The number of severely burnt patients in industrial countries is declining due to augmented safety systems and technical modifications (Allison, 2002). Against this background, a national survey in 1998 revealed 58% of UK ambulance services had no specific treatment policy for burns patients (Allison, 2002). Thus, prehospital carers often feel insufficiently prepared for caring of burnt patients, particularly children, which may be explained by a lack of teaching and simple, evidence based guidelines (Allison, 2002).
Approximately 60% of all patients suffering from burn injuries may be treated as outpatients having burnt less than 10% total body surface area (TBSA). For the corresponding 30–40% burnt patients, the primary care paramedic and physician have to provide initial care and identify correctly whether these patients have to be admitted to a specialized burn centre or to a general hospital.
In contrast to polytraumatized patients, where the speed and quality of the very first diagnostic and therapeutic measures is essential for the prognosis, there is no ‘golden hour’ in burn medicine (Muehlberger et al, 2010). In general, the pathophysiological alterations following severe burn injuries arise delayed and have to be managed in the burn centre. Burn injuries are most commonly caused by thermal, electrical or chemical contact; and depending on the genesis of the burn, the severity of injury is often determined by several organ disorders next to the dermal burn (Muehlberger, 2010).
Nevertheless, prehospital paramedics and physicians should exclude polytrauma and take precautions against the development of hypothermia and detect, or at least presume, a concomitant inhalation trauma which all have a major impact on the prognosis (Muehlberger, 2010). The adequate prehospital emergency treatment should include a safe approach of the paramedic with the aim of stopping the burning process. An appropriate dressing is essential and analgesia during the transport has to be initiated. Accordingly, the evaluation of precise information regarding the circumstances of the burn injury may also be of great importance.
Unlike the in-hospital treatment of burn patients, there are hardly any widely-used guidelines for the treatment of burn injuries in the prehospital setting (Giessler et al, 2004; Muehlberger et al, 2010). The aim of this article is to summarize the essential steps of prehospital burn treatment, analyze pitfalls as well as ‘do's and don'ts’ and discuss guidelines for the emergency care of thermal, electrical and chemical burn injuries, with additional focus on prehospital treatment of burnt children.
Thermal burns
Background pathophysiology
Burns of the body's surface exceeding approximately 15% TBSA may result in extensive pathological effects with an inflammatory response which can affect various organ systems. Although these pathophysiological changes generally occur delayed so that the prehospital carer does not have to deal with the resulting burn disease; in general, a short summary of the possible disorders will help the paramedic to act properly and to feel prepared.
The body is subject to multifactorial dysregulations including the sudden release of vasoactive mediators from the burnt body surface area (BSA). The loss of skin integrity leads to a decrease of body temperature with affected thermoregulation—this increases the susceptibility for infections and energy consumption of the organism.
The result of this disorder can be subsumed in a hyperdynamic state. There is a very popular misunderstanding that burnt patients lose large quantities of fluids and proteins via the open skin wounds immediately after the burn. Disorders of capillary integrity (‘capillary leak’) due to vasodilatation result in volume displacement and reduced mean arterial pressure.
Capillary permeability is increased with a maximum 6–12 hours after the trauma with oedema and low cardiac output which subsides 24 hours after trauma. Fluid displacement and loss of skin integrity can cause an immune deficiency state and loss of intravasal proteins which regulate the oncotic pressure.
All these pathophysiological findings have an impact on the treatment of burnt patients and should be taken into consideration by the prehospital burn care team, especially as there can be a time delay between burn trauma and paramedic contact.
Algorithmic steps
The approach to a burnt patient should be in acordance to the following algorithmic steps which have been modified with respect to UK consensus guidelines (Allison and Porter, 2004a, 2004b; Kramer et al, 2001).
Stop the burning process
At the location of the accident, the burning process has to be stopped or rather extinguished—as far as the primary carer can act obeying all rules of self protection. For thermal burns, professional fire workers should be involved, while specially trained emergency teams may perform decontamination in chemical burns. If the burnt patient remains in the vicinity to high voltage, an electrician should cut off the currency before the paramedic makes contact with the patient. All burnt clothing and any jewellery should be removed unless it is merged with the patient (e.g. polyvinyl chloride, polyester).

Cooling
There are some controversial discussions about this step—especially regarding the correct time, temperature, timeframe and medium. Many patients are often mistakenly cooled down during the transport and arrive to the burn care centre or hospital with mild to severe hypothermia, which has a prognostic impact with increased mortality (Lonnecker and Schoder, 2001). Nevertheless, cooling has a high analgetic potency and can reduce the zone of stasis where capillary perfusion is reduced. This zone is essential because it may either resolve into a deep dermal or a superficial burn. If the burnt BSA is small (<10%), cooling of the burnt wound can be perfomed to the fore, while burns >10% TBSA should only carefully be cooled because there is a high risk of hypothermia (Krämer, 2010). Medium tempered running tap water (approximately 15–20 °C) is sufficient while ice cubes etc. should not be used. Cooling is often performed by laymen from the very beginning— paramedics should therefore critically evaluate if further cooling after arrival at the incident will harm the patient.
A maximum cooling temperature of 15 minutes should not be exceeded, while cooling of small BSA can help pain relief up to 30–60 min after trauma without. Specially manufactured burn dressings (such as Water−Gel®, Burn−Pack®) have been introduced to paramedic services as prefabricated cooling devices, but there remains concerns regarding hypothermia following application due to handling errors (e.g. prolonged application) with limited recommendations. These ready-to-use kits have an increasing significance for hypothermia following cardiopulmonary resuscitation (Adams and Roster, 2008).
After cooling the burn wounds, the patient should get an appropriate dressing and be wrapped to exclude cooling of the whole patient. A helpful reminder is to: ‘Cool the burn wound but warm the patient’ (Allison and Porter, 2004).
Dressings
Dressings are important for pain management and to prevent the burnt area from contamination. The burnt area should be covered with a cellophane type wrap without any external ointments or powders. The referring burn unit requires untreated wounds for definite assessment of the deep and extend of burn. The patient should be wrapped up in blankets or a duvet. Dressings also play a role for thermal balance—thus hypothermia should be prevented. Customary metal films (eg. Metalline®) can reduce the risk of undercooling as a further external measure.
Diagnosis of accompanying, life-threatening injuries
At the place of an accident, burnt patients by thermal injuries often show stable vitals even in the case of large burnt BSA. It should be taken into account that the burnt patient may have other coexistent injuries that lead to unstable vitals (Krämer, 2010).
Patients with both thermal and mechanical injuries require interdisciplinary prehospital and hospital care, thus management of these patients is hindered. Combined trauma occurs in up to 10% of all burn injuries, while the initial assessment of the burnt patient often raises mistakes by losing sight of the severe accompanying injuries (Kramer et al, 2010).
As a consequence, the primary approach to the burnt patient must be with respect to the algorithm of polytraumatized patients. The AcBC (Airway with cervical spine stabilization, Breathing, Circulation) rule should be obeyed. If suspected or diagnosed, the treatment must be with superior approach to the coexistent injuries, including emergency treatment in a trauma centre. The burn injury may then be treated secondarily (Cooke et al. 1996).
Special requirements for the prehospital treatment of patients with electrical burns are summarized in the section, ‘Electrical burns’.
A burn injury accompanying disorders must be prioritized and should be treated in accordance with criteria of Pre-Hospital Trauma Life Support (PTHLS©) (PreHospital Trauma Life Support Commitee in cooperation with the Committee on Trauma of the American College of Surgeons of the National Association of Emergency Medical Technicians, 2007):
Assessment of burn size and severity
To estimate the patient's burnt BSA, only superficial partial thickness (2nd degree, level a), deep partial thickness (2nd degree, level b) and deep burns (3rd degree and deeper) are calculated, while superficial burns (1st degree) are spared out from calculation of the burnt BSA.
The burn size is predominately important for prognosis and calculation of fluid resuscitation but plays a minor role for prehospital treatment. It does not have any life-threatening consequences for the patient if there are mis-calculations of the burnt BSA. Moreover, there are numerous studies about the lack of precise assessment of the extent at the scene of the accident (Hammond and Ward, 1987). Especially small burns <20% TBSA result in gross overestimation (Wachtel et al, 2000), while considerable underestimation is seen in burns >40% TBSA (Wachtel, 2000). Moreover, the percentage share of the surface of a hand is reduced with an increasing body mass index (BMI), i.e. a complete hand does not represent the customary assumption of 1% of the body surface anymore, but only 0.6% with a BMI of more than 31 (Berry et al, 2001).
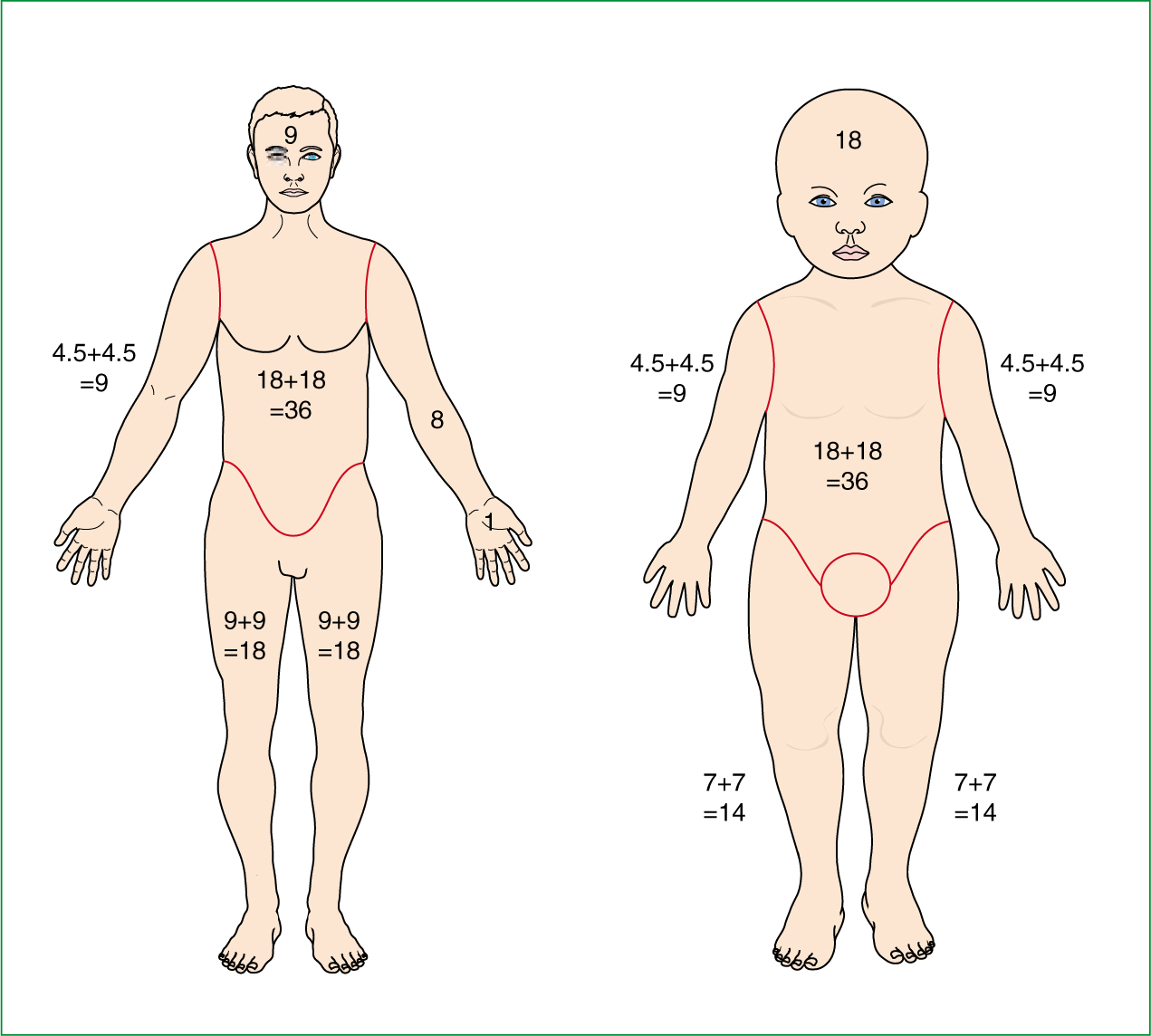
Nevertheless, the preclinical calculation of the burnt BSA remains essential with respect to current guidelines and can be done with the rule of nines according to Wallace who defined body surface areas of 9% or a multiple of ‘9’ (Kyle and Wallace, 1950). The head and arms each constitute 9% of BSA—the legs each 18%, the trunk 18% on each side. The remaining 1% is made up of the perineum, while the patient's palm of the hand gives orientation to estimate 1% BSA for spotted burnt areas (Figure 2) (Wallace, 1955).
| Superficial burns |
| A superficial burn involves only the epidermis and the upper part of the dermal papillae. The burn may appear bright pink or red in colour (erythema). Blisters may or may not be present. The texture is normal or firm and the area is very painful and hypersensitive to touch. On pressure, the burn area will blanch and capillary return will be brisk. In time, the erythema will fade and spontaneous healing will occur with no surgical intervention |
| Superficial partial-thickness |
| Blisters may be present or opened up. The area is very painful and hypersensitive to touch. On pressure, the burn area will blanch and capillary return will be brisk. This type of burn injury results in the entire epidermal layer being destroyed along with varying thickness of the dermis. Hence, a partial thickness injury can be either superficial or deep. Usually, a superficial partial thickness burn will heal itself by regeneration of the epithelial layer but will take longer to heal than a superficial burn |
| Deep-partial thickness |
| The substructures—sweat glands and hair follicles generally remain undamaged, but some can be affected. It is characterized by a creamy coloured base which is mottled in appearance. A deep partial burn where only the deeper substructure, sweat glands and hair follicles, untreated will leave scar tissue. Unfortunately, the depth of a partial thickness burn may take up to 7—10 days to declare it self as superficial or deep |
| Full thickness/deep burn |
| In a full thickness burn, injury occurs to the entire thickness of the epidermis, epithelial elements and dermal appendages. Spontaneous healing is not possible. If left, the area will heal by contraction, thus reducing function. A full thickness burn is characterized by its whitish leather appearance. It can also be brown, cherry red or charred black. It is firm and leathery in texture. Areas will not blanch under pressure. Initially, nerve sensation is greatly diminished or lost completely when the injury is sustained. The eschar of a full thickness burn is extremely inelastic and leads to compression of the underlying tissues as oedema occurs. |
Alternatively, the BSA can be estimated with the ‘half burnt/half not’ approach (serial halves: >1/2, <1/2, 1/4–1/2, <1/4) (Smith et al, 2005). If less than 50% BSA is burnt, the carer decides whether more than half of the half is injured, i.e. a body surface of between 25% and 50%. If the first and second halving makes it obvious that less than 25% of the body surface is affected, a decision can be made with another halving as to whether the burn injury is larger or smaller than 12.5% TBSA (Muehlberger et al, 2010). The latter technique is relatively new and has been shown to be effective in burn size estimation in prehospital care. In rare cases, chest wall escharotomy may be necessary in circumferential burns at the accident place due to insufficient excursions of the chest wall.
Airway management:
Accompanying inhalation injury has been shown to increase mortality from 2 to 35% in burn patients (Tredget et al, 1990; Saffle et al. 1995). Potential affection of the respiratory system by inhalation injury has to be assessed by signs for:
Inhalation injuries may rapidly reduce respiratory function and are accompanied by carbon monoxide intoxication which needs pure oxygen and airway management (Kramer et al, 2010). In this case, prehospital burn care predominately aims at airway management and the stabilization of vitals.
There are fixed indications for airway protection by intubation at the accident site which are in accordance to the ATLS® guidelines (Pruitt and Cioffi, 1995; American College of Surgeons, 2008):
Nevertheless, in a patient with a large burn having sufficiant spontaneous breathing under analgesia, intubation should not be done as a precautionary measure.
Intravenous fluid replacement and cannulation
The increasing fluid extravasation in burn injuries requires rational and individual fluid replacement. Infusion of balanced crystalloid solution (eg. Ringer's lactate or better maleate balanced crystalloid) can be started if the patient is cannulated, but must be started for burns with more than 15% TBSA and/or if time to hospital is more than one hour from the time of injury (Giessler, 2004; Krämer, 2010; Muehlberger, 2010).
Rational infusion management includes not hyperhydrating burnt patients—which is quite common due to mis-assessment of TBSA or lack of knowledge that the burn disease occurs delayed. It has been shown that up to 50% of crystalloid resuscitation fluids may end up as oedema (Crawford and Rask, 1996).
In burn injury treatment, the recommended fluid volumes are based on formulas for burn resuscitation that calculate the necessarily IV fluids due to capillary leak in correlation to the TBSA, the body weight and the time. They have regional modifications, while the most widespread formulas are according to Parkland/Baxter (Table 3) (Baxter and Shires, 1968; Baxter et al, 1973; Scheulen and Munster, 1982).
In general, the prehospital treatment period overlooks only a few hours of the 24 hour resuscitation period for burnt patients, thus calculation in a prehospital setting is less effective. Moreover, a reliable calculation at the scene of the accident is very difficult or impossible as neither the patient's weight nor the precise proportion of the burnt body surface is known. The authors recommend the estimated fluid volumes in Table 4.
Additional care should be taken not to over-infuse small, frail or elderly patients with a history of left ventricular failure. Fluid therapy should ideally be warmed (Warden, 1992; Myers, 1997).
The rationale for patient cannulation is fluid resuscitation and administration of titrated opioid analgesia. It is important that cannulation procedures do not unnecessarily extend the ‘on scene’ time. Cannulation can be limited to two peripheral lines, which should be positioned in unburnt areas if possible. In large burns, an intraosseus cannule (arm, tibia) may be an alternative to a central line. If a entral line is necessary at the accident place, a local excision of the burnt tissue may reduce contaminations.
Analgesia and medication
In general, burn injuries cause severe pain as far as the depth of the burn does not affect nerve endings at the subdermal level. As previously indicated, analgesia is best accomplished by cooling and covering the burnt area. Intravenous opioid can be titrated to make the patient more comfortable. Sedative medications can optimize patient comfort by having an anxiolytic effect. As a useful combinbination for prehospital treatment, S+-ketamine and benzodiazepine (e.g. Midazolam) can be recommended (Krämer, 2010).
Oxygen should be supplied using a mask in any case, while β-2-agonists can promote spasmolysis in toxic inhalation injury. No medication for pain relief should be given intramuscularly or subcutaneously, since fluid shifts are from vascular to extravascular space with unpredictable drug uptake.
Transport
All treatment should be carried out with the aim of reducing ‘on-scene’ time, thus delivery period of the patient to the appropriate hospital can be reduced. Due to potential hypothermia, the means of transportation should be preheated and the patient's body temperature monitored. The prehospital carer should orientate on certain criteria whether to deliver the patient to the nearest appropriate accident and emergency department or directly to a burn centre (Table 5). Communication with the hospital/burn centre should include the essential information only (age, sex, incident time and mechanism, ABC problems, relevant treatment) (Palmer and Sutherland, 1987; Slater et al. 2002).
The ambulance service central office should reserve an available bed at the burn centre/hospital if necessary, then transport by air or by land can be carried out.
Electrical burns
In burn injuries by electrical trauma, the immediate dermal burn can be accompanied by further organ disorders due to current conduction with an entry site at the point of contact and an exit site at earth contact. Electrical injuries are unlike other burns because of the extensive local tissue destruction at the point of entry and exit. Nevertheless, the definite extent of the electrical burn injury is difficult to assess at initial presentation and therefore should be treated as a major burn until proven otherwise.
Direct currents (DC) from lightning strikes deliver a counter shock that depolarizes the entire myocardium resulting in asystole, whereas alternating current (AC) produces greater damage because of titanic contractions (Aehlert, 1994). These contractions can make the person grip on to the cable, unable to release themselves. The current often needs to be turned off before relaxation of the hand muscles can occur.
The damage of tissues from electrical currents is caused by:
The majority of deaths from electrocution are due to two events:
Cardiac monitoring for arrhythmias should be considered for all patients presenting with electrical burn injuries. On the other hand, the estimation of the size of burn by measuring the skin surface burn is valueless (Aehlert, 1994). Considerably greater quantities of tissue may be destroyed beneath intact skin than is superficially apparent. The paramedic needs to ensure cervical spine protection and management of large bone fractures. The wounds in extremities with threatening compartment syndrome should be inspected repeatedly for signs of progressive damage.
Following the electrical burn injury, myoglobin is released from damaged muscle tissue and presents as myoglobinuria with dark brown or red colour of the urine. It is suggested that fluid replacement should be aimed at restoring vital signs and maintaining a urine output of two to three times the normal rate (2 ml/kg bodyweight/hour in children) (Kyle, 1950; Warden, 1992; Myers, 1997).
Chemical burns
Chemical injuries are commonly encountered following exposure to acids and alkali—including hydrofluoric acid, formic acid, anhydrous ammonia, cement, and phenol. Other agents that cause chemical burns include white phosphorus, elemental metals, nitrates, hydrocarbons and tar. Even though there are more than 60 000 chemicals available on the market, the potential deleterious effects of these chemicals on humans are still unknown (Edlich, 2005).
Most chemical agents damage the skin by producing a chemical reaction rather than hyperthermic injury. Although some chemicals exhibit considerable heat due to an exothermic reaction when they come in contact with water, the ability to initiate direct changes on the skin accounts for the most skin injury.
Nevertheless, specific chemical changes depend on the agent, including acids, alkalis, corrosives, oxidizing and reducing agents, desiccants, vesicants, and protoplasmic poisons. No general approach can be recommended. The concentration of toxic agent and duration of its contact primarily determines the degree of skin destruction. Some chemical agents underly systemic absorption and may harm internal organs.
The prehospital treatment of chemical burn injuries primarily aims at decontamination to stop the cauterizing process. Initial management of chemical burns consists of removing the saturated clothing, brushing the skin if the agent is a powder and finally irrigation with amounts of water. The rescuer must be careful not to come into contract with the chemical agent—self protection is necessary wearing gloves and eye protection glasses.
The decontaminating team requires detailed information about the causing chemical agent in order not to worsen the chemical burn. While some chemical agents have to be irrigated by water, some agents may cause further damage to tissue by heat of reaction when neutralized by irrigation. Care should be taken with the management of powder injuries, which may be worsened with water.
The one general recommendation for the decontamination of chemical agents is to get in touch with specially trained forces who will supply special equipment and summaries of chemical characteristics. The transferring hospital should be informed in advance about the suspected chemical agent to prepare safety measures and antidotes. If available, data regarding the probable chemical should be taken with the patient to hospital (Edlich et al, 2005).
Burns in children
Children display some separate characteristics which have to be obeyed for the treatment of burns. In their first year of life, the head constitutes 19% of the BSA, while the lower extremities each represent 12.5% (Figure 2) (Mlcak, 1998). Proportions come to change and are the same as adults by the age of 10 years. Fluid constitutes a higher percentage of body weight with consecutively increased needs for fluid, calories and protein (Kyle, 1950). The BSA to bodyweight ratio is greater than in adults, so that the same percentage of burn is more critical in children (Mlcak, 1998).
Children are more likely to develop hypothermia and approximately 30% of all children present post-burn hypertension due to release of vasoactive agents. While in adults, thermal injuries by fire are most common; in children, scalds are the most common cause of thermal burns. In children, fluid resuscitation is usually 6 ml/kg bodyweight/ % BSA until age of 12 years are recommended; while the formula from Shriners Burns Institute Galveston recommends calculation on the basis of the body surface with 5000 ml/m2 burnt BSA + 2000ml/m2 TBSA, one-half in the first 8 hours, remaining half in 16 hours, adjustment to urine output of 1 ml/kg bodyweight/hour (Kyle, 1950).
For prehospital treatment, the authors recommend estimate fluids as summarized in Table 4. Finally, a burn centre specialized for paediatric intensive care management should be approached because some burn units do not provide paediatric equipment (Mlcak et al, 1998).
Conclusion
Preclinical algorithm for prehospital care of the burnt patient can improve patient outcome and helps to prepare the primary carer sufficiently. There are some pitfalls in preclinical burn treatment which should be avoided. Cooling has to be in balance with body temperature to prevent hypothermia. Dressings should address sterile conditions but special ointments are unfavourable due to difficult secondary assessment in the burn centre. Combined trauma occurs in up to 10% of all burn injuries and can cause life-threatening injuries which have to be initially managed by a Level A trauma centre.
Fluid replacement can be made according to the guide discussed so calculation of resuscitation fluid can be done by the burn centre. No steroids (whether parenteral nor inhalative), antibiotics, diuretics, colloid solution (instead, there is an accompanying haemodynamic shock) should be administered at the preclinical setting.
Criteria for direct delivery of burn injuries to the burn centre have to be noticed, especially in the case of electrical and chemical burns. Thus, preclinical algorithm for prehospital care of the burnt patient can improve patient outcome and helps to prepare the primary carer sufficiently.
