Paramedics are often the first point of call for acutely unwell patients who present with a tachycardia. This tachycardia can be a natural physiological response, or less frequently, an underlying cardiac arrhythmia. Swift (2013) defines a tachyarrhythmia as: ‘where the pulse rate is greater than 100 beats per minute (bpm), with abnormal cardiac conduction present.’
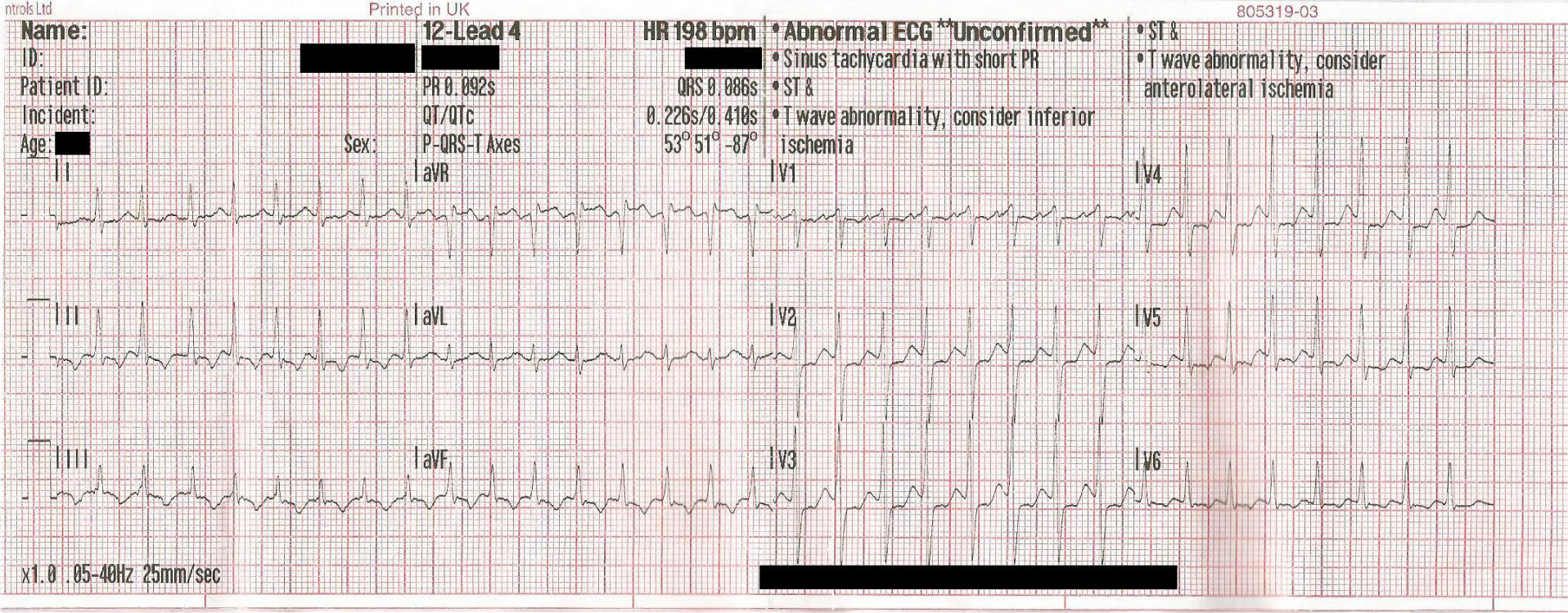
Supraventricular tachycardia (SVT) is a common cardiac tachyarrhythmia that has a prevalence of 2.29 per 1 000 people, with an occurrence of 35 out of 100 000 person-years (Orejarena et al, 1998). SVT is a transient narrow complex tachyarrhythmia (Figure 1) that is associated with a pulse rate of greater than 160 bpm, but typically 180–250 bpm, with an abrupt onset of palpitations. Other common symptoms include syncope, chest pain/tightness and shortness of breath (Whinnet et al, 2012). These typically result in an emergency call to the ambulance service.
There are two common types of SVT: atrioventricular nodal re-entry tachycardia (AVNRT) and atrioventricular reciprocating tachycardia (AVRT), which have slightly different pathophysiology (Wen et al, 1998). AVNRT is the most common cause and have an additional conduction pathway in the atrioventricular node, causing dual conduction pathways, with approximately 25% of the population having the additional pathway (Fogoros, 2012; Whinnet et al, 2012). In patients with AVNRT, an extrasystole triggers the arrhythmia while the faster pathway is refractory, causing a re-entrant circuit to form through the slower pathway and back up the faster pathway (Whinnet et al, 2012).
In the case of AVRT there is an accessory pathway, also known as a bypass tract, an example being the Bundle of Kent in the case of Wolff-Parkinson White (WPW) Syndrome. In WPW the pathway can conduct in both directions, but the majority of patients only have a pathway unable to conduct in antegrade direction (Fogoros, 2012). This accessory pathway allows for the formation of the re-entrant circuit and is characterised by a shortened PR interval on the ECG (Whinnet et al, 2012).
Treatment of SVT within the UK is guided by the Resuscitation Council (UK) (2011) tachyarrhythmia guidelines and the presence or absence of adverse features (Table 1). The paramedic plays an important role within the identification and early management of these patients, particularly in assessing the presence or absence of adverse features.
| Adverse shock features |
|---|
| Shock (systolic BP <90 mmHg, pallor, sweating, cold extremities, confusion, reduced consciousness) |
| Syncope/unconsciousness |
| Myocardial ischaemia (evidence on ECG) |
| Heart failure |
| Chest pain |
Currently within the UK the paramedic management is guided by the UK Ambulance Services Clinical Practice Guidelines (Association of Ambulance Chief Executives (AACE), 2013). Recommended treatment of SVT is through the vagal manoeuvres of Valsalva manoeuvre (VM) and carotid sinus massage (CSM) (AACE, 2013). The use of adenosine is currently not recommended in the treatment of SVT by UK paramedics in the UK Ambulance Services Clinical Practice Guidelines (AACE, 2013).
The aim of this study is to review the literature of the current evidence base for the treatment of SVT, with the aim of identifying whether the evidence supports the current UK paramedic management of SVT and whether this treatment could be enhanced.
Methodology
A research question was designed using the PICO process with a systematic Boolean search methodology. A MeSH (Medical Subject Heading) search was carried out on ‘paramedic’ and ‘pre-hospital’ to identify all commonly used words to ensure a thorough literature search. The key Boolean terms ‘AND’ and ‘OR’ were used to search the literature (Table 2).
| Paramedic |
AND | Supraventricular tachycardia |
AND | Vagal manoeuvre |
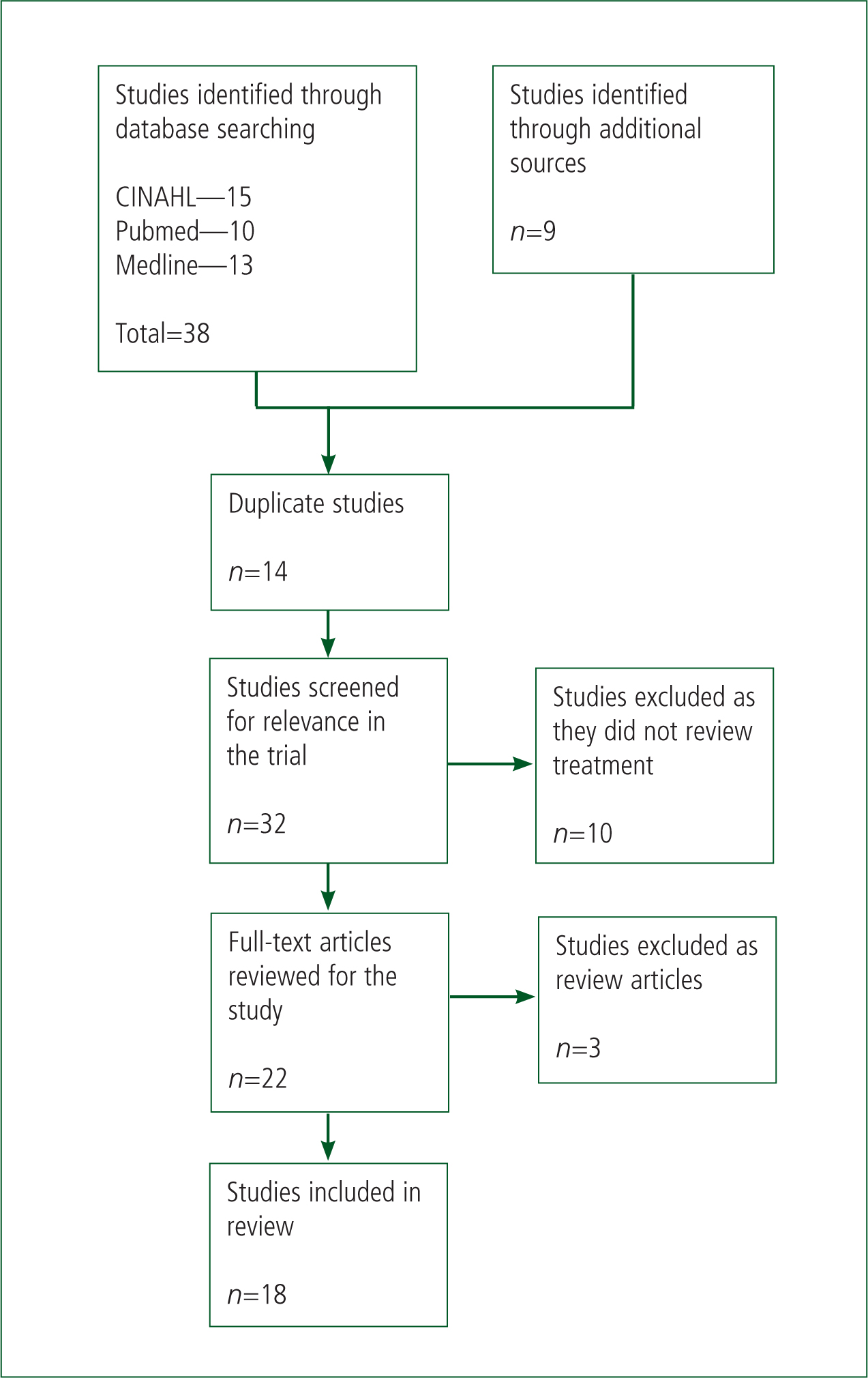
To ensure a comprehensive search of the literature available was achieved, several databases were searched (Figure 2). The databases chosen provided a thorough search of the available literature as they are focused on different aspects of medicine. CINAHL (Cumulative Index to Nursing and Allied Health Literature) provided papers which are relevant to nursing and allied health professions, such as paramedics, since 1982. Additionally, Medline and Pubmed provided access to papers published within medicine and biomedical sciences.
Studies were included within the review if they involved quantitative data and discussed the pre-hospital or emergency treatment of adults over 18 years of age with SVT. All articles also needed to be written in English. The review excluded papers or data based on the human dive reflex due to the inability to use this manoeuvre within the pre-hospital environment.
A search of the databases was carried out on 2 July 2015. Initial screening of titles identified 32 papers as possible inclusions for the study (Figure 2). Further screening removed an additional 13 papers. This was due to the papers being review articles, including papers which were already identified through the literature, or for not reviewing the treatment of SVT. This resulted in 18 papers being included within this article (Table 3). All papers included were screened using the Critical Appraisal Skills Programme (2013) checklists for the relevant study type.
| Study | Study design | Number of participants | Summary of study |
|---|---|---|---|
| Mehta et al, 1988 | Prospective study | 35 | Prospective study where patients were induced with SVT within the electrophysiology lab and vagal manoeuvres used in random order to test efficacy of manoeuvre. |
| McCabe et al, 1992 | Prospective audit | 37 | A prospective case series carried out over 1 year within an urban ambulance service. The study looked at the appropriate use of adenosine along with its associated efficacy and safety. |
| Gausche et al, 1994 | Prospective audit | 127 | Prospective audit over 6 months within an urban ambulance service to look at the safety and side effects of the use of adenosine by paramedics. |
| Furlong et al, 1995 | Retrospective audit | 31 | Audit of treatment of patients with SVT by US paramedics autonomously (without physician control/approval). |
| Lozano et al, 1995 | Prospective audit, cohort study | 244 | Prospective audit of large urban ambulance service in following the introduction of adenosine to paramedics with a historical control group to identify if it improved the care provided and was safe for use by paramedics. |
| Wittwer and Muhr, 1997 | Prospective audit | 74 | Audit of treatment of patients with SVT by US paramedics autonomously (without physician control/approval) following standard protocols. |
| Lim et al, 1998 | Prospective randomised case study | 148 | Prospective randomised case study to compare the vagal manoeuvres of Valsalva manoeuvre to carotid sinus massage. Randomisation was through selecting card and seeing treatment pathway allocated. |
| Wen et al, 1998 | Prospective study | 133 | Laboratory/clinic study on the efficacy of VM, CSM and HDR on induced SVT. All participants were healthy individuals with SVT induced three times for each manoeuvre. |
| Morrison et al, 2001 | Comparison study | 211 | A comparison study of patients with SVT treated by paramedics within the US. The control group was a retrospective audit of treatment only using vagal manoeuvres. The treatment group was a prospective study of the pathway following the addition of adenosine. |
| Goebel et al, 2004 | Retrospective audit | 179 | 10-year retrospective audit of patients treated by US paramedics for SVT. Looked at the appropriate use of adenosine through correct rhythm identification, treatment and occurrence of adverse features. |
| O'Rourke et al, 2004 | Prospective audit | 95 | Comparison of treatment of patients with SVT within a UK emergency department. Initial 15-month audit followed by the introduction of a treatment protocol and prospective audit over the following 6 months. |
| Riccardi et al, 2008 | Retrospective audit | 454 | Retrospective audit of the use of adenosine in an emergency department over 5 years. |
| Walker and Cutting, 2009 | Retrospective and prospective study | 19 | A retrospective audit on the efficacy of the Valsalva manoeuvre followed by a prospective observational study of the modified Valsalva. |
| Cabalag et al, 2010 | Multi-centre case controlled study | 68 | Observational study across several emergency departments of prospective SVT patients looking at the effect of caffeine on the efficacy of adenosine in treating SVT. |
| Sawhney et al, 2013 | Retrospective audit | 115 | A retrospective audit of patients who presented across four tertiary hospitals within London over 12 months. Study looked into the treatment of the arrhythmia as well as the follow up to see if patients were treated appropriately. |
| Gill et al, 2014 | Controlled trial | 120 | Controlled trial comparing verapamil to adenosine in the treatment of SVT. No mention of randomisation. |
| Smith et al, 2014a | Retrospective audit | 882 | Retrospective audit over 1 year to evaluate the effectiveness of the treatment for SVT. |
| Smith et al, 2015 | Retrospective audit | 823 | Cohort study with retrospective audit of the new treatment pathway following the introduction of adenosine compared to previous pathway with verapamil. Each audit took place over 6 months a year apart. |
Results
The literature search identified a total of 18 studies which were included within the review (Table 3), with five studies focusing on vagal manoeuvres (Valsalva manoeuvre, carotid sinus massage or human dive reflex), and the remaining nine looking at the use of adenosine. One study (Morrison et al, 2001) looked at both vagal manoeuvres and adenosine.
Vagal manoeuvres
Ten studies (Table 4) investigated the use of vagal manoeuvres in terminating SVT. The papers could be split into the pre-hospital group (four papers) and the hospital group (six papers).
| Author | Hospital or pre-hospital | Total study size* | Valsalva | CSM | p-value |
|---|---|---|---|---|---|
| Lozano et al, 1995 | Pre-hospital | 244 | Control—3/10 (30) |
0/27 | |
| Lim et al, 1998 | Hospital | 148 | 12/62 (19.4) | 9/86 (10.5) | 0.05 |
| Mehta et al, 1998 | Hospital | 35 | 19/35 (54) | 8/35 (22) | <0.001 |
| Wen et al, 1998 | Hospital | 133 | 63/133 (47.4) | 2/133 (1.5) | <0.00001 |
| Morrison et al, 2001 | Pre-hospital | 211 | Control—9/74 (12.2) |
0.04 | |
| O'Rourke et al, 2004 | Hospital | 95 | 5/95 (5.3) | 5/95 (5.3) | Not given |
| Walker and Cutting, 2009 | Hospital | 19 | 6/19 (31.7) | 0.09 | |
| Sawhney et al, 2013 | Hospital | 115 | 13/76 (17.1) | Not given | |
| Smith et al, 2014a | Pre-hospital | 882 | 99/358 (27.7) | Not given | |
| Smith et al, 2015 | Pre-hospital | 823 | Control—49/178 (27.5) |
0.27 | |
Numbers shown are the total number within the study that were confirmed as SVT and received the specified intervention and the number reverted by it, with percentages in brackets.
Total number of patients included within the study
CSM=Carotid sinus massage
Eight studies investigated the effectiveness of the Valsalva manoeuvre in terminating SVT, with efficacy rates ranging from 5.3% (O'Rourke et al, 2004) to 57.1% (Lozano et al, 1995). Within the hospital group reversion rates were between 5.3% and 54%. Wen et al (1998) and Mehta et al (1988) showed two of the highest reversion rates, with 47.4% and 54% respectively. Both of these studies involved inducing SVT in patients within the hospital setting. Walker and Cutting (2009) present a figure of 31.7% but have a low number of participants (n=19), suggesting statistically this study is not the strongest, despite a p-value of 0.09.
Within the pre-hospital group the reversion rates ranged from 4.4% to 57.1%. Lozano et al (1995) presented reversion rates of 30% in the control group and 57.1% within the treatment group, but with low numbers of patients involved of 10 and 7 respectively. These results are therefore insignificant compared to the larger pre-hospital studies by Smith et al (2014a; 2015), which present reversion rates of 21.4–27.7% across the two studies. The consistency and size of the studies by Smith et al (2014a; 2015) along with a p-value of <0.008 by Smith et al (2015) make these statistically significant.
Four studies with the hospital group investigated the use of CSM in the termination of SVT, with efficacy of the technique ranging from 1.5–22% (Table 4). The two studies (Lim et al, 1998; O'Rourke et al, 2004) where SVT was not induced showed reversion rates of 10.5% and 5.3% respectively. No pre-hospital studies investigated CSM on its own in reverting SVT.
One pre-hospital study (Morrison et al, 2001) and one hospital study (Sawhney et al, 2013) showed the use of both Valsalva and CSM in the termination of SVT. However, the results provide no breakdown of the individual method so add very little to this study.
Adenosine
Thirteen studies (Table 5) investigated the use of adenosine in reverting SVT and could be split into a hospital group of five papers and a pre-hospital group of eight papers.
| Author | Hospital or pre-hospital | Total study size* | 6 mg | 18 mg (1×6 mg and 12 mg) | 30 mg (1×6 mg and 2×12 mg) | Side effect rates | p-value |
|---|---|---|---|---|---|---|---|
| McCabe et al, 1992 | Pre-hospital | 37 | 23/26 (88.5) |
6/26 (23.1) | Not given | ||
| Gausche et al, 1994 | Pre-hospital | 127 | 71/84 (84.5) |
14/127 (11.0) | Not given | ||
| Furlong et al, 1995 | Pre-hospital | 31 | 15/31 |
25/31 (80.7) | 28/31 (90.3) | Not given | <0.05 |
| Lozano et al, 1995 | Pre-hospital | 244 | 38/98 |
61/98 (62.2) | 66 (67.3) | Not given | Not given |
| Wittwer and Muhr, 1997 | Pre-hospital | 74 | 46/74 |
61/74 (82.4) | 66/74 (89.2) | Not given | Not given |
| Morrison et al, 2001 | Pre-hospital | 211 | 24/72 |
18/39 (46.1) | 42/76 (55.3) | 10/76 (13.2) | <0.001 |
| Goebel et al, 2004 | Pre-hospital | 224 | 148/179 (82.7) |
Not given | Not given | ||
| O'Rourke et al, 2004 | Hospital | 95 | Group 1—44/58 (75.7) |
16/95 (16.8) | Not given | ||
| Riccardi et al, 2008 | Hospital | 454 | 331/454 |
399/454 (87.9) | 404/454 (89.0) | 377/454 |
Not given |
| Cabalag et al, 2010 | Hospital | 68 | 52/68 |
60/68 (88.2) | Not given | <0.05 | |
| Sawhney et al, 2013 | Hospital | 115 | 63/63 (100) |
Not given | Not given | ||
| Gill et al, 2014 | Hospital | 120 | 56/60 (93.3) |
42/60 (70) | <0.05 | ||
| Smith et al, 2015 | Pre-hospital | 823 | 115/129 (89.1) |
Not given | Not given | ||
Numbers shown are the total number within the study that were confirmed as SVT and received the specified intervention and the number reverted cumulatively by that dose, with percentages in brackets.
Total number of patients included within the study
Six studies (two from hospital group and four from pre-hospital group) showed the effectiveness of different doses of adenosine. A single 6 mg dose of adenosine was shown to have a reversion rate of between 33.3% (Morrison et al, 2001) and 76.5% (Cabalag et al, 2010). In contrast, the second dose of 12 mg adenosine showed reversion rates between 46.1% (Morrison et al, 2001) and 88.2% (Cabalag et al, 2010). A second 12 mg dose of adenosine had a reversion rate of between 55.3% (Morrison et al, 2001) and 90.3% (Furlong et al, 1995). Morrison et al (2001) showed consistently lower efficacy in reverting SVT compared to the other studies.
The remaining seven studies did not show a breakdown of individual doses but showed overall reversion rates of 75.7% (O'Rourke et al, 2004) to 100% (Sawhney et al, 2013).
Paramedic identification rates
Eight pre-hospital studies showed the accuracy in paramedic SVT recognition. These figures are where the doctors in the emergency department or conducting the trial agreed with the paramedic diagnosis of SVT.
The rate of paramedic SVT recognition ranged from 70.3% (McCabe et al, 1992) to 96.7% (Smith et al, 2014a). The largest studies in terms of participant numbers (Lozano et al, 1995; Morrison et al, 2001; Goebel et al, 2004) all showed recognition rates between 83.7%–95%, with the majority of recognition data being 83.7%–86.1%. This is supported through the study by Smith et al (2014a) who present a 98.7% paramedic recognition rate. Smith et al (2014a), Morrison et al (2001) and Lozano et al (1995) all present statistical data with a 95% confidence level, supporting the data as statistically significant, with Lozano et al (1995) further providing a p-value of <0.006.
Discussion
Vagal manoeuvres
The use of vagal manoeuvres as the first-line treatment in SVT is well supported by the literature through the use of Valsalva manoeuvre and carotid sinus massage (CSM). Both have subsequently been adopted into the Resuscitation Council (UK) (2011) tachyarrhythmia guidelines and also by the UK Ambulance Services Clinical Practice Guidelines (AACE, 2013). The advantage of vagal manoeuvres is that they are relatively simple and non-invasive without the side effects caused by adenosine.
The Resuscitation Council (UK) (2011) suggest that the Valsalva manoeuvre is effective in approximately 25% of SVT patients. This is consistent with the larger pre-hospital studies (Smith et al, 2014a; 2015) that show reversion rates between 21.4% and 27.7% for the Valsalva manoeuvre, suggesting that this is most likely the optimal figure that will be achieved through the technique. With the exception of Wen et al (1998) and Mehta et al (1988), the hospital studies generally showed lower reversion rates and were of much smaller study numbers than the pre-hospital studies.
The effectiveness of the Valsalva manoeuvre has been shown to be influenced by a number of factors including age, history of respiratory disease, pathophysiology of SVT and the technique used (Mehta et al, 1988; Wen et al, 1998; Smith and Boyle, 2009; Smith et al, 2009).
Wen et al (1998) and Mehta et al (1988) both showed that the effectiveness of the Valsalva manoeuvre is dependent upon the pathophysiology underlying the SVT. The Valsalva manoeuvre has a greater efficacy in terminating atrioventricular reciprocating tachycardia (AVRT) than atrioventricular nodal re-entry tachycardia (AVNRT) (53% versus 33%) (Wen et al, 1998). Within the pre-hospital environment and in the emergency department, the underlying pathophysiology is usually unknown, so will therefore have little impact within the pre-hospital environment.
One of the biggest influencing factors is the technique used for the Valsalva manoeuvre. AACE (2013) suggest getting the person to blow against a 20 ml syringe to push the plunger back, with a brief mention of being more effective in the supine position. Most paramedics are not taught the technique while in training, so it is something that is learnt on the road through experience, with a range of differing techniques used. Smith et al (2009) suggest that the best optimal position for achieving reversion using the Valsalva manoeuvre is the supine position, with exhalation achieving a pneumatic pressure of 40 mmHg for 15 seconds. Smith and Boyle (2009) showed that the required pressure of 40 mmHg can be generated by blowing against a 10 ml syringe, which is readily available within the pre-hospital environment. The majority of studies included in this review do no mention the technique used for the Valsalva manoeuvre, which could have an impact on the results collected.
The supine position is used to protect against the hypotensive effect of the manoeuvre (Smith et al, 2014b). This position was challenged by Walker and Cutting (2010), who showed a modified Valsalva manoeuvre using the Trendelenberg position achieved a reversion rate of 31.7%. They suggested that the Trendelenberg position achieved a greater vagal tone and hence the higher reversion rate. The study was small in size (n=19), so while statistically significant (p=0.09), the influence is reduced. Within the pre-hospital setting, the Trendelenberg position cannot be achieved using current ambulance stretchers. A study by Smith et al (2014b) into the vagal effects of both positions showed that there is no statistical difference in the vagal tone between the two positions.
Appelboam et al (2014) are currently investigating the effectiveness of a modified Valsalva through the Randomised Evaluation of modified Valsalva Effectiveness in Re-entrant Tachycardias (REVERT) trial in South Western England, which could further impact these findings.
When the Valsalva manoeuvre fails to revert SVT, the use of CSM is supported by both the Resuscitation Council (UK) (2011) and AACE (2013). CSM is achieved through a supine patient with extended head, and a point on either carotid artery firmly massaged against the spine for 5 seconds (Wen et al, 1998). CSM has been shown to have a much lower efficacy in reverting SVT compared to the Valsalva manoeuvre within the hospital environment of 5.3% (O'Rourke et al, 2004) and 10.5% (Lim et al, 1998). There were no studies that looked into CSM in isolation.
The use of CSM produces reduced vagal potency, especially when unilateral, and combined with vagal stimulation can reduce the desired vagal tone further (Mehta et al, 1988; Lim et al, 1998). The correct use of CSM is very operator dependent, based on locating the correct anatomical part and providing enough force (Lim et al, 1998). Paramedics are not routinely taught the use of CSM and thus are unlikely to be able to correctly carry out the technique.
CSM carries associated risks of plaque dislodge which can result in ischaemic strokes occurring (Adlington and Cumberbatch, 2009). The presence of plaque build up can be determined through auscultation of carotid bruits. AACE (2013) supports the use of CSM following auscultation of carotid bodies and no carotid bruits being identified. In the case presented by Adlington and Cumberbatch (2009), carotid bruits were absent but there was still significant plaque build up.
The use of human dive reflex is not currently recommended for treatment of patients with SVT within the UK (Resuscitation Council (UK), 2011). Within the pre-hospital setting the use of human dive reflex is unfeasible for practical reasons.
Wen et al (1998) and Mehta et al (1988) both studied the effectiveness of the techniques in patients who had SVT induced. With the exception of CSM within the Wen et al (1998) study, all their reversion rates are higher than the other studies. On the whole, pre-hospital reversion rates of SVT through the Valsalva manoeuvre are higher than the hospital studies. This suggests that there could possibly be a link to the effectiveness of the technique and the length of time the patient has been in SVT. As such, vagal manoeuvres, especially the Valsalva manoeuvre, may be significantly more effective at reverting SVT the sooner they are used following the onset of SVT. This, however, is an area which would require further research into looking at the relationship.
Adenosine
The use of IV adenosine is recommended where vagal manoeuvres have failed to revert SVT. In comparison to vagal manoeuvres, adenosine has a much higher efficacy at reverting SVT, with reversion rates of 33.3% (Morrison et al, 2001) to 100% (Sawhney et al, 2013). The efficacy of dose treatment increased with the subsequent 12 mg doses, compared to the initial 6 mg dose (Table 5).
Adenosine has been commonplace within the hospital treatment of SVT within the UK and worldwide. Initial reversion rates for 6 mg (72.9%– 76.5%) are lower than the subsequent 12 mg (87.9%–88.2%). The overall reversion rates presented following a maximum of 30 mg adenosine is between 75.7% (O'Rourke et al, 2004) to 100% (Sawhney et al, 2013), with the majority of total reversion rates being 88.2%–93.3% (Table 5). The hospital use of adenosine has shown that it is effective in the reversion of SVT.
Currently within the UK the use of adenosine is not within the paramedic treatment of SVT (AACE, 2013). Within the US and Australia it is part of the standard paramedic treatment. The effectiveness within the pre-hospital setting shows a wide range of reversion rates from 33.3% (Morrison et al, 2001) to 90.3% (Furlong et al, 1995). The efficacy of the initial 6 mg doses within the pre-hospital environment is lower than in the hospital (33.3%–62.1% versus 72.9%–76.5%), but the overall effectiveness is comparable (82.7%–90.3% versus 81.1%–100%). Two studies (Lozano et al, 1995; Morrison et al, 2001) showed reduced effectiveness of adenosine overall compared to the other pre-hospital studies. The reason for the lower effectiveness is unknown, as the dosage regime was the same.
Cabalag et al (2010) showed that recent ingestion of caffeine within the previous 4 hours reduced the effectiveness of the initial 6 mg dose (47.8% versus 76.5%). No significant impact was seen after 4 hours of caffeine ingestion or within the following 12 mg doses. This suggests that there are factors that can influence the potential efficacy of adenosine which could impact the reversion rates seen within studies, particularly pre-hospital studies where they would been seen quicker following the ingestion of substances like caffeine.
The increased effectiveness of adenosine compared to vagal manoeuvres in reverting SVT have led to some arguments that adenosine should therefore become the first-line treatment of SVT. While it is more effective it needs to be administered through a cannula within a large vein, ideally the antecubital fossa, and is commonly associated with transient side effects. Common side effects include chest pain, impending sense of doom and shortness of breath (Mallet, 2004; Riccardi et al, 2008). Riccardi et al (2008) and Gill et al (2014) reported side effect occurrence of 83% and 70% respectively. In contrast, the five other papers (McCabe et al, 1992; Gausche et al, 1994; Morrison et al, 2001; Goebel et al, 2004; O'Rourke et al, 2004) showed a lower occurrence of side effects ranging from 11.0%–17.3% of patients. There is no explanatory difference between the reporting rates, other than within the pre-hospital environment, whether these were recorded on the paramedic's paperwork compared to doctor's records within the emergency department.
The studies within the review all concluded that use of adenosine is safe and effective and those focusing on pre-hospital care suggested that it is safe for paramedic use. Adenosine is commonplace within the US paramedic scope of practice but US paramedics have more telemetric involvement of doctors. The identification rate of SVT (Table 6) by paramedics is slightly higher (79.4%–95%) for the larger studies. This is higher than that provided by Haynes (2001), who presents a misidentification rate of 25%. Hale et al (2011) suggest a higher identification rate of 89.8%, with the overall identification rate within this review being consistent with the Hale et al (2011) figure.
| Study | Paramedic SVT recognition | Statistics |
|---|---|---|
| McCabe et al, 1992 | 26/37 (70.3) | None given |
| Gausche et al, 1994 | 85/107 (79.4) | None given |
| Furlong et al, 1995 | 31/41 (75.6) | None given |
| Lozano et al, 1995 | Control—88/104 (84.6) |
OR—3.45 95% CI: 1.27–9.7 |
| Wittwer and Muhr, 1997 | 74/102 (72.5) | None given |
| Morrison et al, 2001 | Control—62/64 (83.7) |
95% CI: 0.42 (0.14, 0.72) |
| Goebel et al, 2004 | 188/224 (83.9) | None given |
| Smith et al, 2014a | 119/123 (96.7) | 65% CI: 91.5, 99.0 |
Within the UK paramedics are more autonomous practitioners compared to the US, and as such, within the US paramedics get doctor approval first prior to administration through telemedicine. Furlong et al (1995) and Wittwer and Muhr (1997) both looked at paramedic autonomous use of adenosine and showed the two highest reversion rates of 90.3% and 89.2% respectively within the pre-hospital papers. To further support this, Smith et al (2015) presented a reversion rate of 89.1% in the largest pre-hospital study, where paramedics used adenosine autonomously. This suggests that the use of adenosine autonomously by paramedics is as effective and safe as those where physician control is in place.
Haynes (2001) suggested that with misidentification rates of 25% and two deaths within an area following incorrect administration of adenosine to non-SVT patients, the routine use of adenosine by paramedics should be reviewed. In contrast to this, only one death was reported by the 12 papers focusing on adenosine within this study. Several studies reported adverse features but with only one death, including during the administration of adenosine to asthmatics and atrial fibrillation. This supports the safety of the use of adenosine within the pre-hospital environment by paramedics.
Current treatment in the presence of adverse features is through electronic cardioversion (Resuscitation Council (UK), 2011). A number of studies (McCabe et al, 1992; Gausche et al, 1994; Lozano et al, 1995) showed the safe use of adenosine and subsequent reversion out of SVT in those who presented with adverse features.
There have currently been no studies within the UK on the use of adenosine by paramedics, and while Furlong et al (1995), Witter and Muhr (1997), and Smith et al (2015) have shown autonomous use by paramedics is effective and safe, the continued management of these patients post reversion need to be discussed. London Ambulance Service NHS Trust (2013) is currently undertaking a clinical trial in the use of IV adenosine.
Implications for UK pre-hospital care
This review has looked into the current pre-hospital treatment and evidence around the clinical care of patients with SVT provided by paramedics, with the aim of impacting the care provided within the UK. Several implications for pre-hospital treatment of SVT by paramedics have been identified.
Firstly, paramedic identification of SVT has been shown to be between 83.9%–96.7% overall, which is slightly higher than the 75% suggested by Haynes (2001). The most common arrhythmias being misidentified were sinus tachycardia, atrial fibrillation and atrial flutter. This suggests that any training around ECGs as a result of improving recognition should place emphasis on diagnosing between these arrhythmias and potential importance of rhythm strips in diagnosing an arrhythmia. The use of a checklist or ECG guidance to assist may also be of use. However, it is important to note that none of these studies were UK based and therefore UK paramedic ECG recognition is unknown.
Secondly, the use of vagal manoeuvres needs to be looked at, with paramedics receiving formal training in the optimal technique for the Valsalva manoeuvre as this has been shown to increase the efficacy of the manoeuvre (Smith et al, 2009). This will potentially increase the number of patients who are reverted prior to arrival at hospital. This could also be impacted in the future by the REVERT study (Appelboam et al, 2014).
The pre-hospital use of CSM by paramedics should be re-evaluated due to the lack of ability of paramedics to identify carotid bruits and the absence of carotid bruits not excluding plaque build up. The low efficacy of the technique would have little impact on the pre-hospital reversion rates.
Thirdly, adenosine has been shown to be highly effective at reverting SVT and has been safely adopted into the paramedic clinical practice in the US and Australia, with a low occurrence of adverse incidents. The autonomous use of adenosine within the US and Australia also support its use within the UK by paramedics.
Some potential research areas have also been identified, such as investigating the effectiveness of the Valsalva manoeuvre and time since onset of SVT following on from observations of this review. Further research into the use of adenosine in the patient presenting with adverse features is also an area for future research.
Limitations
There have been several limitations which have impacted the review. Firstly, the evidence within the review has generally been from cohort or case-controlled retrospective or prospective studies (Class II-2a-2c) compared to randomised clinical trials (RCTs) (Hamer and Collison, 2005). The lack of RCTs within the current research base limits the findings of this review and would further support the current evidence base. The lack of evidence, particularly into the effectiveness of the vagal manoeuvres also limits the recommendations made.
The lack of UK studies also potentially influences the evidence, as while ambulance services from other countries are similar, they are distinctly different due to the reduced autonomy of paramedics compared to the UK paramedic.
Conclusions
The current treatment of SVT by UK paramedics does follow the evidence to a point, and the use of vagal manoeuvres is well supported by the evidence, though the use of CSM should be re-evaluated due to the potential safety impact. The use of adenosine by UK paramedics is supported through the safe and effective use by US and Australian paramedics, and would further enhance the treatment to these patients provided by paramedics within the UK.

