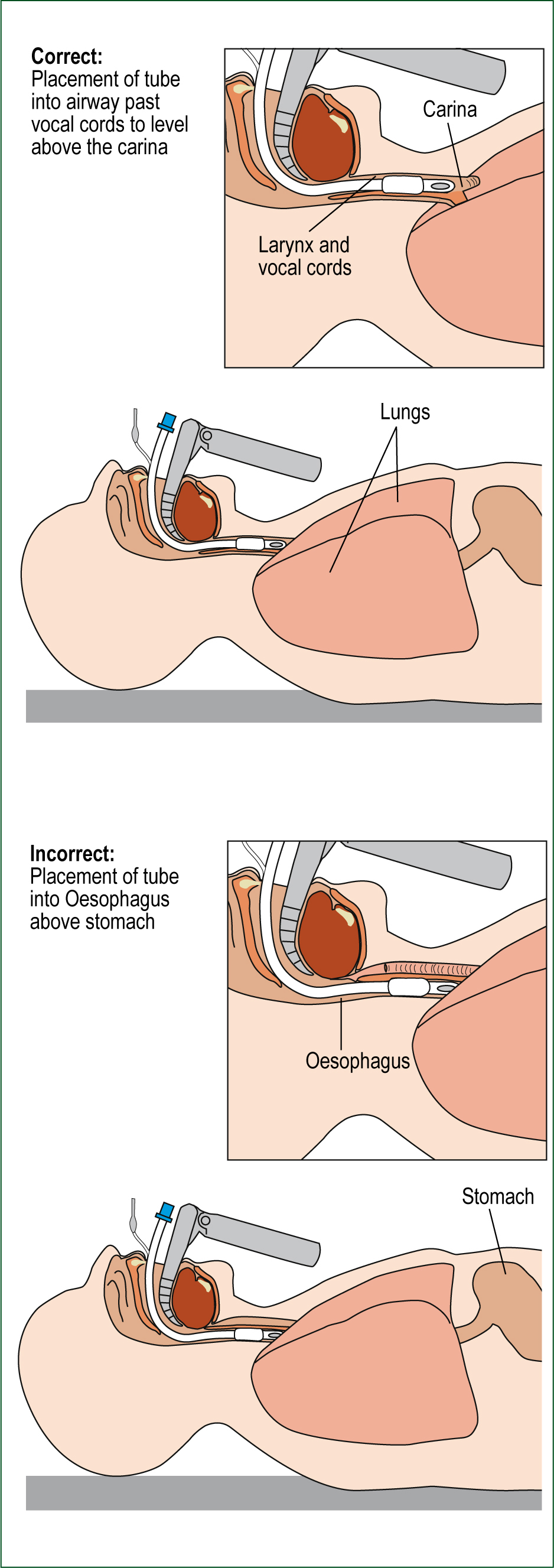
The maintenance of a patent airway is a requirement for every patient. In the context of critically ill patients, this is frequently achieved by the use of invasive airway devices. Endotracheal intubation (ETI) is considered the ‘gold standard’ of airway management in the hospital setting (Wang, 2007).
ETI is recommended by the Australian Resuscitation Council for airway maintenance and protection during cardiopulmonary resuscitation (Australian Resuscitation Council, 2010). Since the inception of paramedic practice over 30 years ago paramedics have performed ETI. Early research into paramedic pre-hospital ETI focused on skill performance, with research demonstrating ETI success rates of greater than 90% (Jacobs et al. 1983; Stewart et al. 1984).
Since the turn of the century, the performance of pre-hospital ETI by paramedics has come under increasing scrutiny. Researchers have generally found either equivocal or unfavourable outcomes associated with pre-hospital ETI by paramedics (Wang and Yealy, 2006). One possible explanation for these outcomes is the varying rates of adverse events that have been identified as being associated with paramedic pre-hospital ETI. The most serious of these adverse events is an unrecognised oesophageal intubation. The incidence of unrecognised oesophageal intubations by paramedics performing ETI in the pre-hospital setting has been reported to vary from 0–17% (Jacobs et al. 1983; Stewart et al. 1984; Pointer, 1988; Cobas et al. 2009). Intubation is an infrequently performed pre-hospital procedure and is most commonly performed for patients in cardiac arrest (Bendall et al. 2010).
The purpose of this study was to determine the incidence of unrecognised oesophageal intubations by paramedics in a metropolitan setting. We hypothesised that there would be a prevalence of unrecognised oesophageal intubation of between 1% and 2%.
Methods
Study Design
This study was a retrospective observational analysis of patients who were intubated in the pre-hospital setting by intensive care paramedics and transported to St George Hospital, Sydney, between 1 January 2007 and 31 December 2010.
Population and setting
St George Hospital is a level 1 trauma centre, seeing more than 59 000 presentations to the emergency department each year, and admitting around 20 500 patients. St George Hospital services a population of more than 250 000 people from southern Sydney, as well as being a tertiary referral centre for surrounding regions (New South Wales Health, 2010).
‘In order to perform ETI, intensive care paramedics must complete didactic lectures and manikin practice, as well as a 120-hour practicum placement in operating theatres’
The Ambulance Service of New South Wales is the sole provider of pre-hospital emergency medical services for the state of New South Wales. It services over 7.25 million people in New South Wales, distributed across an area of 801 600 square kilometres, resulting in over 1 million responses in 2010/11. The Ambulance Service of New South Wales operates a quasi-tiered service provision model. Basic life support level services are provided by paramedic ambulances, and advanced life support level care is provided by intensive care paramedics, who may respond as a member of an ambulance crew or as a single responder. Only intensive care paramedics are trained and authorised to perform ETI. Paramedics and intensive care paramedics treat according to protocols with no ‘real-time’ medical control.
‘Intensive care paramedics are able to perform non-drug facilitated ETI in any unconscious patient with an absent cough or gag reflex’
In order to perform ETI, intensive care paramedics must complete didactic lectures and manikin practice, as well as a 120-hour practicum placement in operating theatres, where they must successfully perform a minimum of 20 ETIs under the supervision of an anaesthetist. Once qualified, ETI skill maintenance requirements consist of supervised intubation of a manikin every 18 months. Other airway options available to intensive care paramedics include bag-valve-mask, oropharyngeal and nasopharyngeal airways, and laryngeal mask airways.
Intensive care paramedics are able to perform non-drug facilitated ETI in any unconscious patient with an absent cough or gag reflex. Confirmation of tube placement requires the mandatory use of a colorimetric end-tidal CO2 (ETCO2) detector and auscultation of the epigastrium and bilateral lung fields. Intensive care paramedics are also required to monitor patients for signs of an oesophageal intubation. Signs include: air leak; a need for excessive cuff inflation; the patient remaining hypoxic despite intubation and administration of 100% oxygen; or the presence of gastric distension. Rapid sequence intubation (RSI) is only performed in New South Wales by physician-staffed aeromedical retrieval teams. However, intensive care paramedics are able to administer sedation (morphine and midazolam) post-intubation if required to maintain intubation. Capnography waveform monitoring is used only by a small subset of intensive care paramedics, and no patient in this study received pre-hospitalcapnography waveform ETCO2 monitoring.
Human subjects committee review
Ethics approval for this research project was obtained from the Sydney South West Area Health Service Ethics Review Committee (RPA zone). Site specific assessment approval was granted by the Ambulance Service of New South Wales and St George Hospital.
Study protocol
Patient health care records from the Ambulance Service of New South Wales were used to identify patients who were intubated by intensive care paramedics during the study period and subsequently transported to the emergency department of St George Hospital. Each patient’s hospital medical record was then reviewed by at least one of the study’s authors. If endotracheal tube (ETT) placement appeared ambiguous, a second author would review the medical record. On the few occasions when this occurred, both reviewing authors reached agreement on ETT placement. For inclusion in the study there had to be documentation in the hospital medical record of at least one objective method of determining ETT placement (ETCO2, laryngoscopy or chest X-ray) being documented. This data was gathered by the authors using a standardised data collection form.
Outcome measures
The primary outcome was the proportion of patients with an unrecognised placement of the ETT in the oesophagus. All other tube positions that enabled ventilation of the patient to occur were considered as correct placement of the ETT in the primary analysis. The secondary outcomes were the proportions of each type of tube malposition (oesophageal, primary bronchus, laryngeal and pharyngeal).
Results
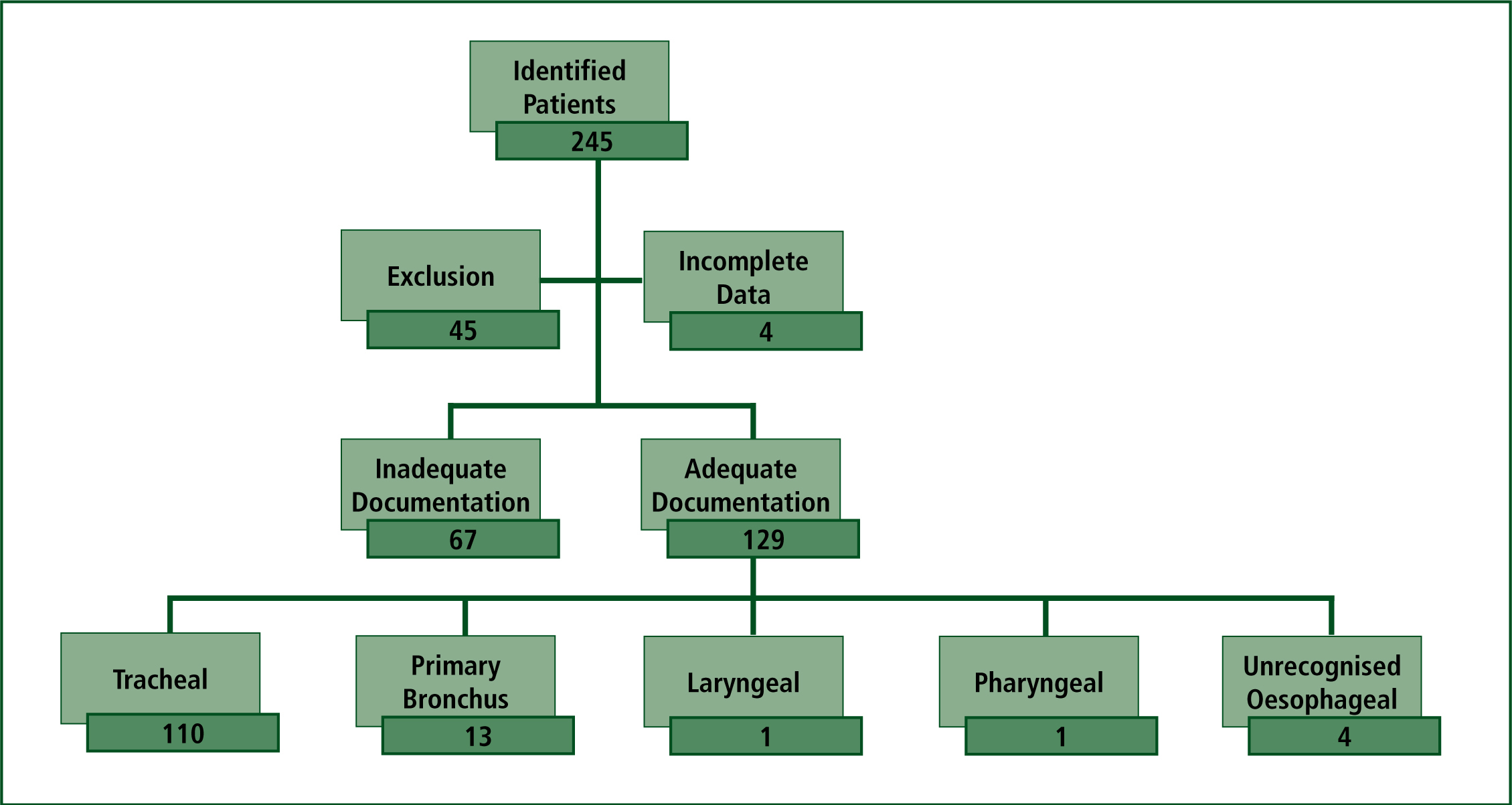
During the study period, 245 patients were identified as being intubated by intensive care paramedics. This was indicted by the marking of ETI data fields on patient health care records from the Ambulance Service of New South Wales and subsequently transported to St George Hospital. After cross-referencing these records with the hospital medical records, 45 patients were excluded because they did not have an ETT in-situ on arrival to the emergency department, or because they had airway management and/or ETI performed by an aeromedical retrieval team. Hospital medical records were unable to be located for four identified patients.
‘The 3.1% incidence of unrecognised oesophageal intubations found in this research study is appreciably lower than the 8–17% identified by some studies’
A total of 196 patients arrived at the emergency department with an ETT in-situ. The medical records of 67 patients who arrived with an ETT tube in-situ where subsequently excluded, owing to inadequate documentation, which did not allow an accurate determination of ETT position to be made. The remaining 129 patients had sufficient clinical information documented in the patients’ medical record indicating ETT placement. Of the patients included in the final analysis (n=129), 64% were male, 88% were in cardiac arrest, and the main condition was trauma in only 7% of patients. The age of patients ranged from 8 weeks to 96 years, with a median age of 72 years (interquartile range 56–81). Of these 129 patients, 4 (3.1%, 95% confidence interval (CI) 0.9–7.8%) had an unrecognised oesophageal intubation. The final ETT positions of the remaining 125 patients were 85.3% (95% CI 78–90.9%) located in the trachea, 10.1% (95% CI 5.5–16.6%) located in a primary bronchus, 0.8% (95% CI 0–4.2%) in the larynx and 0.8% (95% CI 0–4.2%) in the pharynx (Figure 1).
ETCO2 was the most frequently documented quantitative method of confirming ETT placement being used in 91% of the included patients. A chest X-ray was the next most common method (29%) followed by direct laryngoscopy (5%). Documentation of equal breath sounds and/or the absence of epigastric sounds on auscultation were not by themselves considered sufficient for ruling out an oesophageal intubation. However, it was documented 82% of the time, and assisted the authors to determine primary bronchial intubations. Patients frequently had more than one method for determining ETT placement documented (Table 1).
| Confirmation method | Frequency (%) |
|---|---|
| End-tidal carbon dioxide (ETCO2) | 118/129 (91) |
| Chest X-ray | 37/129 (29) |
| Laryngoscopy | 7/129 (5) |
| Auscultation | 106/129 (82) |
Discussion
The incidence of unrecognised oesophageal intubations identified in this study is consistent with the published literature (Jacobs et al. 1983; Stewart et al. 1984; Pointer, 1988; Cobas et al. 2009). The 3.1% incidence of unrecognised oesophageal intubations found in this research study is appreciably lower than the 8–17% identified by some studies (Katz and Falk, 2001; Jemmett et al. 2003; Silvestri et al, 2005; Wirtz et al. 2007; Cobas et al. 2009).
A possible explanation for this lies in the use of confirmatory devices. Three of these studies report sporadic or infrequent use of ETCO2 detection devices (Katz and Falk, 2001; Jemmett et al. 2003; Wirtz et al. 2007). Despite reporting an unrecognised oesophageal intubation rate of 8.5%, Silvestri et al (2005) identified that all of the 13 unrecognised oesophageal intubations occurred in a subset of patients for whom ETCO2 monitoring was not used.
During the study period, the Ambulance Service of New South Wales required the mandatory use of colorimetric ETCO2 detectors to confirm placement after all ETIs by intensive care paramedics. However, these detectors can produce equivocal results. The device is purple in colour when removed from its packaging. It changes to yellow when a gas mixture containing CO2 flows through it. The colour should change between yellow and purple during the respiratory cycle. If the colour is between purple and yellow (tan) then this is considered an equivocal result and may occur if the tube is not in the airway or perfusion of the lung is poor as occurs in cardiac arrest. To clarify this result it is recommended to deliver six more ventilations, and if the detector remains tan then the ETT is considered to be in the airway with low perfusion (Vargese, 2007). In studies where quantitative capnography waveform monitoring was utilised, the prevalence of unrecognised oesophageal intubation has been reported to be <1%.
In their study, Silvestri et al (2005) identified that when quantitative waveform capnography was used, unrecognised oesophageal intubations did not occur. This low prevalence was also found in other studies that utilised quantitative waveform capnometry (Ochs et al, 2002; Davis et al. 2004). Of the four cases of unrecognised oesophageal intubations identified in this study, a colorimetric ETCO2 detector was used in three instances. On the one occasion in which an ETCO2 detector was not used, the reason was not documented. Of the three instances where it was indicated that an ETCO2 detector was used, the patient health care records from the Ambulance Service of New South Wales documents a ‘tan’ and a ‘positive’ colour change on application in two cases, and there was no documentation of the colour change in the remaining case. Quantitative capnography waveform monitoring may better clarify ETT position in these equivocal cases, and the use of these devices may enable further reductions in the incidence of unrecognised oesophageal intubation to be achieved.
The reason for a 3.1% incidence of unrecognised oesophageal intubations cannot rest solely with the lack of quantitative waveform capnography. During the study period intensive care paramedics had colorimetric ETCO2 detectors available to assist with verification of ETT placement and their use was mandatory. The majority (88%) of the patients in our study were in cardiac arrest at some stage during their pre-hospital management. Colorimetric ETCO2 detectors have been found to be reliable in verifying proper ETT placement in patients who have suffered an out-of-hospital cardiac arrest, with Hayden et al (1995) demonstrating a 0.2% incidence of unrecognised oesophageal intubation in this population subgroup. The potential benefit of quantitative waveform capnography over colorimetric ETCO2 detectors is an important area for future research.
The positive correlation between quality of training and frequency of ETI skill performance to ETI success rates is well established (Garza et al. 2003; Wang et al. 2006). Wang et al (2005) demonstrated that paramedics are required to perform at least 15–20 ETIs to achieve baseline proficiency, and that in the US the average number of ETIs a paramedic student performs before graduation is 9.5. The Ambulance Service of New South Wales requires its intensive care paramedics to perform a minimum of 20 ETIs before graduation. After this time the only current requirement is a supervised manikin ETI once every 18 months. In our jurisdiction, the majority of our intensive care paramedics perform less than 10 intubations per year (Bendall et al. 2010). An incidence of unrecognised oesophageal intubation lower than 3.1% was expected given the initial high quality of paramedic ETI training and the mandatory use of colorimetric ETCO2 detectors. The lack of ongoing training requirements for intensive care paramedics may partly explain this study’s unrecognised oesophageal intubation rate.
In our study we have primarily defined ETT placement as ‘unrecognised oesophageal’ or ‘correct’ (Figure 2). In coming to this definition we have used the ability to ventilate the patient’s lungs as the standard to measure against. We are not discounting the iatrogenic harm that primary bronchial, laryngeal or pharyngeal ETIs can present for the patient. However, we are mindful of the signs and symptoms of oesophageal ETT placement versus ‘correct’ placement. During the review period it became apparent that primary bronchial ETT placement frequently was not determined until a chest X-ray was performed. In the case of the single pharyngeal intubation, the ETT was left in-situ for 30 minutes in the emergency department, effectively ventilating the patient, who was being mechanically ventilated before the ETT was replaced. If the patient’s lungs are being ventilated, then the devastating effect of hypoxic brain injury or death from an unrecognised oesophageal intubation is avoided.
We have included all patients who arrived at St George Hospital with an ETT in-situ in our cohort. While demographics such as age or clinical aetiology can affect an intensive care paramedic’s ability to successfully perform ETI, the methods and clinical skills required to verify ETT placement (and exclude an unrecognised oesophageal intubation), remain the same.
Limitations
The results of our study should be interpreted in the light of several limitations. The main limitation is the retrospective observational nature of this research. Data on ETT placement was extracted from medical records where identifying ETT placement was not the primary objective of the clinician at the time of documentation. As such, no method was universally used to determine ETT placement. Data was obtained from a single emergency medical services agency and only from patients transported to a single hospital. We only included patients who arrived at St George Hospital with an ETT in-situ in the study. In New South Wales intensive care paramedics are authorised to cease resuscitation efforts on patients who remain in asystole after completion of advanced cardiac life support protocols. Failure to respond to therapy may possibly be the result of a misplaced ETT.
Another important limitation is the exclusion of 67 cases due to poor documentation. Medical personal are much more likely to thoroughly document ETT placement in instances where misplacement is suspected, than in cases where the findings appear normal. This may have biased our primary outcome if these 67 excluded cases were less likely to have a malpositioned ETT, thereby overestimating the incidence of ETT misplacement. If we assume that there were no unrecognised oesophageal intubations among these 67 cases, the prevalence of unrecognised oesophageal intubation would then have been 2%.
Conclusions
The incidence of unrecognised oesophageal intubations in this study was consistent with other reports in the literature, although higher than expected given the training and equipment used in this setting. With the availability of confirmatory devices such as ETCO2 detectors and our current knowledge of the factors affecting ETI skill performance, a lower incidence of unrecognised oesophageal intubation should be achievable. An incidence of unrecognised oesophageal intubations of zero should be the goal of emergency medical services. This rate should be achievable; the key factors appear to be the use of confirmatory devices as well as the initial training and currency of an intensive care paramedic’s intubation skills. The prevalence of unrecognised oesophageal intubations may be reduced through recursive training programs and the use of quantitative waveform capnography. These interventions would be an important focus for future research.
This study was conceived and undertaken as a component of a Master of Health Science for Martin Nichols. Charles Sturt University, the Ambulance Service of New South Wales, the Ambulance Research Institute and St George Hospital have provided administrative support for this research project. No organisation or individual has provided or received financial support for it except for the authors’ performing their employment duties.
