LEARNING OUTCOMES
After completing this module, the paramedic will be able to:
If you would like to send feedback, please email jpp@markallengroup.com
Hyperkalaemia is classified as a high level of potassium within the blood and can be defined as a serum potassium level of more than 5.5 mmol/litre (Nyirenda et al, 2009; Nair and Peate, 2013).
Potassium is the commonest positive ion in the human body and is essential for muscle contraction through the conduction of nerve impulses via action potentials. Approximately 2% of the body's potassium is in extracellular fluid, with the largest concentration being within intracellular fluid.
Potassium is tightly regulated at 3.5–5.5 mmol/litre; this is maintained by a complex process involving the transfer of potassium between intracellular and extracellular fluid by the sodium-potassium pump (Simon et al, 2020). This pump is stimulated by beta agonists, insulin and theophyllines taking potassium into cells. Conversely, acidosis and cell damage decrease the activity of the pump causing an extracellular shift in potassium ions, thereby increasing concentration. The action of aldosterone within the kidneys increases the excretion of potassium, maintaining homeostasis in the long term, with an increase in potassium concentration stimulating the release of aldosterone (Kumar and Clark, 2017). These mechanisms ensure serum potassium levels are maintained at a level within the normal range even though daily potassium intake varies.
This case study discusses a patient presenting with hyperkalaemia in the community, following a request from the out-of-hours GP service for rapid emergency ambulance transport to hospital. It is based on an incident encountered more than 8 years ago and, even though paramedic practice has significantly evolved over this period, little has changed regarding paramedic guidelines concerning the recognition and treatment of hyperkalaemia within the prehospital setting (Eaton et al 2018; Brown et al, 2019). All names and places have been changed to protect confidentiality.
Case study
A two-person paramedic emergency ambulance crew responded to an emergency call at a local address for an older man who had attended his GP earlier in the day because of a general deterioration in his health. Blood tests taken at his GP practice were identified as abnormal by the out-of-hours GP later that day. Serum potassium was raised at 8 mmol/litre (normal range 3.5–5.5 mmol/litre), indicating hyperkalaemia. As these results were concerning, the out-of-hours GP called for an ambulance, stating that this patient was in danger of developing cardiac arrhythmias that could progress into cardiac arrest. The blood test results were conveyed to the emergency ambulance crew while they were en route to the patient.
When the ambulance crew arrived at the scene, the patient was waiting outside his home with his bags packed, ready to go to hospital. He was fully alert, orientated with good colour, breathing normally and appeared not to be in any pain.
It was decided to take observations within the emergency ambulance in a controlled environment where the patient could be assessed appropriately. All his observations were within normal parameters, except the electrocardiogram (ECG) which was consistent with hyperkalaemia, with tall peaked T waves and widened QRS complexes present (Houghton, 2019). He was conveyed to hospital safely without incident; nevertheless, given the severity of hyperkalaemia, this outcome could have easily been different.
Causes and pathophysiology of hyperkalaemia
Altered potassium regulation may have major consequences for muscle, nerve and cardiac function (Nyirenda et al, 2009). The primary concern for health professionals is altered excitability of cardiac muscle membranes, leading to cardiac arrhythmias and cardiac arrest. Therefore, quick and effective management is important.
There are many causes of hyperkalaemia, ranging from renal disease to trauma.
As insulin is involved in regulating potassium levels, low levels of insulin can result in elevated blood glucose levels and diabetic acidosis; serum potassium would also be raised (VanPutte et al, 2020). This transcellular shift with increasing circulating potassium can be caused by trauma (e.g. crush injuries), rhabdomyolysis, acute kidney injury, burns and treatment with drugs such as beta-blockers, non-steroidal anti-inflammatory drugs (NSAIDs), angiotensin-converting enzyme (ACE) inhibitors, digoxin and potassium-sparing diuretics (Sarwar, 2012; Sugand et al, 2019).
Foods rich in potassium such as tomatoes, chocolate and bananas can increase potassium levels within the body, precipitating hyperkalaemia.
Paramedics should be aware that pseudohyperkalaemia can be caused if a tourniquet is applied for more than 2 minutes, causing localised haemolysis, which can be avoided by monitoring tourniquet time (Sarwar, 2012).
Patients at risk
Patients who are more at risk of developing hyperkalaemia are those taking drugs that precipitate renal failure such as ACE inhibitors, NSAIDs, heparins, angiotensin-II receptor blockers and drugs that can cause an increase in serum potassium such as digoxin and beta-blockers.
Potassium levels in these patients need to be monitored closely especially at the start of their drug treatment and during illness (Wilkinson et al., 2017). Patients who have had a drug overdose, have cardiac pathology, have had surgery, have a decreased renal excretion of potassium (for example in mineralocorticoid deficiency as occurs in Addison's disease) or decreased renal function may also be at risk of developing hyperkalaemia (VanPutte et al, 2020).
Identification of hyperkalaemia
Hyperkalaemia is identified most accurately by venous blood tests; undertaking an ECG can also help practitioners identify hyperkalaemia and is a key part of assessment (Morris et al, 2008). Access to blood test results is limited in the prehospital setting, so an accurate and thorough patient history, including past medical history and drug history, is essential to identifying hyperkalaemia, and should be combined with an ECG.
Correct interpretation of the ECG is vital and, even if blood results are not to hand, an ECG can highlight hyperkalaemia of different severities: tall peaked T waves in a patient with a serum potassium level of 5.6–6.5 mmol/litre; a lack of P waves at 6.5–7.5 mmol/litre; widening of the QRS complex at 7–8 mmol/litre; and asystole and ventricular arrhythmias such as ventricular fibrillation with levels of 8–10 mmol/litre (Figure 1) (Sarwar, 2012).
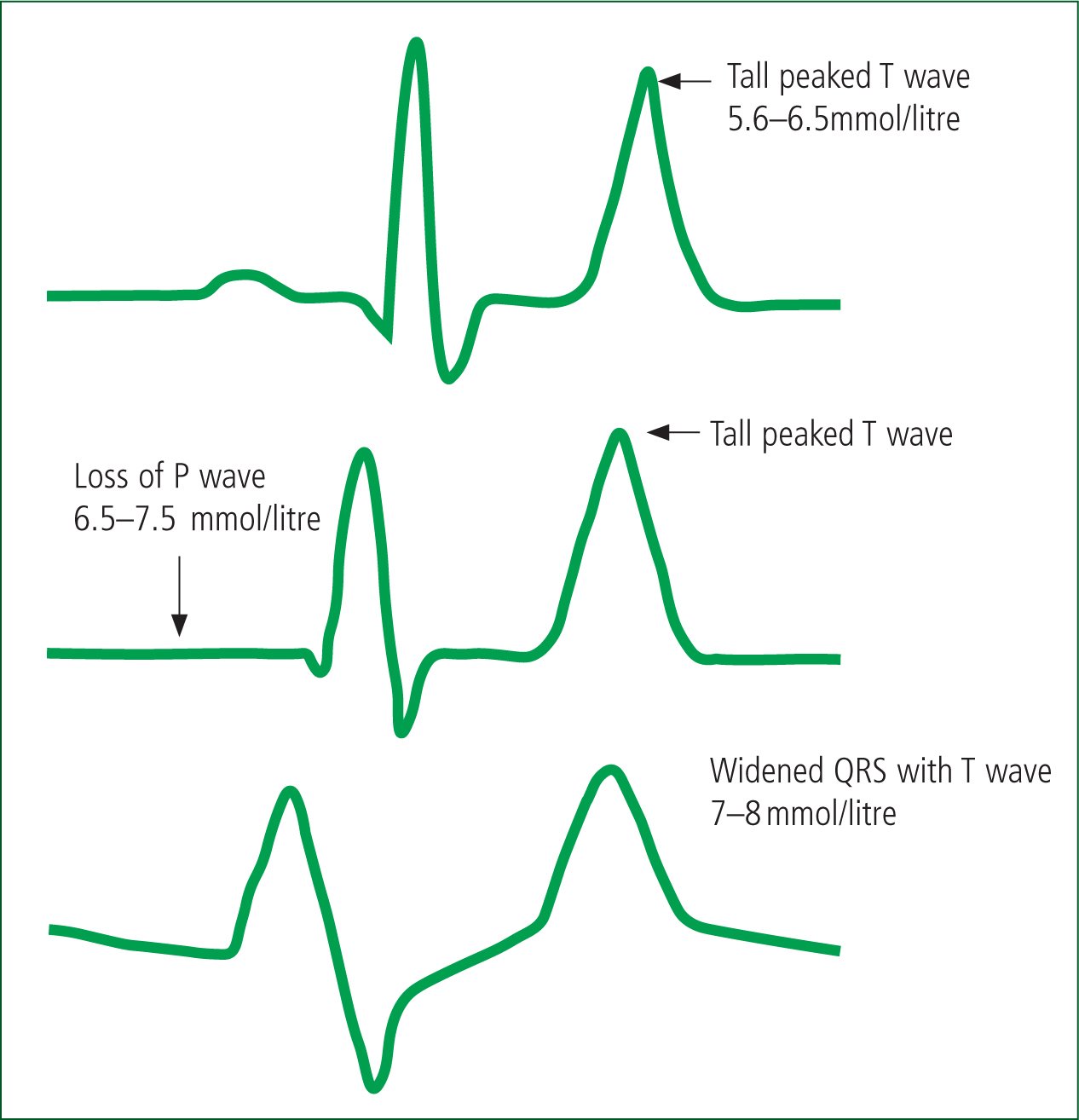
A guide to the ECG changes corresponding to the different serum potassium ranges could be drawn up to aid identification of the stage of hyperkalaemia. Combined with a detailed history and accurate clinical decision-making in the absence of blood tests, such a guide would be useful within the prehospital setting.
Treatment of hyperkalaemia
Treatment of hyperkalaemia includes protecting the myocardium with calcium as this antagonises the effect of potassium on the cardiac membrane, thus preventing further damage. However, this does not lower the serum potassium, so further intervention is required. Additional treatment includes insulin with glucose (preventing hypoglycaemia), as insulin binds to membrane receptors resulting in uptake of potassium intracellularly by the stimulation of the sodium-potassium pump. This treatment is achievable in the prehospital care setting only if a point-of-care urea and electrolyte blood test can be carried out, as it involves titrating infusions against blood results (Ahee, 2000; Joint Formulary Committee (JFC), 2021a).
Salbutamol can also be used to treat hyperkalaemia as it drives potassium intracellularly (therefore lowering serum potassium); it does this by binding to beta 2 receptors in muscle and liver cells, stimulating adenylate cyclase, which converts adenosine triphosphate to adenosine monophosphate (Ahee, 2000; JFC, 2021a).
Salbutamol can be given intravenously (IV) or nebulised and is quick-acting. It has a short half-life of between 30 minutes for IV and up to 2 hours if nebulised, which is particularly useful in the short term (Sarwar, 2012; JFC, 2021b). Salbutamol treatment for hyperkalaemia could be carried out in the prehospital setting as nebulised salbutamol is already used by UK ambulance services.
Sodium bicarbonate can also be used to correct causal or compounding acidosis (JFC, 2021a). However, it is slow acting and is mostly used to treat hyperkalaemia resulting from chronic renal failure rather than acute conditions (Sarwar, 2012).
Haemodialysis is recommended for severe cases of hyperkalaemia. While it is the most effective treatment, it cannot be provided in prehospital care (Ahee, 2000; JFC, 2021a).
Discussion
Within prehospital emergency and unscheduled care, there is some debate as to whether it is possible to diagnose hyperkalaemia without access to serum blood tests (Strange, 2013).
However, paramedics could potentially diagnose and treat hyperkalaemia using clinical observations combined with an in-depth clinical history and accurate ECG interpretation. Moreover, when severe hyperkalaemia has been revealed by a blood test and admission to the emergency department has been requested because of that result, early treatment could prevent the development of a poorly perfusing arrhythmia or even cardiac arrest.
Salbutamol has been proved to be equivalent to insulin and glucose treatment, with the most advantageous method of administration being nebulisation as this reduces risk to cardiac patients compared to IV administration; however, both routes can cause tremor and tachycardia if large, repeated doses are given (Ahee, 2000; Strange, 2013; JFC, 2021a).
Within the UK ambulance services, nebulised salbutamol has been used by critical care teams who have access to advanced medical support for the treatment of trauma-induced hyperkalaemia, such as crush syndrome with hyperkalaemia occurring in a similar but more severe way to pseudohyperkalaemia.
Within other ambulance services across the world, such as Southwest and Eastern Ontario in Canada, the consideration of beta 2 agonists in these circumstances is encouraged (Evans, 2009; Regional Paramedic Program for Eastern Ontario, 2021). However, non-medical independent paramedic prescribers within the UK can now use nebulised salbutamol to treat severe hyperkalaemia in cases of trauma-induced hyperkalaemia.
Even in medical cases of hyperkalaemia, the use of salbutamol is widely included as part of a doctor's treatment plan and is clinically indicated by the British National Formulary, although as an unlicensed indication (JFC, 2021a; 2021b). The use of a drug for an unlicensed indication is a legal, common practice but it must be based on sound scientific evidence (General Medical Council, 2021).
Salbutamol, alongside calcium gluconate, insulin and glucose in direct response to relevant ECG changes or a raised serum blood potassium result is the recommended treatment for hyperkalaemia (Raine et al, 2013). The use of nebulised salbutamol is also recommended within the Oxford Handbook for Medical School, which is a key text for medical students (Sugand et al, 2019).
While nebulised salbutamol is recommended in the first-line management of hyperkalaemia in other areas of healthcare, there are no established protocols within UK ambulance service clinical guidelines that enable paramedics to use it in the prehospital setting.
There is very little information within the UK ambulance services clinical practice guidelines for hyperkalaemia apart from relating to a crush injury or one of the reversible causes in a cardiac arrest, and they state that hyperkalaemia is ‘challenging to diagnose in the prehospital setting’ (Brown et al, 2019). The guidance does not consider the type of emergency call experienced within this case study where the patient had been confirmed to have hyperkalaemia by serum blood test results.
Providing emergency medical services (EMS), clinicians are competent to recognise hyperkalaemia through the history, signs and symptoms, and ECG, or if hyperkalaemia has been confirmed through venous blood tests. Paramedics already carry salbutamol but cannot currently use it to treat hyperkalaemia, and this contravenes the medical ethical values of beneficence and non-maleficence—doing good by promoting what is best for the patient and avoiding harm (Beauchamp and Childress, 2019). This issue could be addressed by allowing paramedics to provide treatment at the scene in the short term, preventing the patient from deteriorating. The traditional, core values of UK ambulance services are to ‘preserve life, prevent deterioration and promote recovery’ (Hines, 2003).
In addition, a blood test result showing a serum potassium level of 8.0 mmol/litre could be confusing for paramedics as they are unfamiliar with interpreting blood test results unless they have progressed to specialised or advanced clinical practice. Therefore, establishing the severity of hyperkalaemia from a blood test result may be difficult.
Conclusion
This experience of being required to convey a patient to hospital based on a previous abnormal blood test result indicating hyperkalaemia is not an isolated one.
Emergency medical services operate 24 hours a day and are increasingly used as emergency transport for medical cases referred by health professionals, in addition to the traditional ambulance role of responding to 999 calls.
Lateral thinking regarding recognising and treating cases of hyperkalaemia within the prehospital setting is required here, as there appears to be a case to start treatment that would benefit the patient and prevent this condition from progressing further.
With early intervention, hyperkalaemia can be safely managed in the short term until the patient arrives at hospital. It makes sense for ambulance services to consider the use of nebulised salbutamol in cases of hyperkalaemia (medical and traumatic) in the short-term, prehospital setting to prevent the patient from deteriorating and to promote their recovery. This could easily be made possible as emergency ambulances and rapid response vehicles already carry the drug and the equipment needed to nebulise it (oxygen and masks) and paramedics already know how to administer it.
This additional use of a drug already sanctioned for paramedic administration in acute asthma, exacerbation of chronic obstructive pulmonary disease and expiratory wheezing associated with conditions such as anaphylaxis would need to be approved by the authors of the UK ambulance services clinical practice guidelines; a suitable safe patient group direction would need to be developed and subsequently sanctioned for use by local ambulance trusts before prehospital administration (Brown et al, 2019).
The addition of nebulised salbutamol for the treatment of hyperkalaemia by paramedics to the UK ambulance services clinical practice guidelines, combined with a supplementary guide including the stages of hyperkalaemia on an ECG along with information on presentations, at-risk patient groups and serum potassium levels, would be welcome.
This effective and relatively safe treatment could significantly improve patient outcomes and ease paramedics' frustration at not being able to treat these patients effectively in the prehospital setting.

