An indication of critical illness is an imbalance in oxygen delivery to vital organs, resulting in hypoperfusion (Odom and Talmor, 2016). Because of hypoperfusion, anaerobic metabolic demand is increased, resulting in an increase in blood lactate levels (Soller et al, 2014). Elevated blood lactate indicates an increased risk of mortality, even in individuals who appear physiologically stable (Vincent et al, 2016).
In hospitals, lactate levels are commonly measured to assess adequacy of resuscitation, and are a key marker for evaluating patients with sepsis, where a lactate level ≥4 mmol/litre indicates septic shock (Casserly et al, 2015), and is a guideline for fluid resuscitation (National Institute for Health and Care Excellence (NICE), 2016). Similarly, it has been identified that lactate is useful in predicting mortality in trauma (Colon-Franco et al, 2017). Da Costa et al (2017) recognised that early monitoring of lactate levels in trauma patients identifies the adequacy of perfusion and the progression of organ failure, whereby lactate increments of 1 mmol/litre show increases in mortality.
Paramedics are often the first point of contact for patients presenting with sepsis (Groenewoudt et al, 2014) and trauma (Soller et al, 2014). Because of the drive to take care to the patient (Department of Health and Social Care, 2005), the paramedic role is evolving so these practitioners triage patients more effectively. However, it can be challenging for a paramedic to recognise the severity of a patient's condition, with studies reporting a mixture of paramedic diagnostic accuracy within a range of 12–78% (Wallgren et al, 2014; Green et al, 2016), resulting in a lack of optimal treatment and appropriate conveyance (Carberry and Harden 2016).
Tools such as the National Early Warning Score and Systemic Inflammatory Response Syndrome criteria have been developed to improve the recognition of deteriorating patients (Tusgul et al, 2017). Such tools, however, have limited sensitivity and diagnostic success in prehospital environments (AlQahtani et al, 2017).
Jansen et al (2008) postulate the use of lactate measurement as a tool in prehospital settings to improve triage and early treatment. However, the reliability of lactate measurement devices has been criticised for overestimating lactate levels (Lightowler and Hoswell 2016), which may result in inappropriate decision making and incur unnecessary costs to medical resources.
This literature review investigates:
Method
A literature search was conducted on several occasions between October 2017 and May 2018, using the Medline, CINAHL, Sciencedirect, Scopus and Academic Search Premier databases, which were accessed via EBSCOhost. The British Paramedic Journal was searched separately as it did not appear on any database, and was deemed a relevant contributor to the existing literature base.
Key words from a paramedic literature search filter devised by Olaussen et al (2017) were used, comprising of Ambulances OR Emergency Medical Technicians OR Air Ambulances OR paramedic* OR ems OR emt OR prehospital OR pre-hospital OR first responder* OR emergency medical technicians OR emergency services OR Ambulance* OR HEMS OR field triage. Medical subject headings identified topic-specific keywords for lactate, including: lactic acid OR lactates, and point-of-care testing; incorporating testing OR point of care OR testing OR bedside testing.
Inclusion and exclusion criteria were derived from past literature reviews that focused on a prehospital setting (Hilditch, 2015; Lightowler and Hoswell, 2016), where the quality of each article was assessed on publication, study design, population, intervention, comparison, and outcome (Table 1).
| Inclusion criteria | Exclusion criteria |
|---|---|
| Publication type: original research published in peer-reviewed journals |
Publication type: literature reviews, systematic reviews, editorials, comments, conference presentations and book chapters |
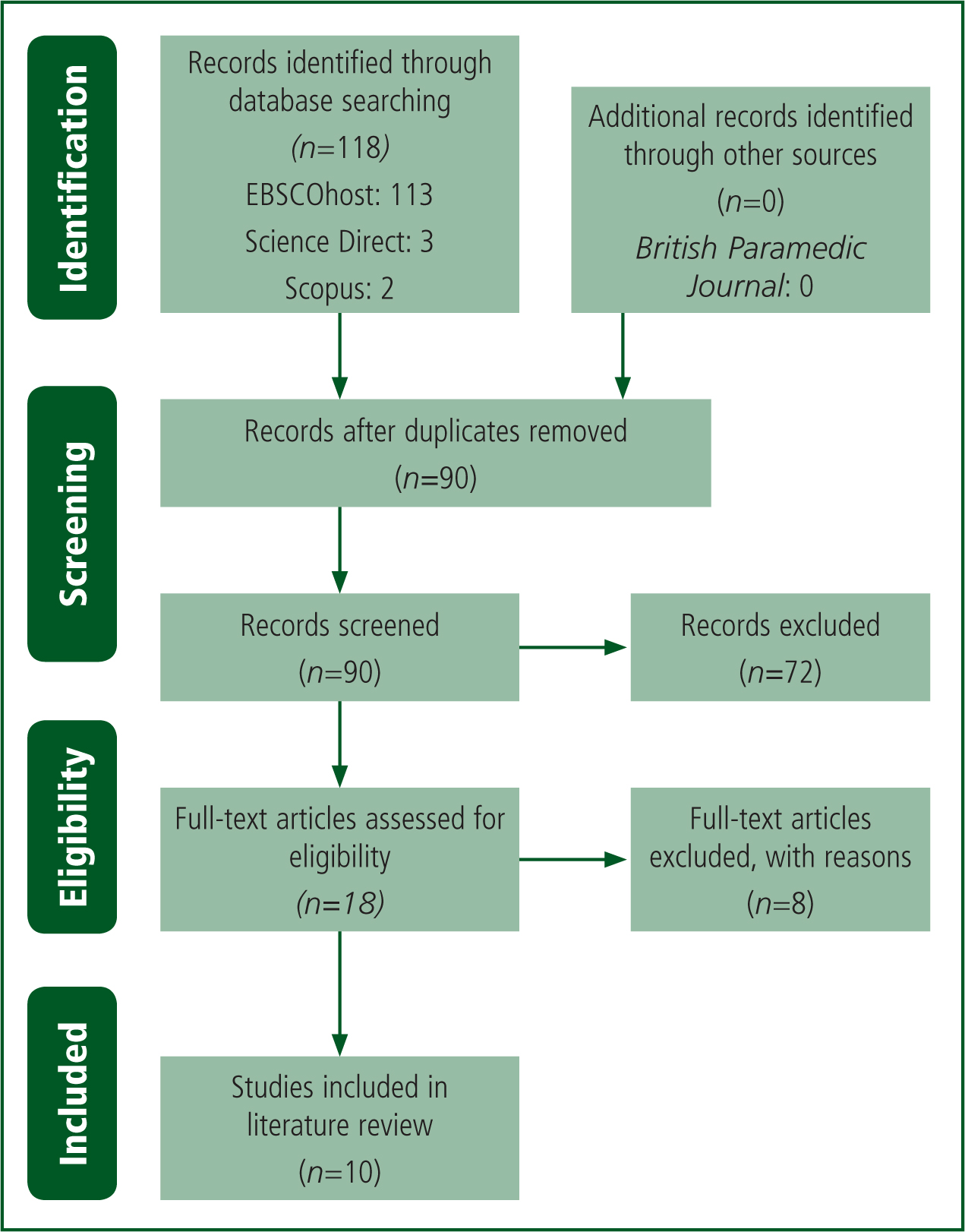
Initial search results yielded 118 articles, 23 of which were duplicates. A PRISMA method (Moher et al, 2009) was used to screen and identify eligible articles, of which eighteen were selected for text review; eight were excluded after full-text review, five because they examined the lactate test in hospital (González-Robledo et al, 2014; Walchok et al, 2016; Williams et al, 2016; Colon-Franco et al, 2017; Kim et al, 2017); one because it assessed the lactate of clinicians performing chest compressions (Abelairas-Gómez et al, 2017) and two because they lacked statistical methods to effectively measure an outcome, so yielded limited results for discussion (Younger and McClelland, 2014; Stanley et al, 2017). A final 10 articles were included in the literature review (Figure 1).
Results
Primary themes were derived based on the focus and results of each study. Three themes were identified: two as a result of patient presentation—traumatic injuries and medical shock—and the third investigating the accuracy of prehospital lactate measurement (Table 2).
| Study | Purpose | Method | Time frame | Sample size | Outcome measures | Relevant findings |
|---|---|---|---|---|---|---|
| Guerra et al, 2013 | Identify severe sepsis with a sepsis protocol including prehospital venous lactate measurements | Prospective study |
1 year | 112 | Diagnosis, pre- and inhospital treatment, and mortality | Mortality lower in those recognised by the protocol |
| Shah et al, 2013 | Diagnostic accuracy of prehospital lactate for predicting outcomes in paediatric trauma | Prospective study |
2 years | 217 | Identifying critical care need | Lactate and Glasgow Coma Scale significant in identifying if critical care required |
| Mullen et al, 2014 | Investigate lactate in medical patients undergoing prehospital transport | Prospective study |
18 months | 59 | Mortality and treatment | Sepsis identification significantly better in lactate group |
| Tobias et al, 2014 | Investigate the association of prehospital lactate with hospital mortality. | Prospective study |
14 months | 673 | Compare lactate to a critical illness score and mortality | Lactate measurement >2 mmol/litre in critically ill patients means they are more likely to require intensive care admission |
| Guyette et al, 2015 | Comparison of prehospital lactate and systolic blood pressure for predicting the need for resuscitative care in trauma | Prospective study |
18 months | 387 | Use of venous lactate and hypotension readings for escalating care in blunt and penetrating trauma | Lactate reading was more sensitive than systolic blood pressure in identifying the need for resuscitative care |
| Boland et al, 2016 | If prehospital clinicians can recognise patients with sepsis using a lactate meter | Prospective study |
2 years | 112 | Diagnosis, length of stay, and outcome at hospital | No significant relationships found |
| Brown et al, 2016 | Evaluate the diagnostic value of prehospital venous lactate within a trauma criteria tool | Retrospective study |
5 years, 8 months | 6347 | If lactate improves trauma level activation | Incorporating lactate into a trauma activation tool significantly improves triage |
| St John et al, 2018 | Whether prehospital lactate predicts need for resuscitative care in non-hypotensive trauma patients | Retrospective study |
14 months | 314 | Resuscitative care | Lactate predicts the need for resuscitative care in normotensive trauma patients, but no more than stroke index |
| Swan et al, 2018 | Comparing point-of care lactate with in-hospital lactate measurements | Retrospective study |
1 year | 269 | Association between prehospital and inhospital lactate | Poor association between lactate measurements, particularly as time between measurements increases |
| Swan et al, 2019 | Investigate if prehospital lactate levels predict intensive care unit admission and mortality | Retrospective study |
1 year | 253 | Mortality, admission and length of stay | No relationships found |
Discussion
Prehospital lactate in trauma
Shah et al (2013) identified that prehospital lactate values were the most significant indicator that paediatric patients would require critical care after experiencing trauma (P=0.01). The Glasgow Coma Score (GCS) was also significantly associated with the need for critical care (P=0.0001), although the GCS excluded 11 patients requiring critical care whose lactate levels did not. Furthermore, Shah et al (2013) identified that a 2 mmol/litre lactate threshold minimised misclassifying patients requiring critical care, with a sensitivity of 64% and specificity of 66%, so moderately triaged paediatric trauma patients. Sensitivity and specificity might be improved should lactate measurement be combined with other tools such as the GCS. However, the GCS in trauma patients aged under 4 years has been criticised as unreliable (DiBrito et al, 2018), warranting the potential use of lactate measurements to improve paramedic recognition.
Guyette et al (2015) identified similar results in adult trauma patients, discovering that a prehospital venous lactate measurement value of 2.5 mmol/litre or greater had a linear association for an increased need for resuscitative care need. The sensitivity of prehospital lactate was considerably higher than systolic blood pressure of ≤90 mmHg (96% vs 64%, P=0.01) in blunt trauma; however, it was lower and non-significant in penetrating trauma (79% vs 69%, P=0.42). Lactate was more sensitive than systolic blood pressure when measured within 15 minutes of the patient requesting an emergency ambulance (100% vs 59%), and remained similarly sensitive when patient contact was more than 15 minutes (89% vs 70%). These findings imply that point-of-care lactate testing may be warranted in identifying resuscitative care need over a systolic blood pressure of ≤90 mmHg. However, the study was limited as it included only patients with a systolic blood pressure of 70–100 mmHg.
St John et al (2018) further investigated the value of venous lactate testing in escalating resuscitative care in normotensive major trauma patients conveyed to a trauma centre by ambulance, excluding those with a systolic blood pressure of ≤100 mmHg. A lactate value of ≤2.5 mmol/litre was found to moderately predict the need for resuscitative care (sensitivity 74.6%, specificity 53.4%), but was no more effective than measuring shock index, so may not be a cost-effective method in assessing the need for escalating treatment.
St John et al (2018), however, argue that prehospital lactate testing might be effective for risk stratification, validating existing triage decision criteria and minimising false-negative observations. To support this claim, Brown et al (2016) evaluated the diagnostic value of incorporating prehospital venous lactate within a trauma criteria tool, integrating lactate values to modify the trauma tool, whereby a value of <2.5 mmol/litre indicated no trauma activation, 2.5–4 mmol/litre triggered a single physician response was needed, and >4250 mmol/litre signified a major trauma team should attend. The study showed that lactate values used in the criteria tool were better for classifying patients for the appropriate level of trauma care need (P<0.01), resulting in a 7.2% reduction in overtriage, and a 0.7% reduction in undertriage; it was found to have the greatest net benefit for deciding trauma activation.
Both studies (Brown et al, 2016; St John et al, 2018) were limited by their retrospective design, which prevented the researchers from establishing the type and severity of trauma diagnosed in the prehospital setting. However, findings corroborate previous studies.
Coats et al (2002) discovered that elevated lactate levels equated with severity of traumatic injury in a UK helicopter emergency service setting; Guyette et al (2011) further support the relationship of prehospital lactate in the recognition of critical care requirement, organ dysfunction and the need for inhospital surgery.
Prospectively, a lactate value of ≥2.5 mmol/litre indicates a need to escalate trauma care in adults to an appropriate trauma facility; however, this requires further research, particularly in the UK, to establish whether the inclusion of lactate would provide more benefit than existing tools. Similarly, a prehospital lactate cut-off level of 2 mmol/litre indicates the need for paediatric referral to critical care, reflected by the inhospital value of >2 mmol/litre that warrants paediatric intensive care admission (Bai et al, 2014).
Moreover, the existing major trauma tool in the UK (NICE, 2016) has been reported to overtriage 8% and undertriage 1.8% of major trauma patients (Clinical Audit and Research Unit, 2017). The UK major trauma guidance is similar to the trauma care tool established in the study by Brown et al (2016), and the inclusion of point-of-care lactate testing could further improve major trauma triage, further reducing overtriage and undertriage margins.
Prehospital lactate in medical scenarios
The evidence regarding prehospital lactate with medical patients draws a mixture of conclusions.
Tobias et al (2014) investigated the role of venous lactate measurement in predicting mortality in patients presenting with medical shock, identifying that a lactate reading of ≥2 mmol/litre had a greater association with mortality than a reading of <2 mmol/litre (5.2% vs 1.4%, P<0.01), and an admission to intensive care was more likely (14% vs 7.4%, P<0.01). Furthermore, a lactate level of ≥2 mmol/litre alone was found to be of modest sensitivity (76%) and low specificity (55%), and was shown to have similar discrimination as the prehospital critical illness score. When combined, however, sensitivity and specificity yielded statistical improvement, implying that the inclusion of lactate measurement might improve triage and escalation of care in medical patients.
Conversely, Mullen et al (2014) found capillary lactate measurement was not statistically significant in predicting mortality in aeromedical patients experiencing sepsis, liver failure, respiratory failure or cardiac arrest (P=0.64). A capillary lactate level of ≥4 mmol/litre, however, was found to increase the odds ratio of mortality (OR=2.1, 95% CI (0.3-13.8)). Furthermore, no statistical significance was found between the lactate and non-lactate measurement groups regarding escalation of care (P=0.11), although Mullen et al (2014) noted that more fluids and transfusions were given to patients without a lactate reading. Though the study applied some randomisation, measuring mortality and escalation of care within the same study may have confounded the results.
While Tobias et al (2014) and Mullen et al (2014) suggest that a lactate threshold of ≥4 mmol/litre may increase the likelihood of mortality, Swan et al (2019) found no significance between prehospital lactate and mortality, even at a lower lactate threshold of ≥2 mmol/litre. Swan et al (2019) noted that the overall mortality through the study period was 7.5%, which might have affected the results.
Furthermore, Guerra et al (2013) identified that incorporating prehospital venous lactate measurement into a sepsis protocol by paramedics reduced mortality in those meeting the criteria by 13.6% (P=0.0040); patients under the protocol were intubated less frequently (8% vs 35%, P=0.003) and, although these figures were not statistically significant, they were observed to receive accelerated antibiotic treatment (P=0.07) and more fluids (P=0.11). Unfortunately, the late acquisition of lactate devices at 6 months into the study, the small sample and the lack of comparison between lactate values and other vital signs renders it difficult to conclude whether measuring prehospital lactate values significantly impacted on patient management compared with the use of the sepsis criteria tool alone.
Moreover, Boland et al (2016) disagree with the findings of Guerra et al (2013); they found a capillary lactate reading was not significant in recognising sepsis, regardless of whether the patient was admitted to hospital or their length of stay. Nearly a quarter (24%) of the 84% patients admitted to hospital received a diagnosis of sepsis, where a lactate reading of ≥4 mmol/litre was found to have low sensitivity (19%). Interestingly, the study reported that a lactate level of <4.0 mmol/litre had a high specificity (91%) in ruling out sepsis.
The application of lactate testing in prehospital medical patients remains contentious in relating lactate measurement to recognising a specific medical complaint, treatment decision and mortality. Substantial corroborative evidence to suggest the application of prehospital lactate devices as a sole means to identify the severity of medical patient presentations is lacking.
A previous study by Jansen et al (2008), however, indicates that prehospital lactate is significantly related to mortality, giving better prognostic information than other vital signs. Indeed, the role of lactate measurement in hospital remains valuable in monitoring the effectiveness of resuscitation and risk of mortality, particularly with sepsis (Bai et al, 2014).
The established threshold of 4 mmol/litre is indicative of resuscitative measures, including intravenous fluid, for an improved patient outcome (Casserly et al, 2015), and is recommended for inhospital treatment by NICE (2017). Within the prehospital setting, Tobias et al (2014), Mullen et al (2014) and Brown et al (2016) allude to the importance of undertaking resuscitative measures when a lactate reading is ≥4 mmol/litre to reduce mortality; further research is warranted to investigate whether such a relationship exists and can be used to improve patient care and outcome.
Accuracy of lactate measurement
Swan et al (2018) sought to establish whether prehospital lactate measurements were reliably associated with inhospital lactate levels. They observed that prehospital lactate levels were higher than those in hospital (median: 3.0 mmol/litre vs 1.95 mmol/litre, P<0.001), and a prehospital lactate reading of ≥ 2 mmol/litre was more likely to result in lactate being measured in hospital (76.1% vs 23.9%; OR=3.18, 95% CI (1.88–5.37), P<0.0001). Furthermore, the reliability of prehospital lactate levels diminished in predicting in-hospital lactate levels over time.
Guerra et al (2013), however, noted a positive correlation (0.86, P=0.0001) between 22 prehospital and inhospital venous lactate measurements. Although the sample is small, the correlation illustrates that prehospital venous lactate may be a valid measure in establishing an accurate baseline.
Boland et al (2016) concur with the findings of Swan et al (2018), where a value below the given lactate threshold could rule out sepsis in the prehospital setting. Swan et al (2018) further noted that hospitals seldom investigated for sepsis when a prehospital lactate reading was below 2 mmol/litre. Moreover, inhospital point-of-care lactate studies acknowledge that a lactate reading of <2 mmol/litre does not prompt a sepsis diagnosis (Shetty et al, 2018).
Therefore, lactate measurement is potentially suitable in the prehospital setting as a suitable method for ruling out sepsis, thereby minimising unnecessary admissions. Future research could investigate whether such a strategy minimises risk to patients, and is cost effective for service provision.
Conclusion
Point-of-care lactate monitors have been accurately demonstrated to improve decision making and be cost effective in hospital, and these findings could apply in the prehospital setting.
Moreover, incorporating lactate measurements within established decision tools may improve triage; a lactate threshold of ≥2.5 mmol/litre could indicate the need to escalate trauma care to an appropriate facility, and ≥4 mmol/litre in medical patients might denote resuscitative measures should be undertaken to reduce mortality. Sepsis in particular, which already has an established inhospital threshold of 4 mmol/litre, could guide prehospital resuscitative treatment, although the evidence remains inconsistent and requires further investigation. Likewise, a threshold of <2 mmol/litre could aid in ruling out a sepsis diagnosis in prehospital patients where this is suspected, minimising unnecessary hospital admission.
It is important to emphasise, however, that lactate measurement alone would be insufficient as a diagnostic tool, and needs to be applied within the context of other clinical findings. Therefore, the use of lactate-measuring devices might be more appropriate for advanced paramedic practitioners, who are able to integrate additional information, knowledge and experience and refer patients appropriately.
Overall, the lack of evidence from limited literature with varying results might contribute to reasons why lactate measuring devices are not commonly used in prehospital environments. Future research on UK prehospital paramedic practice should focus on assessing the effectiveness of lactate measurements in guiding prehospital decisions in trauma and medical resuscitation.
Limitations
The studies reviewed were of a mixed quality. Small convenience sampling was predominantly used, and a range of lactate devices and methods of blood acquisition were employed in both prehospital and inhospital settings, which affect the reliability of lactate values. Additionally, the variety of study locations and health professionals reduce the results' applicability to the role of a UK paramedic. Finally, the mode of transport was a mixture of helicopter and ambulance, which could have affected response and conveyance times, and patient condition, which may have been more severe in those carried by helicopter than those in ambulances, altering lactate values.

