In the UK, it is estimated that around 103 000 people suffer an acute myocardial infarction each year (Townsend et al, 2012). Paramedics will attend to a number of these patients, delivering specific life saving care and transporting to an appropriate healthcare facility. The use of the 12 lead electrocardiograms (ECGs) by paramedics to diagnose an ST elevation myocardial infarction (MI) is standard procedure, as is the subsequent management of these patients.
Infarctions affecting the right ventricle can occur in isolation however they are more commonly found in association with IMI. Consequently, right ventricular involvement should be considered in all patients presenting with an inferior myocardial infarction (IMI). Patients suffering a right ventricular infarction (RVI) may require alternative treatment methods due to the high risk of haemodynamic instability and cardiac arrhythmia associated with this condition (Yager, 1996; Goldstein, 2002; Pfisterer, 2003).
RVI was first identified over 70 years ago, however, it was not acknowledged as a clinical condition until 1974 when Cohn et al (1974) published results of their study identifying haemodynamic compromise due to right ventricular failure in patients suffering IMI. It is believed that approximately 50 % of IMIs may be complicated by right ventricular involvement (Jacobs et al, 2003; Chockalingam et al, 2005; Kakouros and Cokkinos, 2010). The severity of symptoms experienced by patients varies from mild contraction abnormalities to complete failure of pump function (Goldstein, 2002). Patients with IMI and RVI are likely to have increased in-hospital mortality of 31 % compared with 6 % for those suffering an isolated IMI, and a higher risk of complications (64 % compared with 28 %) (Zehender et al, 1993; Carter and Ellis, 2005). The SHOCK Registry (SHould we emergently revascularise Occluded coronary arteries for Cardiogenic shock (SHOCK) (Jacobs et al, 2003) study found a significant difference in patient survival, with a poorer outcome for people suffering from right ventricular cardiogenic shock in comparison to left ventricular shock (Jacobs et al, 2003). Prompt diagnosis of RVI and early intervention with appropriate treatment methods is essential in reducing mortality (Hashmat et al. 2010).
Right ventricle function
The right ventricle works as a low-pressure volume pump, receiving blood from the systemic venous circulation and pumping it to the pulmonary arteries. Although it has the same stroke volume as the left ventricle, it requires only a quarter of the energy to pump due to low pulmonary vascular resistance, this being 10 % of the systemic resistance (Carter and Ellis 2005; Haddad et al. 2008).
Occlusion of the right coronary artery proximal to the posterior descending coronary artery, compromises blood flow to the right ventricle and explains the involvement of the right ventricle in the majority of IMIs (Fijewski et al. 2002; Spiers, 2006). Ischaemia from the occlusion adversely affects contraction of the right ventricle, which becomes non-compliant and dilated, reducing onward blood flow to the pulmonary artery (Bledsoe et al. 2008). With reduced blood volume from the pulmonary circulation, the left ventricle receives a smaller volume of blood, resulting in diminished left ventricular preload and decreased cardiac output (Yager, 1996; Goldstein, 2002; Kakouros and Cokkinos, 2010). Hypotension frequently ensues; resulting in a reflex tachycardia, which shortens the diastolic period and further compromises haemodynamic stability, ultimately ending in cardiogenic shock (Carter and Ellis, 2005).
‘…a decrease greater than 10 mmHg may be considered an abnormal finding, and is common in patients with pericardial constriction…’
Recognition—physical signs
In the pre-hospital environment, paramedics have only their physical assessment skills and ECG monitoring to assist them in identifying whether RVI is present. Awareness of the different clinical presentations that may occur with RVI is useful and potentially life saving.
In 1930, Saunders identified the clinical manifestations of RVMI, describing a triad of symptoms consisting of, hypotension, clear lung fields and elevated jugular veins (Haddad et al. 2008). Pulsus paradoxus and Kussmauls sign have also been identified in patients suffering RVI (Haji and Movahed, 2000). Pulsus paradoxus is a change in systolic blood pressure seen during inspiration, a decrease greater than 10 mmHg may be considered an abnormal finding, and is common in patients with pericardial constriction (Gray et al, 2008). It may be detected through palpation of the pulse, which can feel weaker or may disappear during inspiration (Haji and Movahed, 2000; Smith, 2008). Kussmaul's sign, also known as external jugular venous distension can be seen in patients with RVI as a result of elevated jugular venous pressure which is caused by a rise in atrial pressure secondary to right ventricular failure (Gray et al, 2008; Smith, 2008). The presence of Kussmaul's sign and elevated jugular venous pressure has been found to have 88 % sensitivity and 100 % specificity for the presence of RVI (Haji and Mohaved, 2000). Peripheral oedema may also be present as pressure in the venous circulation increases and serum is forced from the veins into surrounding tissue (Smith, 2008).
In IMI nausea and vomiting are more common due to increased vagal activity, and stimulation of the diaphragm may also cause hiccoughs or belching (Gray et al, 2008). In addition, patients may also complain of dyspnoea, a result of increased oxygen demand associated with cardiogenic shock, however, auscultation of the chest will reveal clear bilateral air entry (Bledsoe et al. 2008). Lung fields may remain clear as a result of reduced left ventricle preload (Goldstein, 2002).
ECG presentation and interpretation
The conventional 12 lead ECG provides a limited view of the heart, showing predominantly the left ventricle and left anterior descending artery (LAD) coronary artery. In an inferior myocardial infarction, ST segment elevation may be present in leads II, III and aVF (Houghton and Gray, 2003). Lead V1 provides a limited view of the right ventricle, and while IMI with ST segment elevation in V1 is suggestive of RVI, it is not a reliable sign and absence of elevation does not rule out the presence of RVI (Spiers, 2006). Slurring of the ‘R’ wave in the right precordial leads or aVR could also indicate RVI in IMI (Kakouros and Cokkinos, 2010).
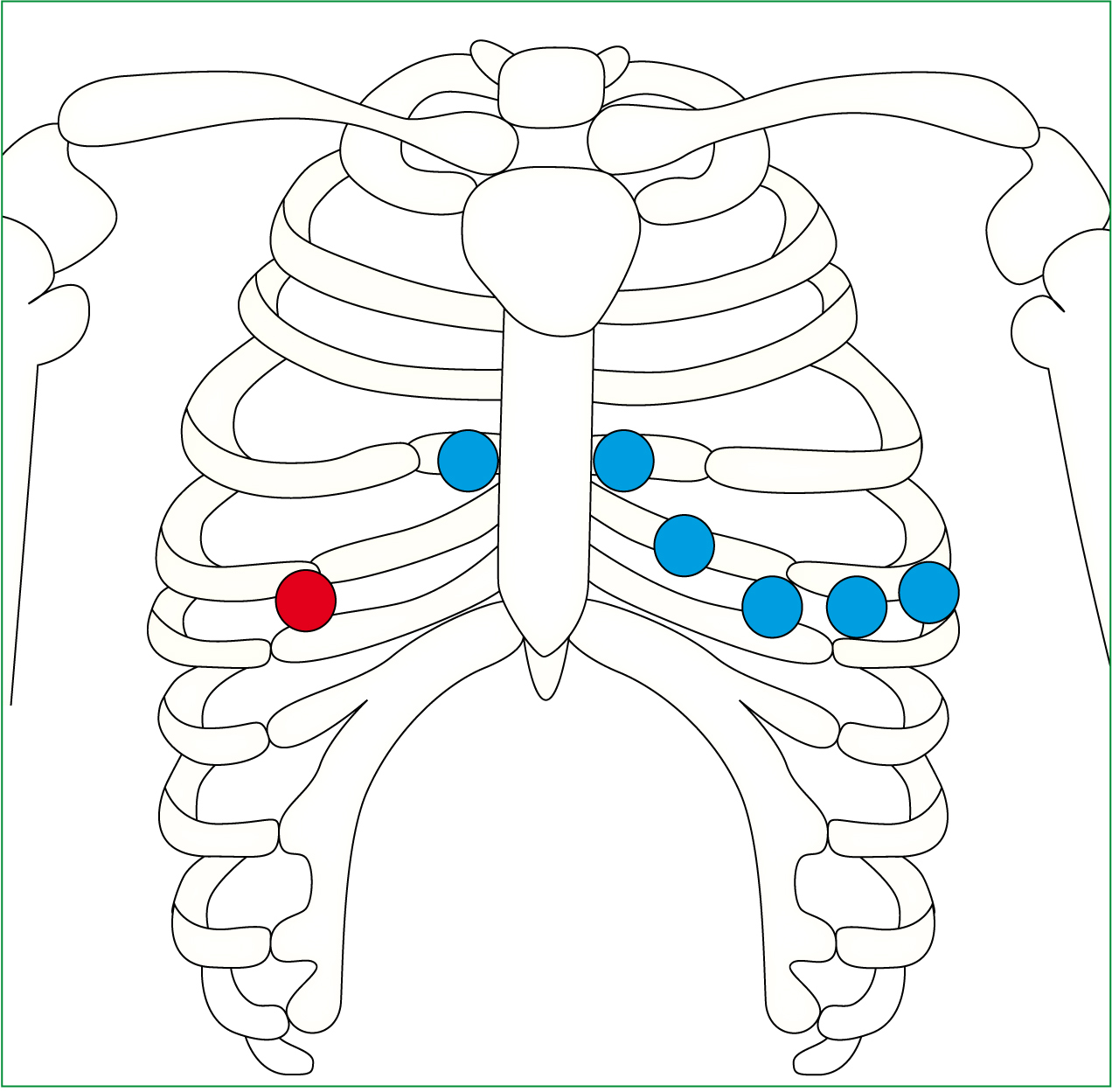
The electrophysiology of the right ventricle can best be examined by moving the left precordial leads in a mirror image onto the right side of the chest, providing a view of the right ventricle, the leads should be labeled V4R, V5R and V6R on the ECG printout to avoid confusion (Spiers, 2006). Some authors argue that a right side precordial ECG should be routine in all patients with IMI to ensure early identification of RVI enabling commencement of appropriate intervention as early diagnosis is crucial to reducing morbidity and mortality (Mehta et al, 2001; Fijewski et al. 2002; Docherty, 2003; Hashmat et al. 2010). However, the above practice can be time–consuming and it can make things difficult when repeating an ECG to identify the possibility of an evolving MI, a quicker alternative is to use the lead V4R to obtain the required view.
It is widely regarded within the literature (Klein, et al, 1983; Zehender et al, 1993; Spiers, 2006) that the moving of lead V4 to the right side of the chest, fifth intercostal space, mid-clavicular line to create lead V4R (Figure 1) is a reliable way to determine RVI, if ST segment elevation > 1 mm is present in this lead then suspect RVI (Houghton and Gray, 2003). Performing a V4R is not indicated in every patient presenting with chest pain, however as 50 % of IMI are associated with RVI it is reasonable to suggest that all patients presenting with an IMI should have a V4R. This should take place early in the assessment of these patients as changes may be transient and disappear by the time of arrival at hospital, also identification of a RVI requires alternative management compared to standard acute coronary syndromes (ACS) (Docherty, 2003; Spiers, 2006; Kakouros and Cokkinos, 2010).
Klein et al (1983) measured the sensitivity of ST elevation in V4R to determine its reliability in diagnosing right ventricular involvement. They found ST segment elevation in V4R in 82.7 % of patients with an IMI also had RVI, and concluded that early recording of V4R in patients with IMI is a simple and effective diagnostic test in determining whether there is a RVI.
Although ST segment elevation > 1mm in V4R is an indicator of RVI, it is often a transient finding. Studies have found it to be absent in patients with RVI presenting 12 hours after onset of chest pain (Haji and Movahed, 2000). Chockalingam et al (2005) advise that a right-sided ECG should be routine in all patients presenting with an acute IMI as ST-segment recovery occurred with 85 % of patients in 24 hours and nearly all patients by 48 hours. Klein et al (1983) suggest an even smaller time frame of two hours before ST elevation disappears, emphasising the importance of an early ECG following onset of chest pain. Unfortunately, times given by studies vary and no specific time frame can be given, however it would seem reasonable to acquire an ECG incorporating V4R as early as possible Where indicated, RVI can be further complicated by disruption of blood flow to the SA and AV nodes which can lead to a multitude of arrhythmias, including sinus bradycardia, AV nodal blocks, ventricular tachycardia and where atrial infarction has occurred, atrial fibrillation (Goldstein, 2002; Spiers, 2006; Haddad et al. 2008). Right bundle branch block and third degree heart block may also be associated with RVI (Carter and Ellis, 2005).
Implications for the pre-hospital environment
In patients suffering IMI with RVI, consideration should be given to the complications that may occur and the therapeutic options available to paramedics to mitigate these. Paramedics should ensure a thorough physical assessment of their patient is completed, taking into consideration time critical features. Hypotension should not be completely relied upon as fewer than 50 % of patients initially present with haemodynamic compromise (Rotondo et al, 2004; Carter and Ellis 2005). Chockalingam et al (2005) found only 20 % of patients presented with Kussmaul's sign and 36 % had clear lung fields despite complaining of dyspnoea. Therefore, it could be argued that the single most useful tool in investigating a patient with a possible RVI pre-hospitally is the ECG.
In IMI with suspected RVI the use of nitrates and opiates is well discussed within the literature, Goldstein (2002) states that vasodilators and diuretics are contraindicated in treatment of RVI. Other authors advise they be used with caution as a reduction in cardiac output could lead to hypotension (Houghton and Gray, 2003; Jacobs et al, 2003; Carter and Ellis 2005; Spiers, 2006; Bledsoe et al. 2008). Patients with IMI and RVI may not initially present with hypotension but may develop this with a reduction in preload initiated by bradyarrhythmia or administration of nitroglycerine (Goldstein, 2002). GTN and morphine both have a vasodilatory affect, and should not be administered to any patient with a systolic blood pressure of less than 90 mm Hg. For those patients presenting with IMI and RVI who have a stable blood pressure, administration of nitrates, or, to a lesser extent opiates, may compromise this.
When a paramedic is present it could be argued that fluids can be administered in an attempt to rectify hypotension however, it is has been suggested that fluid administration alone will not be adequate to counteract the severe hypotension patients may experience in response to nitrates or other vasodilatory drugs, raising the issue that paramedic intervention may not be sufficient to resolve the problem.
The Resuscitation Council (RC) advise against the use of nitrates and other vasodilatory drugs in patients with IMI and suspected RVI (Arntz et al, 2010). Current Joint Royal Colleges Ambulance Liaison Committee (JRCALC) clinical practice ambulance guidelines recognise a systolic blood pressure of less than 90 mmHg as a contraindication for the administration of GTN or Morphine (JRCALC, 2006). However there is no recommendation in place for those patients suffering an IMI to have an ECG including V4R performed prior to administration of GTN to exclude the possibility of RVI. If RVI is suspected, obtaining IV access and preparing an infusion of 0.9 % sodium chloride prior to giving these will ensure the paramedic is prepared to administer a fluid bolus should the drugs provoke a negative haemodynamic response (Arntz et al, 2010). It could be argued that fluid administration to an infarcted heart is controversial, however, fluids are required to ensure blood supply to the left ventricle by maintaining right ventricular output (Houghton and Gray, 2003; Kim et al, 2006). The concept of volume loading is based upon Starling's law, the strength of ventricular contraction is increased by stretch, the greater the stretch, the stronger the contraction (Marieb, 2009).
‘The implementation of specific treatment options for RVI into JRCALC guidelines will ensure all paramedics are aware of this condition and apply it to clinical practice.’
Several studies emphasise caution when administering fluid, and, as there is the possibility of volume overload, fluid administration must be monitored carefully as excessive amounts may further compromise right ventricular function by causing an increase in ventricle wall tension and a decrease in contractility, reducing cardiac output (Yager, 1996; Jacobs et al 2003; Kakouros and Cokkinos, 2010). The paramedic should aim to maintain a systolic of 90 mmHg (Spiers, 2006).
Conclusions
Through exploration of literature, this article has studied RVI within the pre-hospital environment, including the pathophysiology, recognition, diagnosis, associated complications and management of this condition. Pre-hospitally, awareness of this condition can ensure early diagnosis and implementation of therapeutic intervention where required, reducing patient morbidity and mortality. The V4R lead has been found to have high sensitivity and specificity in diagnosing the presence of RVI in IMI (Docherty, 2003). Performing this diagnostic test pre-hospitally can capture a change that may not be present on arrival at hospital, as literature suggests this is transient and known to disappear within an unspecified time frame. For those patients suffering an IMI, this will prompt the provider to perform a V4R to confirm or deny the presence of RVI. Performing and recording a 12 lead ECG including V4R prior to administration of nitrates or other vasodilating drugs such as opiates will ensure the risk of haemodynamic instability is avoided or precautions taken to correct it, should it occur. The implementation of specific treatment options for RVI into JRCALC guidelines will ensure all paramedics are aware of this condition and can apply it to clinical practice. Consideration should also be taken in highlighting the risks associated with administration of vasodilatory drugs.
Further research into RVI within the pre-hospital environment would be advantageous as current literature is limited, with the majority involving research within a hospital environment performed by physicians.
