Pre-hospital care describes the care delivered to a patient out of hospital in a nominal emergency situation. This is the type of care that is normally associated with ambulances and ambulance clinicians. Some ambulance services have developed innovative volunteer models to care for pre-hospital patients while an ambulance is en-route. The premise is that even those with basic first-aid skills can save a life, in specific contexts. For example, in the United States there was a call from Government following the 9/11 terrorist attacks to enhance citizen readiness for, and resilience after, emergencies, resulting in the formation of community emergency response teams (Connolly, 2012). This model has been advocated for developing countries that have increasing numbers of patients but have insufficient resources to set up large emergency care systems (Sun and Wallis, 2012). Such first responder systems are particularly applicable and valuable to remote and rural areas where there are fewer ambulance assets (i.e. clinicians and vehicles) and the distances travelled can be much greater (Rahman et al, 2014)—this can increase ambulance response times, especially when coupled with poor road networks or other geographical challenges.
Within the UK, ambulance service community first responder (CFR) schemes recruit volunteers from local communities and give them the necessary training and equipment to deal with a limited range of medical emergencies. According to the Ambulance Service National Forum CFR survey there were 2 431 operational CFR schemes across the UK in early 2014, involving over 12 000 CFRs (personal communication with Scottish Ambulance Service (SAS) community engagement officer). Scottish CFR schemes first emerged in 2002 and now there are 137 schemes with over 1200 CFRs trained to at least ‘First Person On Scene’ level. They are an integral part of Scotland's rural and national health policy and strategy (The Scottish Government, 2008; SAS, 2011). The greatest number of CFR schemes and responders is in the north of Scotland, the largest geographical division within the SAS but with the lowest population density. The number of callouts across a sample of six Scottish CFR schemes (‘remote rural’ = 2; ‘rural area’ = 1; ‘small town’ = 1; ‘other urban area’ = 2; as defined by the Scottish Government Urban/Rural Classification 2011–2012) ranged from 2 to 74 in a one year period (2010–2011) (Roberts et al, 2014). Some 41% of Scottish CFR callouts (as recorded by the Advanced Medical Priority Despatch System; Cady, 2014) were to Category A, immediately life-threatening emergencies, and CFRs reached patients on average 10.9 minutes earlier than other resources (e.g. ambulances) (Cady, 2014).
Community first responders may encounter several difficulties during the assessment and treatment of their patients as they wait for an ambulance to arrive. The recording and interpretation of physiological data is a key challenge. Despite having patient report forms, these are often filled in retrospectively, the implication being that ambulance clinicians usually only receive a verbal handover. Physiological monitoring is carried out manually and intermittently, sometimes recorded in ink on the back of a protective glove. This introduces the potential for data loss and inaccuracy, and a break in the continuity of valuable clinical information. It can also be stressful dealing with a patient who has a life-threatening condition. Kindness et al (2014) conducted a stressor survey among Scottish CFRs and reported that they often felt helpless when managing patients. CFRs reported emotional demand not only on the most stressful callouts but also in more typical callout situations. This is comparable to the acute and chronic stress sometimes experienced by professional pre-hospital carers (Osofsky et al, 2011; Hegg-Deloye et al, 2014). It is reasonable to hypothesise that volunteer rural CFRs are potentially more susceptible to stress given their lower training level, greater distance from ambulance support networks and the fact that they also respond to life-threatening emergencies.
The University of Aberdeen inter-disciplinary MIME project (Managing Information in Medical Emergencies) aimed to develop technology to support rural CFRs during patient management (i.e. non-traditional, non-expert users of medical technology). The MIME project was funded by the University's dot.rural Digital Economy Hub, supported by Research Councils UK. The aim of this paper is to describe our MIME technology initiative in brief and then discuss the nature of our collaboration journey with the SAS. We propose that this model is one that others could replicate; the Knowledge Exchange (KE) sub-context to our research activities has been mutually beneficial. There are also wider implications for the arrangement of research activities within ambulance services, which have tended to lag behind the more formal organisation of research conducted in hospitals and in primary care contexts.
The MIME system
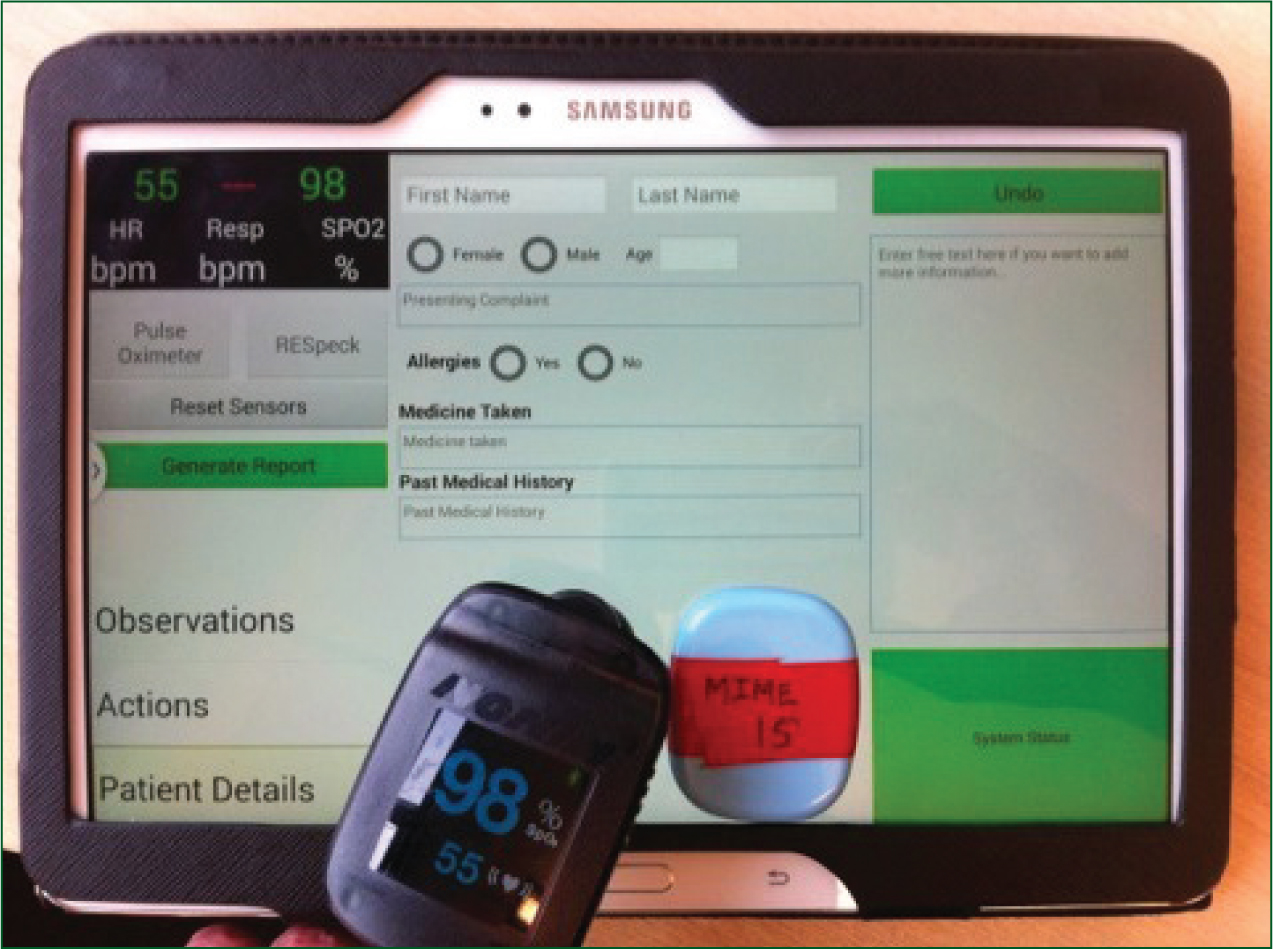
The MIME technology consisted of two key components: i) lightweight medical sensors that were simple to apply and operate (see Figure 1), and ii) novel software that presented these data very simply, facilitated the input of pertinent patient information (personal details, observations, actions), and generated a handover report at the press of a button.
Medical sensors
The MIME variant employed two lightweight, wireless medical sensors that delivered respiratory rate (RR), heart rate (HR) and blood oxygen saturation (SpO2) data. HR and SpO2 were generated by the Nonin 3230 finger pulse oximeter (Plymouth, Minnesota, USA), while RR was sensed by the RESpeck device (University of Edinburgh, Department of Speckled Computing, School of Informatics, Scotland), which attached to the abdomen using adhesive tape and used an internal accelerometer to record the cyclical movement of the abdominal wall with breathing (Drummond et al, 2011). Both sensors communicated their data using a Bluetooth® ‘Smart’ Low Energy wireless protocol to a Samsung Galaxy Note 10.1 2014 edition tablet. This maximised battery life, and the use of wireless sensors eliminated any risk of snagging, which is a common hazard experienced by clinicians moving patients in confined spaces. The addition of RR was particularly novel given that this vital sign is traditionally poorly monitored (Cretikos et al, 2008). Our proposed model was that the two sensors would be applied as early as was safe and practical during CFR patient management, and be utilised as a helpful adjunct to traditional manual assessment.
Novel software
Our software represented an entirely novel contribution to supporting CFRs, over and above the relatively straightforward task of implementing the existing patient report form in an electronic format. The system began by prompting consideration of scene safety and the appropriateness of applying the sensors. The sensors then paired with the tablet and the ‘Observations’ screen was presented to the user. Data such as level of response using the AVPU scale (Alert, responds to Voice, responds to Pain, Unresponsive; American College of Surgeons Committee on Trauma, 1993) were recorded simply by pressing large buttons on the user-interface, and then time-stamped. The same method was employed for the ‘Actions’ screen, which was used to record patient management procedures (e.g. applying high-flow oxygen). A third screen, ‘Patient details’, permitted the recording of patient personal data and the call code (i.e. the working diagnosis): integration of the system with ambulance service IT systems could potentially allow these fields to be pre-populated automatically.
‘Our software represented an entirely novel contribution to supporting CFRs, over and above the relatively straightforward task of implementing the existing patient report form in an electronic format’
Physiologic values were displayed continuously on the tablet screen and recorded to an internal database every 5 seconds, meaning that a large volume of data was accumulated continuously and very quickly. Clinical thresholds in the form of a traffic light system were applied to each parameter in order to alert the user to any deterioration; for this we employed physiologic limits associated with the National Early Warning Score (Smith et al, 2013). The system also incorporated some simple decision support; for example, if SpO2 dropped below 94% then it suggested considering applying high-flow oxygen in order to achieve an SpO2 of 94–98% (O'Driscoll et al, 2008). In the future, caution would be advised in patients with known chronic obstructive pulmonary disease.
At any point during patient management CFRs could press the ‘Generate report’ button, which created a handover report with sentence structure. Natural Language Generation (NLG) code, which was embedded within the MIME software, took the user-inputted observations, actions and patient details, as well as the automatically recorded physiologic data and interrogated it for patterns and trends to produce an English language report (Schneider et al, 2013a; 2013c). Such automated analysis was essential given that data for the three physiologic parameters were recorded every 5 seconds, rapidly building up a very large volume of data. Table 1 displays an example of MIME NLG system output based upon treatment and findings data.
| Treatment and findings |
|---|
| At 14:07 the patient's airway was obstructed, SpO2 remained constant around 84% for 1 minute, his breathing was slow and his breathing was shallow. |
Natural Language Generation software has been developed successfully for summarising data in other unstable clinical scenarios such as the neonatal intensive care unit (Portet et al, 2009). Within the context of future ambulance telecommunication systems the NLG report could be sent to the ambulance's cab-based terminal while en-route, and be uploaded to an ambulance service database for immediate central review, clinical governance and later audit and research.
Where implemented the MIME system could enable CFRs to capture a far greater volume of physiological patient data than is achievable currently. CFRs would also have an enhanced awareness of a patient's medical status through the automated identification of the subtle signs of deterioration and subsequently deliver timely, appropriate care (e.g. earlier recognition of need for high-flow oxygen). Within future models of care, ambulance clinicians and clinical advisors (located in control centres) could gain useful knowledge and information of the nature of the medical emergency responded to, which may also ensure appropriate resources are dispatched. Ambulance services would also have an improved patient record for the purposes of CFR audit, research and training. This is particularly important given that the CFR role is evolving but with a limited supporting evidence base. Evaluating the impact of CFRs is essential for on-going audit and for ensuring that each scheme receives appropriate training for their typical emergency callouts (which may vary greatly).
MIME research objectives
In order for us to design appropriate technology for CFRs we needed to understand pre-hospital care in detail. Our objectives were as follows:
The MIME system has been evaluated extensively since its inception in 2010. This has included sensor studies on healthy volunteers and pre-hospital patients (Mort et al, in press), research on the structure and appropriateness of NLG-generated reports compared with ‘expert’ reports generated by ambulance clinicians (Schneider et al, 2013a; 2013b; 2013c), and evaluations of the MIME user-interface where CFRs interacted with the system in mock patient scenarios. This has resulted in the development of a full prototype.
Collaboration journey with the Scottish Ambulance Service
Identifying an appropriate gatekeeper
Achieving our research objectives necessitated close interaction with potential pre-hospital technology user groups. This began by making contact with our local division of the SAS. Initially, a senior manager within the service was nominated as our key point of contact, which was appropriate in the early stages. However, the project grew in scale and activity, which placed greater demands on their time. In recognising this, responsibility was transferred to a new contact who was a clinical research paramedic (CRP). This individual was both clinically and research active, and attached to an academic research unit. The CRP post was already well established (McClelland, 2013), along with internal communication pathways. We found that this common appreciation of research made it easier to achieve a mutual understanding of our methods and needs.
Recruiting ambulance clinicians to MIME research
From our collective experience, the more in-person or personalised interaction with ambulance clinicians, the more likely they were to take part in research. For example, when recruiting ambulance clinicians to our sensor fieldwork with pre-hospital patients we arranged an evening visit to our local station. The study chief investigator attended and gave an informal talk about the study. Every clinician invited to the event volunteered to take part, with no dropout during the study. We provided participating clinicians with a small incentive in the form of a certificate of involvement in research, which was recognised by the SAS and contributed to their continuing professional development. Help from an area service manager based at the station was also crucial for coordinating and facilitating the event. Their involvement demonstrated the service's commitment to assisting the research process.
The first evaluation of our NLG software experienced a low ambulance clinician response rate (Schneider et al, 2013a). An electronic survey was employed and delivered to clinicians’ National Health Service (NHS) email addresses. A total of nine clinicians from NHS Highland completed the survey, which involved reading four different handover reports (i. paramedic written report; ii. CFR patient report form; iii. CFR verbal report; iv. computer-generated report), ranking them in order of preference and rating how useful, understandable and accurate they were. However, it was difficult to estimate response rate with any accuracy as the survey was distributed through a variety of internal SAS routes; establishing the total number of clinicians who received the survey proved problematic. Nevertheless, the nine responses were informative and helped us to refine the MIME system, but could not be interpreted as delivering generalisable results. Furthermore, in a CFR survey conducted by a MIME PhD student the invitation to the study appeared not to be distributed by the ambulance service to some CFRs. Future studies must ensure more robust and coordinated dissemination strategies to enable more accurate recording of response rates. Our most recent NLG evaluation (commenced December 2014) has achieved an 18% response rate so far (18 responses from a questionnaire sent to a random sample of 100 ambulance clinicians across NHS Highland), with the additional positive impact of a single reminder expected.
Low response rates to surveys by ambulance clinicians appear to be relatively common; indeed, involvement in research more generally tends to be poor. Hargreaves et al (2014) reported that paramedics voiced a number of barriers to taking part in clinical trials, including time pressure and the fact that conducting research is not their responsibility. However, the power of the survey from Hargreaves et al was in itself compromised by a low (32%) paramedic response rate. Anecdotally, methods that appear to improve ambulance clinician response rate to surveys include posting physical questionnaires (i.e. personalising with a name and address), providing post boxes at stations (to serve as a local, physical reminder) and providing stamped, addressed reply envelopes. Another strategy that we employed was to recruit an ambulance clinician stakeholder group, which we communicated with virtually using email, Skype™ and telephone. This was valuable for guiding the direction of the project, producing study materials (e.g. expert handover reports for software evaluations). For ambulance clinicians it meant that they could respond if and when they had the time, with little pressure.
Knowledge Exchange sub-context
Knowledge Exchange (KE) has been defined as:
‘…collaborative problem-solving between researchers and decision-makers that happens through linkage and exchange. Effective KE involves interaction between decision-makers and researchers and results in mutual learning through the process of planning, producing, disseminating, and applying existing or new research in decision-making’
Implicit to KE is the ‘two-communities’ metaphor/assumption (Wingens, 1990), which articulates that decision/policy-makers (the SAS) and researchers (the MIME team) effectively live in different worlds of knowledge, operation and reward, which neither appreciates in full (Graham et al, 2006). The presence of knowledge brokers in both the SAS (the CRP) and academia (a MIME research fellow with experience of pre-hospital research) meant that this knowledge divide could be bridged. We have described KE as a sub-context to our research activities as it occurred serendipitously (i.e. not by design) without a specific goal. In its strictest sense, KE commences with working together to scope, refine and ratify the research question from the outset. This ensures that the output of the research will have the maximum possible relevance and impact in the chosen technology deployment domain. However, this is not a simple process as each partner may have different views on what the research should deliver, and what is an interesting challenge to academics may not be an immediate priority for the partner organisation.
We consider that three types of KE took place in MIME, which we have termed i) Technology KE, ii) Operational KE, and iii) Research Process KE. Technology and Operational KE were more intuitive than Research Process KE; they mainly involved the more mechanistic transfer of information relating to sensor technologies and digital data capture mechanisms (academia to ambulance service), ambulance technology platform current status and future strategy (ambulance service to academia), and the day-to-day operation and objectives of the ambulance service (ambulance service to academia).
The transfer of Research Process KE was two-way, and not restricted to exchange around pre-hospital methodologies and ethical considerations (e.g. obtaining patient consent). For example, the organisation and governance of the research process was more developed in the university setting than it was in the ambulance service. Also, other NHS Boards in Scotland have more formalised procedures for managing research (i.e. physical research and development departments) than the SAS. The SAS is a ‘Special Health Board’ and receives no central research support funding: the health service in Scotland allocates in excess of £42 million annually to NHS Health Boards to support the research they undertake (for NHS staff time in individual studies but also for core research posts), with the level of funding reflecting the level of research activity. Under the current research support funding arrangements, the SAS could attract greater funding (including for research infrastructure) if it were able to engage in more research activity. The SAS is in its ninth year of collaboration with the Nursing, Midwifery and Allied Health Professions Research Unit at the University of Stirling. Both this and our MIME research demonstrate how successful future models of collaboration between NHS and Higher Education Establishments may look.
Conclusions
The University of Aberdeen MIME project aimed to develop technology to support CFRs attending rural pre-hospital emergencies. In the course of our research we came across challenges that we needed to negotiate. Sometimes we have had to work hard to explain our methods and the sequence of our development work to relatively research-naïve pre-hospital practitioners. However, we have also had to learn about ambulance service operation. The strategy that has delivered us most success has been ensuring effective and timely communication (in-person and virtual) with key individuals within the technology end-users' organisation. This was essential in order that the ambulance service understood and trusted our objectives and methods. Ultimately, this has enhanced the impact of our activities and ensured that our research was grounded in real-life pre-hospital care. Seely (2014) has advocated a ‘Boots on the ground’ philosophy for encouraging the adoption and diffusion of technological innovations in health care. We endorse this approach, as barriers are broken down and real views identified when meeting face-to-face with end-user organisations.
The University of Aberdeen plans to commercialise the MIME system in the future and this may involve a formal collaboration with the ambulance service. Such collaboration in innovation is actively promoted by the Scottish Government (The Scottish Government, 2012a) and there are successful recent precedents.

