathing, chest or abdominal pain and furthermore had no obvious outward injury on their initial evaluation while she was still in the vehicle. Her initial vital signs on scene were as follows: systolic blood pressure of 220mm Hg by palpation, heart rate of 116/min, respiratory rate of 16/min, and a blood sugar of 6.67 mmol/l. It took approximately twenty minutes for fire crews to extricate her from the vehicle. The extrication was prolonged by the fact that she had undone her seatbelt and was unable to climb out of the car on her own. Pre-hospital personnel then placed the patient in a rigid cervical collar and secured her to a long spine board for transportation to the hospital. After the patient was immobilised, they transported the patient to the hospital which was approximately 30minutes away.
During transport, the paramedic attending to the patient noted that she had become increasingly agitated and began pulling at her cervical collar, stating ‘I can't breathe’ repetitively. She continually attempted to sit upright on the bed and was fighting against her spinal immobilisation restraints. As her agitation increased, the EMS crew noted her oxygen saturations decreased and never rose above 89 % despite high-fow oxygen via a non-rebreather face mask.
Emergency Department Course
On arrival to the Emergency Department (ED), the patient was in severe respiratory distress and had an altered mental status. She continued to fail her arms around, grabbed at her cervical collar, and refused to answer questions appropriately. Instead, she yelled ‘you're killing me and I can't breathe’ The report given to emergency medicine physicians in the ED was that the patient was very well initially and stable with a minor complaint of hip pain. She had become progressively more agitated and hypoxic during transport. The physicians in the ED were also concerned about the report that the patient was involved in a rollover accident at highway speeds. It was not communicated to ED physicians by EMS that the car had merely tipped over. The patient was unable to cooperate with questioning regarding medical history and was in obvious respiratory distress. The decision was made to emergently, orally intubate the patient using Rapid Sequence Induction (RSI) with etomidate and rocuronium. After intubation, the patient's oxygen saturations improved from a pre-intubation saturation of 76 % to 99 %. After her airway was secured and her oxygenation improved, attention was then paid to the remainder of the primary and secondary survey. She continued to be very hypertensive with a post-intubation blood pressure of 260/140 mmHg. Propofol was started for sedation post-intubation. There were no obvious injuries noted on external examination, the only notable finding was persistent jugular venous distention (JVD) and crackles on auscultation of lungs. At this time, a chest radiograph was performed revealing diffuse interstitial infiltrates consistent with pulmonary edema, but with the questionable history of trauma could also represent bilateral pulmonary contusions. There were no obvious rib fractures noted and no subcutaneous air was present on the chest x-ray. The x-ray also revealed a large cardiac silhouette suggesting long standing hypertension or congestive heart failure. Her electrocardiogram (ECG) revealed left ventricular hypertrophy (LVH) with a strain pattern. A Focused Assessment Sonography in Trauma (FAST) performed at the bedside showed no intraperitoneal free fluid or pericardial effusion. At this time, the physicians in the ED got further clarification about the scene from EMS providers, regarding the true mechanism (i.e. car only tipped over) and determined that this was likely an acute episode of severe hypertension resulting in left-sided heart failure, causing fash pulmonary edema perhaps exacerbated by being supine and immobilised for a lengthy transport.
The ED physicians then sat the patient upright in bed, placed the patient on an intravenous nitroglycerin drip, and administered a bolus of intravenous fiurosemide for presumed cardiogenic pulmonary edema. However, the patient remained in a cervical collar and a typical trauma work up was done, which included a computed tomography (CT) scan of the brain, cervical spine, chest, abdomen, and pelvis as well as a troponin-I and brain- type natriuretic peptide (BNP) levels. Patient was admitted to the intensive care unit for further management.
Hospital course
Once admitted, the diagnosis of acute pulmonary edema from heart failure was confirmed by echocardiography performed by cardiology revealing decreased left ventricular ejection fraction of 45 % with grade 1 diastolic dysfunction. Her BNP value was also severely elevated at 2273 picograms/ ml. The patient continued to diurese, her blood pressure came down as the pulmonary edema was being treated with nitroglycerin, and the remainder of her trauma and cardiac evaluation were negative for any acute injury. Once extubated, the patient revealed a past medical history significant only for hypertension. Her home medications consisted of benzapril, an ACE inhibitor, and clonidine, an alpha-2 adrenoreceptor agonist. She had no previous history of heart failure and claimed to have an average systolic blood pressure of 160 mmHg on her home medications. Ultimately, she was discharged 48 hours after admission with a diagnosis of heart failure and had no residual problems as a result of this episode.
Adverse affects of spinal immobilisation
This case demonstrates the recognised complications of spinal immobilisation. Given the life altering consequences of a devastating spinal injury and a reported incidence of 40–50 per million people per year according to the National Spinal Cord Injury Statistical Centre, it is easy to understand reflexive spinal immobilisation of trauma patients. This is compounded by the legal exposure a provider might have for a missed unstable fracture. As a result, pre-hospital personnel, following the recommendation of the American College of Surgeons, commonly use rigid spine boards for the immobilisation and transportation of trauma victims. Easy to apply, a thin rigid board along with a cervical collar, and tape or straps make a patient easier to transport with an immobilised spine. Unfortunately, there is a paucity of available literature, particularly recent studies regarding the complications associated with immobilisation. Lerner et al (1998) write that as the consequences of this tradition most pre-hospital protocols require any trauma patient to be fully immobilised based primarily on mechanism regardless of clinical signs or symptoms.
However, there is little evidence to support the idea that rigid immobilization and transportation is beneficial. In fact, Hauswald (1998) argued that spinal damage occurs at impact (i.e. primary impact) and that subsequent movement usually will not cause additional neurologic harm. Furthermore, multiple studies over the last thirty years suggest that immobilization increases pain, increases tissue injury, decreases pulmonary function, and provides minimal to no neurological benefit.
Pain
Increased pain associated with spine board immobilisation, especially if prolonged, has been documented repeatedly. Barney et al (1989) concluded that spine boards lead to unnecessary radiography and expense. They looked at pain associated with immobilisation and found that immobilisation resulted in cervical and lumbar pain and tenderness—the same criteria usually relied upon for obtaining spinal imaging. Chan et al (1994a; 1994b) investigated the effect of spinal immobilisation on healthy volunteers and concluded that it can causes significant pain in otherwise uninjured patients in as little as thirty minutes. The spine board was associated primarily with headache, back pain, and mandible pain. Looking at padded versus unpadded spine boards for cervical spine immobilisation, Walton et al (1995) found that while padded boards resulted in significantly less pain, all subjects still experienced pain as a result of their immobilisation. Lerner et al (1998) studied 39 healthy individuals over the age of 18 and reported that greater than 76 % experienced pain after immobilisation on an unpadded board and that 69 % of their subjects experienced pain after immobilisation on a padded board. Furthermore, additional occipital padding made no difference in perceived pain in their study. Cross and Baskersville (2001) compared pain scores of patients on traditional hard wooden boards to those immobilised on vacuum splints. They found statistically significant increases in pain at the occiput, lower back, and sacrum of immobilised volunteers on hard boards. However, they also recognised the practical obstacles to wide spread implementation of vacuum splints such as the increased space taken up in ambulances, their questionable durability, achieving adequate decontamination, and increased cost.
Tissue injury
Cordell et al (1995) took the investigation of pain caused by spine boards one step further. They concluded that the boards were not only painful but that the tissue-interface pressure may be high enough to cause tissue ischemia. Their study was supported by several earlier reports. Linares et al (1987) concluded that board immobilisation results in increased development of pressure sores. This is due in part to the delays such as additional imaging frequently associated with a patient arriving at the hospital on a rigid board. Mawson et al (1988) found that the time on a board correlated with the development of pressure ulcers within eight days of injury. More recently, Hauswald et al (2000) compared four methods of immobilisation attempting to maximise comfort and minimise ischemia. While recognising the beneft of long boards, they note that spinal immobilisation has never been shown to affect neurological outcome and that most patients are not truly immobilised. Patients tend to reposition themselves on the board, which could in theory worsen any spinal injuries. The exception might be those with trauma that makes it impossible to feel or move—the very patients at highest risk for tissue hypoxia. Ultimately, the authors recommend immobilisation on a soft surface or vacuum splint. In 2010, Berg et al (2010), using near-infrared spectroscopy, concluded that healthy volunteers suffer sacral tissue hypoxia with reactive hyperperfusion following spine board immobilisation. A trauma patient, especially one with chronic health issues, experiencing poor peripheral perfusion from systemic hypotension would be at even greater risk for tissue hypoxia and pressure ulcer development.
Respiratory function
Multiple investigations detail the detrimental effects of rigid spinal immobilisation on the pulmonary function of healthy individuals. First, Bauer et al (1988) demonstrated that strapping healthy volunteers to a rigid board resulted in a decrease of their forced vital capacity, forced expiratory volume, and forced mid-expiratory fow creating a ‘marked pulmonary restrictive effect' similar to other restrictive diseases such as pulmonary or pleural fibrosis. This iatrogenic cause of decreased pulmonary function combined with a patient's preexisting pulmonary disease or concurrent traumatic pathology could have devastating consequences. Second, Schafermeyer et al (1991) looked at the effects of spinal immobilisation of the pulmonary function of children six to fifteen years old. Ultimately, they found that spinal immobilisation resulted in a reduction of forced vital capacity to 80 % of baseline. As a result, they concluded that pre-hospital personnel must consider spinal immobilisation as a variable when evaluating causes of ventilation difficulties in their patients. Third, Totten and Sugarman (1999), using healthy volunteers, measured respiratory function at baseline and during immobilisation. They found that six of the eight measures they checked showed a statistically significant difference during immobilisation. Ultimately, they found that the elderly and children suffered the most from immobilisation. Totten and Sugarman (1999) found that both rigid board and vacuum mattresses restrict respiration an average of seventeen percent in their healthy volunteers. A review by Kwan and Bunn (2005) found 11 clinical trials related to adverse effects of spinal immobilisation. Since death from asphyxiation is one of the major preventable causes of mortality in trauma patients, Kwan and Bunn believe the adverse respiratory effects to be particularly relevant.
Benefits of immobilisation?
As for the neurologic protection presumably given by rigid spine board immobilisation, the evidence is sorely lacking. In fact, Hauswald et al (1998) concluded that pre-hospital immobilisation has little to no effect on neurologic outcomes in patients with blunt injuries. Furthermore, their study comparing similar populations in Malaysia (non-immobilised ) and New Mexico (immobilised ) not only did not demonstrate a protective effect, it suggests that neurologic disability is actually higher with immobilisation. Possible reasons given for deleterious effects include many of already described disadvantages of immobilisation— delayed resuscitation, tissue hypoxia, and increased intracranial pressure from cervical collars. Schriger et al (1991), while attempting to determine how much occipital padding is required to place cervical spines in neutral position, defined as ‘the normal anatomical position of the head and torso that one assumes when standing looking straight ahead' found that immobilisation on a fat backboard actually places ninety-eight percent of subjects in relative cervical extension (beyond the 12 degrees of extension used as the radiographic definition of ‘neutral’). De Lorenzo et al (1996) also looked into the optimal position for cervical immobilisation. They, however, used magnetic resonance imaging to determine that the most favourable ratio of spinal canal/spinal cord cross-sectional ration at C5 and C6 was actually 14 degrees of flexion, not extension. Clearly, placing 98 % of patients in relative cervical extension does not achieve optimal positioning. Most recently, Shafer and Naunheim (2009) conducted a study that concluded that the least amount of cervical spine motion occurred when an individual was allowed to exit a vehicle on his or her own with just a cervical collar in place. The evidence against immobilisation in penetrating trauma is much clearer. Both Connell et al (2003) and Kaups et al (1998) conclude that penetrating trauma without evidence of spinal injury requires no immobilisation.
Decision to immobilise
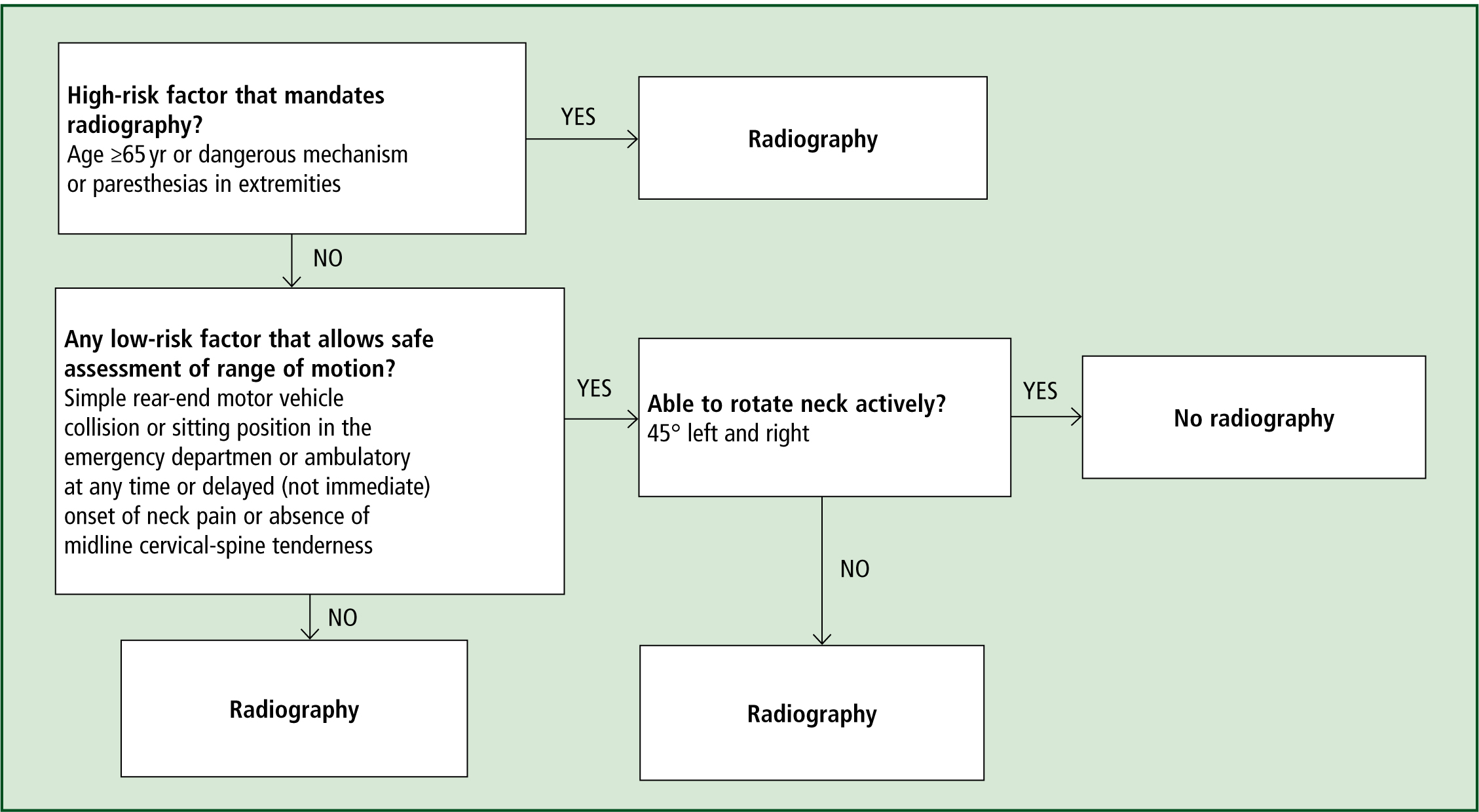
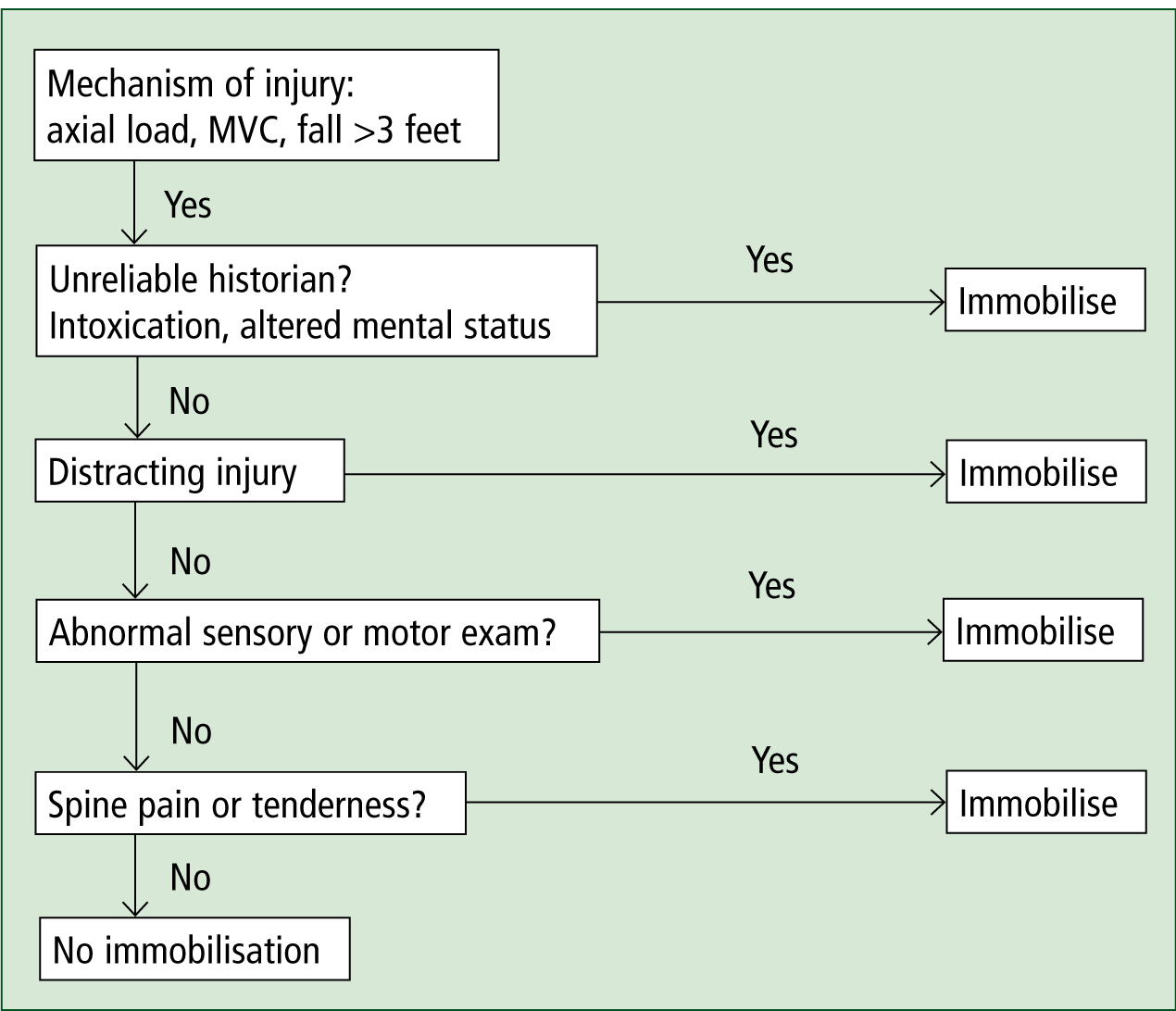
Given the known complications of rigid spine board immobilisation, when should pre-hospital personnel immobilise a patient? Domeier et al (1997) concluded that the traditional decision tree, based primarily on mechanism of injury, be augmented with one that identified clinical findings associated with spinal fractures or spinal cord injuries. Their retrospective review revealed that ‘at least one of the five findings of altered mental status, neurologic deficit, spinal pain, intoxication, and suspected extremity fracture' was documented in every patient with a cervical spine injury and present in nearly all thoracic and lumbar injuries as well. Similarly Hoffman et al (2000) described the validity of highly sensitive clinical criteria (the NEXUS criteria—National Emergency X-Radiography Utilization Study) based on an absence of neurologic deficits, intoxication, altered mental status, or a distracting injury to identify trauma patients at low risk of spinal injury and to rule out the need for radiography in the ED. Similarly, Steill et al (2001) developed the Canadian C-Spine rule for alert and stable trauma patients. This rule had a 100 % sensitivity based on three main questions. (See Figure 1 for Canadian C-Spine Algorithm) More recently, Burton et al (2006) examined the use of what they called a ‘NEXUSlike’ pre-hospital protocol. Their clinical assessment tool began with analysis of mechanism of injury then progressed through an algorithm of patient reliability, presence of distracting injury, abnormal sensory or motor exam, and spinal tenderness or pain. (Figure 2) They found that EMS providers could evaluate trauma patients with a four-step, clinically based, protocol that resulted in less than half of all trauma patients being immobilised. Out of 32 000 trauma patients, one unstable spine fracture patient was not immobilised. That patient was an eighty-six-year-old female who experienced back pain after moving furniture.
Conclusion
The case presented illustrates many of the difficulties faced by pre-hospital personnel regarding the decision to immobilise a patient. The rural EMS providers had been told they were responding to a trauma. At the accident scene, the patient was not altered or otherwise assessed as unreliable. She did not complain of spinal pain or tenderness and did not have a suspected fracture (although it could be argued that her hip pain was a potential fracture). Finally, she had no apparent sensory or motor deficits. Nevertheless, pre-hospital personnel responded in the traditional, conservative manner and immobilised the patient on a long spine board. Unfortunately, this resulted in an adverse outcome, including hypoxic respiratory failure which required intubation and a stay in the ICU. Kwan et al (2009) came to the same conclusion when they conducted a Cochrane Review looking to quantify the effects of different spinal immobilisation methods (including no immobilisation) on mortality, neurologic disability, and adverse effects in trauma patients. The review revealed no randomised control trials involving immobilisation and trauma patients. They found that no proven benefit existed, that the likelihood of further damage without immobilisation is small, and that spinal immobilisation has multiple adverse consequences including increased pain, tissue hypoxia, and decreased pulmonary function. Furthermore, if the patient had been allowed to sit upright with her collar still in place and received nitroglycerin, these actions may have prevented her adverse events. Finally, this case reinforces the value of frequent patient reassessment and clear communication with ED staff. Mechanism of injury has been shown to be a poor predictor of spinal injury and spinal immobilisation must continue to be questioned and investigated, especially given the known complications and equivocal value.
