LEARNING OUTCOMES
After completing this module, the paramedic will be able to:
Rhabdomyolysis is a syndrome where skeletal muscle is broken down, resulting in the release of intracellular contents into the bloodstream, which can lead to systemic complications.
This can be caused by direct cellular injury or the depletion of adenosine triphosphate (ATP). Depletion of ATP leads to a failure of the sodium potassium pump in the membrane of the myocyte (muscle tissue cell). Failure of this pump causes an influx of sodium and calcium into the cell, causing the cellular membrane to break down and release its contents. This can be caused by direct cellular injury or depletion of adenosine triphosphate (ATP) due to ischaemia (Nellist and Lethbridge, 2013).
Of people aged >65 years, 30% will have a fall each year, with this rising to 50% in those aged over 80 (Tian et al, 2013). Patients who remain on the floor for a long time are at risk of developing rhabdomyolysis. It is similar to a crush injury but instead of an object ‘pinning’ the person down, tissue necrosis can occur at the point of contact and skeletal muscle is destroyed, releasing its contents into the bloodstream (Falls Action, 2018). This can eventually lead to crush syndrome, which encompasses rhabdomyolysis, lactic acidosis, hyperkalemia, dysrhythmias, renal failure, shock and even death.
Myoglobin is a muscle protein containing haem (which contains iron and allows the protein to carry oxygen) and is normally present in the circulation in a small quantity. This binds loosely to plasma, which prevents it from crossing the glomerulus in the kidneys. When excessive myoglobin enters the bloodstream from extreme muscle breakdown, it exceeds the binding ability of blood plasma, crossing the glomerulus and entering the renal tubules.
This causes dark (tea- or cola-coloured) urine; an excess amount of myoglobin in the urine is called myoglobinuria and this can happen from as little as 100g of skeletal muscle breaking down. When water is reabsorbed through the tubules, this increases the concentration of myoglobin, which leads to the formation of casts, which can cause an obstruction. Other mechanisms contributing to acute kidney injury (AKI) include renal vasoconstriction and oxidative injury caused by the haem group causing lipid breakdown (lipid peroxidation) and tubular cytotoxicity (Nellist and Lethbridge, 2013).
Signs and symptoms
The classic clinical presentation of rhabdomyolysis is weakness, muscle pain and tea- or cola-coloured urine (myoglobinuria). However, these signs are not always present. In fact, patients may not experience any muscle pain at all, and may instead be complaining of cramping and stiffness (Nellist and Lethbridge, 2013; Miller, 2019).
Other signs associated with underlying derangement in electrolytes and build-up of toxins include signs of infection like tachycardia, fever, altered mental status, nausea and vomiting, and abdominal pain (Nellist and Lethbridge, 2013; Miller, 2019).
Causes
Table 1 shows some of the causes (physical and non-physical) of rhabdomyolysis (adapted from Nellist and Lethbridge, 2013). It can be caused by anything (physical or non-physical) that causes either a direct or indirect depletion of ATP in the cell, which causes muscle breakdown.
| Causes of rhabdomyolysis | |||
|---|---|---|---|
| Physical | Non-physical | ||
| Trauma |
|
Metabolic syndromes |
|
| Occlusion, hypoperfusion |
|
Toxins |
|
| Excessive exercise/activity |
|
Infections |
|
| Electrical current |
|
Electrolyte imbalances |
|
| Hyperthermia |
|
Endocrine disorders |
|
| Autoimmune disease |
|
||
Source: adapted from Nellist and Lethbridge (2013)
Diagnosis
Along with the clinical signs and symptoms, rhabdomyolysis is diagnosed by a rise in creatine kinase (CK) levels five times higher than the upper limit of normal. Levels begin to rise 2–12 hours after the initial muscle injury, reaching their maximum between 24 and 72 hours. A reduction in these levels is usually seen within 3–5 days of alleviation of muscle injury.
Myoglobin appears in the urine when plasma concentration exceeds 1.5 mg/dl, but it is visible in the urine only when levels are 100–300mg/dl. It can be detected by urine dipstick at levels of 0.5–1mg/dl. However, myoglobin has a short half-life of 2–3 hours so it is rapidly excreted, and levels may return to normal in around 6–8 hours. This is why its measurement via dipstick is not a definitive diagnosis, as CK levels may remain elevated despite a drop in myoglobin levels.
It should be remembered that urinalysis dipsticks do not differentiate between myoglobin, haemoglobin and red blood cells so may be misleading if haematuria from trauma is a possible cause of darkened urine.
Hyperkalemia
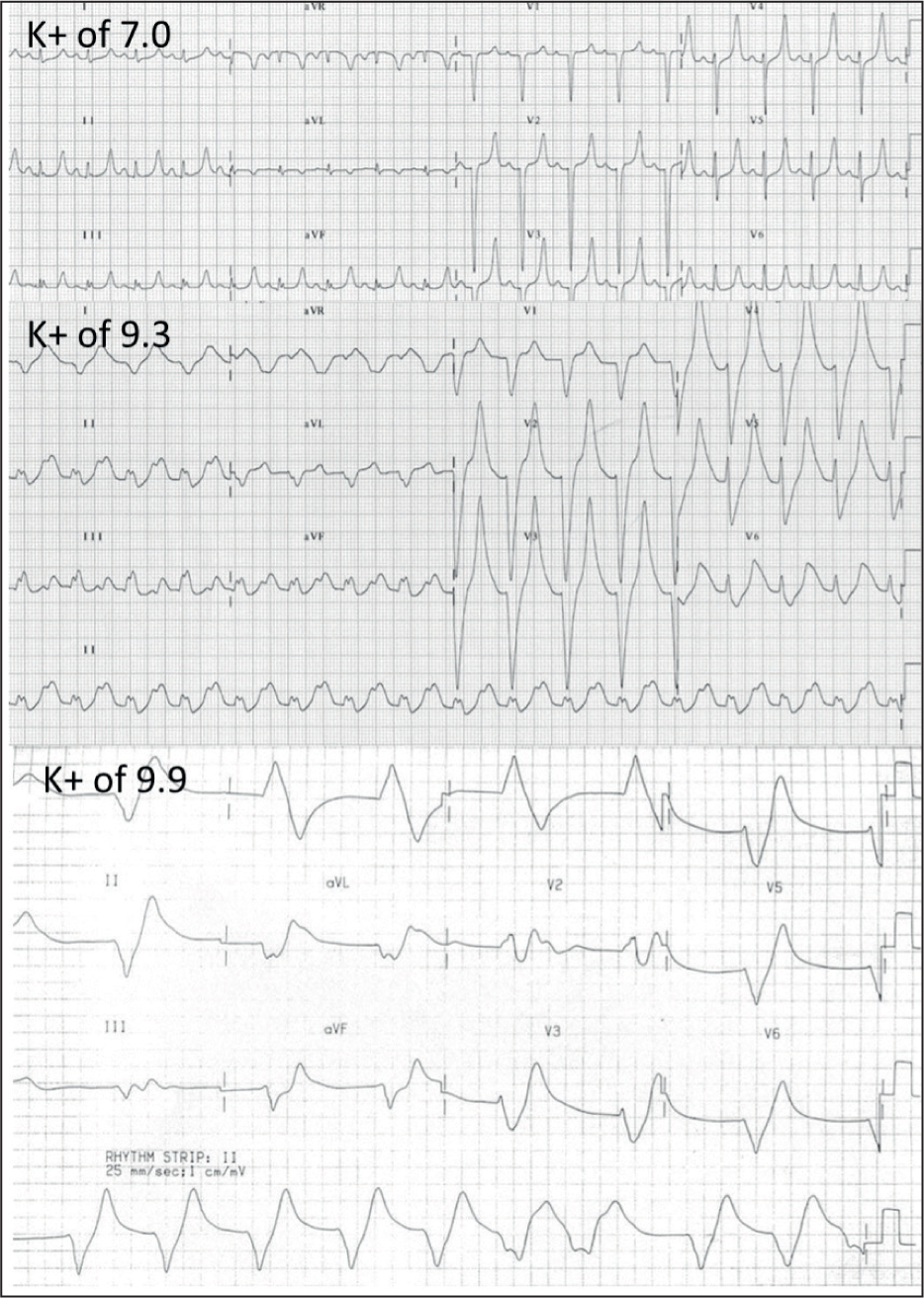
Practitioners should also be aware of increased potassium in the systemic circulation (hyperkalemia) because of damage and destruction of muscle cells. In the prehospital phase, the ECG is a helpful tool to recognise possible hyperkalemia.
ECG changes include peaked T waves and a prolonged PR interval. As levels rise dangerously high, there may be a loss of P waves, a widening of the QRS, the formation of a ‘sine’ wave, bradycardia and, eventually, a terminal dysrhythmia such as ventricular fibrillation (VF), asystole or pulseless electrical activity (PEA) with bizarre complexes (Nellist and Lethbridge, 2013) (Figure 1).
Risk factors for rhabdomyolysis in falls
A fall may occur for many reasons including weakness and frailty, environmental problems, musculoskeletal issues, and neurological and cardiac problems, and these may contribute to a patient not being able to get off the floor. If this immobilisation is prolonged, this can be a risk factor for rhabdomyolysis.
However, there are no specific guidelines on the time period when rhabdomyolysis is likely to occur because there are many variables. These include:
Although it is hard to state a definitive time to estimate when rhabdomyolysis may occur, an early study by Ratcliffe et al (1984) showed that, if an elderly person collapsed and stayed on the floor for as little as 1 hour, this was long enough to see significant rises in CK levels. Even though a significant rise in CK is not a predictor of AKI, it is important to note that shorter periods on the ground can see rhabdomyolysis beginning to manifest (Nellist and Lethbridge, 2013).
Prevalence of rhabdomyolysis in older people
There appear to be very few studies on the prevalence of rhabdomyolysis in Ireland and the UK.
McKenna et al (2019) investigated the prevalence and causes of rhabdomyolysis over 1 year in Tallaght University Hospital, Dublin. Rhabdomyolysis was found in 306 (1.7%) of the 18 297 admissions. The study found that ACS was the most common cause, followed by postoperative states, prolonged immobilisation, infection and seizures. Of these patients, 43% went on to develop AKI, and 50% of those died, showing how serious the condition can become. However, the age group of this study included any patient aged >18 years of age and rhabdomyolysis resulted from any cause, not specifically looking at older people aged >65 years and who had experienced a fall.
There appears to be only one study that looked at the epidemiology and prognosis of rhabdomyolysis specifically in the people aged >65 years, and this was a retrospective chart review in a single hospital in Pennsylvania in the United States over 4 years. In the 167 patients in the study, the most common cause of rhabdomyolysis was falls, with or without immobilisation (56.9%). The incidence of AKI was 68.9%, and there were 45 deaths (21%) over the 4-year study period. The study also found that a high number of medications (>8), presence of AKI and decreased glomerular filtration rate (GFR) were predictors of rhabdomyolysis and associated with lower survival rates (Wongrakpanich et al, 2018).
Statins were also found to be responsible for a small number of rhabdomyolysis cases in this study, so an elderly patient taking a statin is at a higher risk. In addition, GFR and renal flow steadily declines from the age of around 40, making older adults more susceptible to AKI than younger adults (Wongrakpanich et al, 2018).
Prehospital treatment
According to a systematic review, there are no management guidelines for the treatment of rhabdomyolysis, and no randomised controlled trials (RTC) have been conducted on the topic either (Chavez et al, 2016). Therefore, recommendations for its management have been drawn from retrospective studies and case reports. The mainstay of treatment is:
According to Chavez et al (2016), early and aggressive fluid therapy is the keystone of rhabdomyolysis treatment. This increases renal blood flow, thereby also increasing the excretion of the compounds that cause AKI.
Although literature comparing the different types of fluid resuscitation is lacking, Sever et al (2012), making recommendations for managing crush victims in mass disasters, said isotonic saline should be the fluid of choice and it should be infused at a rate of 1 litre/hour for 2 hours after injury and 500ml/hour after this. It is important to note that these recommendations are not based on RCTs.
Prehospital clinical practice guidelines (CPGs) in both Ireland (Prehospital Emergency Care Council, 2018) and Queensland Ambulance Service (2015) recommend fluid therapy for crush injury patients at 20ml/kg. This is equivalent to 1.6 litres for an 80 kg patient, and 2 litres for a 100 kg patient. The Queensland guidelines state that this should be given before release, and the St John's Ambulance New Zealand (2017) guidelines state that 20 minutes of resuscitation should be allowed before release or movement in preparation for reperfusion injury/release syndrome. They also state that 10 minutes before release, continuous salbutamol should be nebulised and 10% glucose be initiated, and, as the weight is being removed, that 50 ml 8.4% sodium bicarbonate and 1 g 6.8 mmol calcium chloride be administered over 1 minute in that order.
Could sodium bicarbonate help prevent AKI? It is plausible that using sodium bicarbonate to increase the urine pH may reduce myoglobin cast formation and lipid peroxidation, thus preventing AKI. However, it may also cause intracellular acidosis and volume overload, especially in patients with respiratory or circulatory failure. The most important point here regarding sodium bicarbonate use in this way is that there is a lack of RCTs and no studies have compared this to IV fluid therapy alone (Chavez et al, 2016).
Hyperkalemia
Management of potential hyperkalemia should include constant cardiac monitoring. Look for:
A review into the management of hyperkalemia in the acutely ill patient by Dépret et al (2019) has some recommendations potentially applicable to prehospital care. Beta-2 agonists such as salbutamol activate the sodium–potassium pump, transferring extracellular potassium into the intracellular space. This then decreases potassium concentrations in the circulatory system. They recommend 10mg of nebulised salbutamol as the first-line treatment to lower potassium levels (Dépret et al, 2019).
Queensland Ambulance Service (2015) has a dedicated hyperkalemia CPG, which states that continuous nebulised salbutamol can reduce serum potassium levels by 0.5–1 mmol/litre in 30 minutes. This CPG also advises the use of 8.4% sodium bicarbonate, stating that it will reduce extracellular potassium by the same degree as salbutamol. Dépret et al (2019) recommend the use of hypertonic sodium bicarbonate: 100 ml–250 ml of 8.4% solution over 20 minutes for patients with a metabolic acidosis (pH<7.2). However, in the prehospital setting, there is no way of telling what the blood pH is.
Prehospital treatment priorities
Treatment priorities include:
Advice card for patients who have fallen
Some patients may not clinically present with the signs and symptoms of rhabdomyolysis and feel well after assistance from the ambulance service. They may not wish to travel with you to the emergency department for further assessment.
In these cases, consider whether they have been given enough information to make an informed decision regarding their care. Paramedics could give a ‘falls advice card’ (Figure 2) to patients who are remaining at home, which can help guide their decision regarding further care.
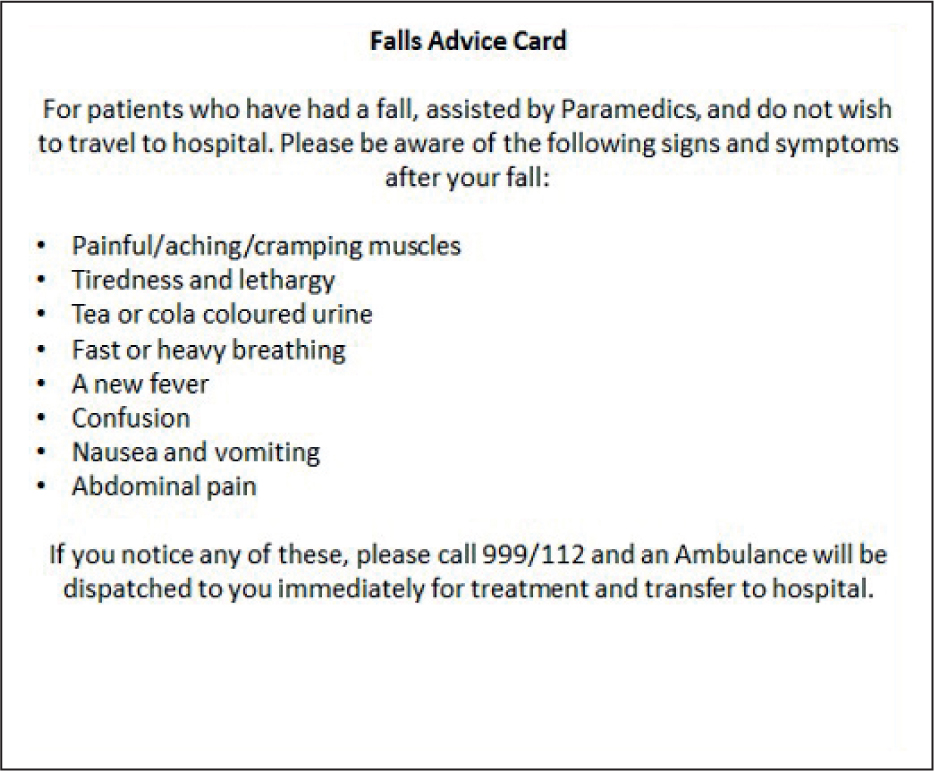
This card would advise the patient to call their GP or the ambulance if the following symptoms occur: painful, aching or cramping muscles, tiredness and lethargy, tea- or cola-coloured urine, fast or heavy breathing, a new fever, confusion, nausea and vomiting, and abdominal pain.
Conclusion
This article outlines what rhabdomyolysis is and how dangerous it can be if not treated promptly, particularly in elderly people who have fallen.
There seems to be no international consensus on how to best treat this condition both in and out of hospital, which poses a challenge to practitioners.
The purpose of this CPD module is to create an awareness of the condition and initiate discussion around it and how best to treat it in the prehospital setting. Treatment options include providing IV fluid therapy, cardiac monitoring and administering nebulised salbutamol if hyperkalemia is suspected. This article does not supersede the clinical practice guidelines you operate under.
Senior clinician support is recommended when considering treatment options outside your normal scope of practice.
Illnesses and traumatic injuries discovered in primary and secondary surveys should be treated accordingly. The suspicion of rhabdomyolysis should be emphasised in your handover to the receiving hospital along with relevant medical and social factors.
If an asymptomatic patient wishes to remain at home, they must be given sufficient advice so they can make a fully informed decision regarding their care. The is potential to provide a falls advice card to help them make a decision if they become unwell after paramedics have attended.

