United Kingdom statistics for asthma show 1 204 deaths from asthma in 2008 (Asthma UK, 2008). Although death rates from asthma are declining, near-fatal asthma (NFA) still presents a signifcant challenge to emergency responders, with most asthma deaths occurring outside of the hospital (Rodrigo et al, 2004). Restrepo and Peters (2008) define near fatal asthma as ‘typically associated with the presence of hypercapnoea, acidaemia, altered state of consciousness and the development of cardio-respiratory arrest requiring endotracheal intubation and mechanical ventilation’.
NFA is a subtype of asthma with unique risk factors and variable presentation that requires early recognition and aggressive intervention. (Restrepo, 2008). United Kingdom ambulance dispatch records show that around 17 % of ambulance calls are prioritised as breathing diffculties (Clawson, 2008). Of these, around 30 % are identified as being asthmatic. While all of these calls cannot be attributed to NFA, it is reasonable to surmise that paramedics are called to patients with life-threatening asthma and some of these may later be categorised as near-fatal.
Case description
A 999 emergency call to a 57-year-old female with breathing diffculty; seen to collapse in the street and ‘going blue’. The caller, a passer-by, said the female was holding an asthma inhaler. The ambulance, with a crew comprised of two paramedics and a nurse observer, arrived on the scene within 4 minutes of the initial call, no bystander cardiopulmonary resuscitation (CPR) was being carried out on their arrival.
On assessment, the female was unresponsive, apnoeic and pulseless. CPR was commenced while the defibrillator pads were attached. The monitor showed a, non-shockable, bradycardic pulseless electrical activity (PEA). It was immediately apparent that the patient had severe bronchospasm; as ventilation utilising a bag/ valve/mask, oxygen, and an oral pharyngeal airway was extremely difficult. The pressure required to squeeze the bag was excessive, airways resistance was very high and the expiratory phase was protracted.
Closer examination revealed central cyanosis and oxygen saturations of 79 %. A decision was made to perform early endotracheal intubation to permit higher ventilation pressures. Intubation was achieved rapidly, utilising laryngoscopy, cricoid pressure and the tube being passed under direct vision. Once the airway was secured, the patient was evacuated from the roadside into the ambulance.
CPR continued and it was noted that the chest compression was helping with the expiratory phase of ventilation, but there was still no improvement in the active phase; with excessive effort required to squeeze the bag. As intravenous access had not been attempted by this point, a decision was made to administer adrenaline via the endotracheal route and 2 mgs of 1:10 000 was accordingly instilled.The effect was almost instantaneous; a marked reduction in resistance was felt as the adrenaline was ‘bagged in’. As ventilation continued, the operator became aware that, with each inflation, the bronchospasm was palpably dissipating; oxygen saturations picked up to 94 % and within minutes of the improved ventilation, return of spontaneous circulation (ROSC) was achieved.
The patient was admitted via the emergency department to the intensive care unit where she was sedated, ventilated, and subsequently went on to make a full recovery without any neurological deficit. The patient had been an asthmatic since childhood, and the ‘brittle’ asthma was variably controlled and she had a history of previous emergency department attendances, although no history of needing to be ventalated. On the day of the emergency call, she had awoken in the night with a tight chest and a wheeze, and following contact with the out-of-hours services, was advised to attend the local medical centre in the morning. She had been walking to the centre at the time of collapse.
Literature search
A literature search strategy using medline, Cinahl Plus and the Cochrane Library for the time period 01-01-1980 to 01-03-2012, using the search terms ‘[Endotracheal OR Intratracheal] AND [Epinephrine OR Adrenaline] AND [Asthma OR Asthma AND Attack]’ yielded 23 clinical papers, of which only two studies were clinically relevant to the subject area.
Liebman (1997) wrote a case study report of an in-hospital, 13-year-old asthmatic patient in cardiac arrest, secondary to acute asthma, which responded well to high dose (8 mgs) endotracheal epinephrine, though Liebman acknowledged that the improvement may have been also due to other treatment factors.
A recently completed ‘best evidence topic’ meta-analysis (Nutbeam, 2009) showed there to be insuffcient evidence to support the routine use of endotracheal adrenaline in patients with respiratory arrest secondary to asthma, citing the aforementioned Liebman (1997) case study as the only clinically relevant paper. However, as a result, they did support consideration of the use of endotracheal adrenaline in patients unresponsive to conventional treatment.
Discussion
The pathogenesis of acute asthma is described in Table 1 (Smith et al, 2000; Woodruff et al, 1998; Barr et al, 2000; Rodrigo et al, 2000). Type 1, or slow-onset acute asthma, is more common (80 %–90 %) and is characterised by airway infammation, excess mucous production and a gradual onset over many hours, days or sometimes weeks. Upper respiratory tract infections have been identifed as the predominant trigger for this type and they are generally slow to respond to treatment.
| Type 1 | Type 2 | |
|---|---|---|
| Descriptiopn and onset | Slow-onset acute asthma | Sudden-onset, asphyxic, brittle, hyperacute asthma |
| Rate of occurance | 80–90 % | 10–20 % |
| Deterioration | Progressive deterioation: >6 hours (usually days or weeks) | Rapid deterioation: ¼ 6 hours |
| Trigger factors | More likely to be triggered by URTI | More likely to be triggered by respiratory allergens, exercise, and phychological stress |
| Pre-deminant mechanism | Inflammation | Bnonchospasm |
| Airways obstruction | Less severe at presentation | More severe obstruction at presentation |
| Response to tretment | Slow | Rapid |
Table adapted from Rodrigo et al, 2004
Type 2, asphyxic or hyperacute asthma, is the less common type (10 %–20 %), and is characterised by severe bronchospasm and an acute onset over 3–6 hours. Trigger factors for this type include allergen exposure, emotional distress and exercise. Response to treatment is more rapid in this group. (Rodrigo et al, 2004; Wasserfallen et al, 1990).
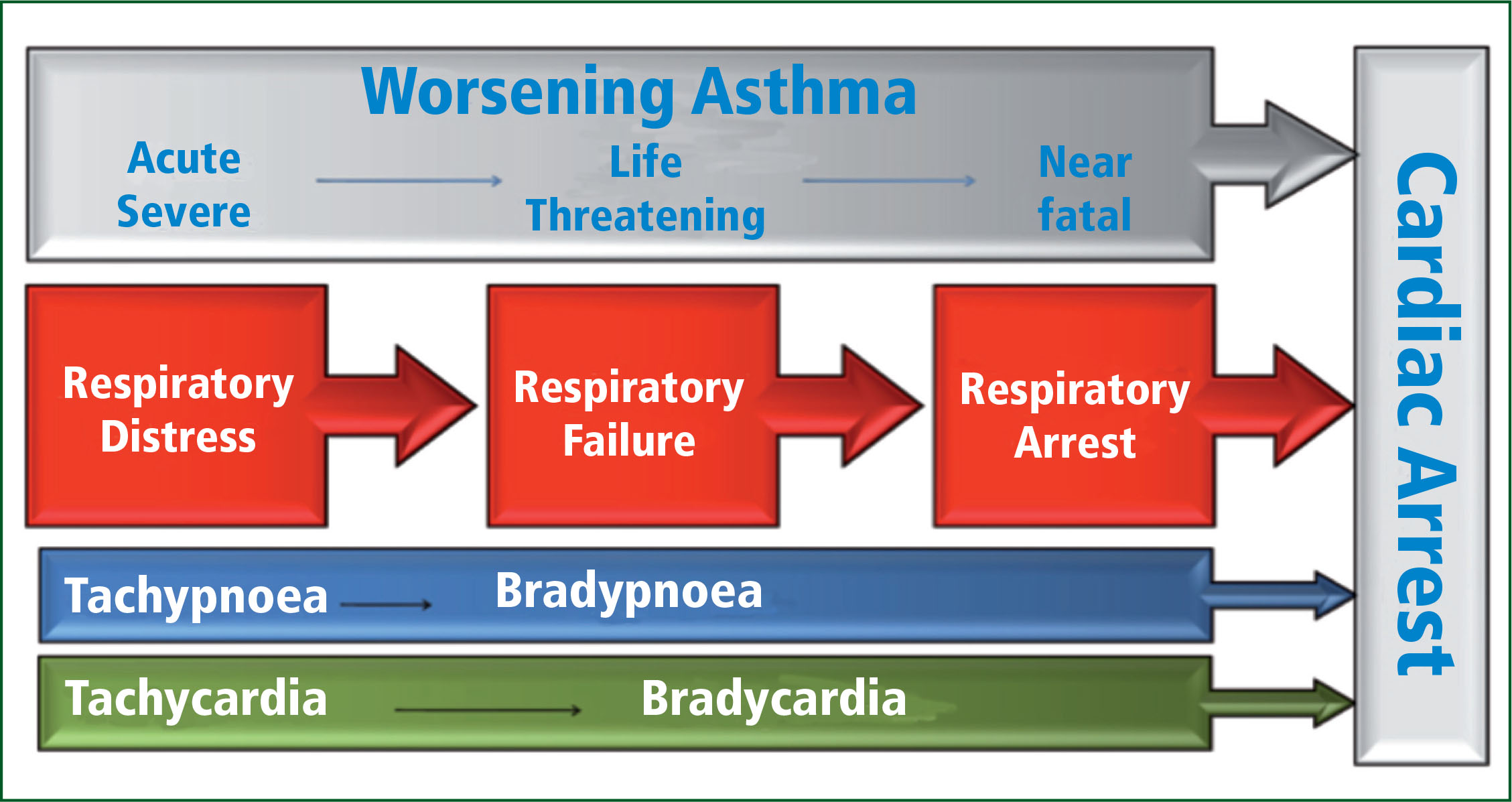
It may be surmised from the descriptors and the patient history, that the second of these, asphyxic asthma, is the more likely phenotype for our case report's NFA pathogenesis, the probable mechanism being respiratory failure developing into respiratory arrest; alongside a bradycardia developing into cardiac arrest (Figure 1).
The pharmacodynamics of endotracheal adrenaline administration and intrapulmonary drug absorption were first described in 1967 when a study compared the effects of intravenous, intra-cardiac and endotracheal adrenaline in an induced hypoxic cardiac arrest using a dog-model. The study concluded that each route was equally effective in reversing circulatory collapse (Redding, 1967). Until 2010, successive international resuscitation guidelines have recommended that the endotracheal route be the second choice for cardioactive drugs in the management of cardiac arrest. The route takes advantage of the extensive, absorptive pulmonary surface area of the lung, more than 65 m2 (Greenberg, 1984). Drug absorption occurs at all levels of the respiratory tract from the trachea to the alveoli. Greenberg and Spivey (1985) demonstrated that radio-opaque contrast media, administered endotracheally, was dispersed bilaterally to both lungs, but distally to the alveoli only after forceful, manual hyperventilation. The study recommended 5–10 rapid ventilations following instillation.
It needs to be highlighted that the 2010 International Consensus Guidelines for Advanced Life Support (Deakin, 2010) has withdrawn the recommendation to use the endotracheal route for cardiac arrest drugs, citing unpredictable plasma concentrations following administration, and the increased evidence in favour of the intraosseous route as a secondary choice to intravenous access. This case episode happened prior to the guideline changes.
British Thoracic Society guidelines state that there is limited evidence to support the use of parenteral β2 agonist therapy, but suggests that intravenous therapy should be reserved for those patients in extremis in whom inhaled therapy cannot be used reliably (BTS/SIGN, 2009). The guidelines do not discuss the endotracheal route. Putland et al (2006) have shown that intravenous epinephrine is associated with a low rate of major, and a moderate rate of minor adverse events in patients with severe asthma.
United Kingdom pre-hospital clinical practice guidelines (JRCALC, 2006) advise that 500 mcgs of adrenaline 1:1000 can be administered subcutaneously or intramuscularly ‘in life threatening asthma with failing ventilation and continued deterioration despite nebulised therapy’.
Although there are no studies which examine or compare the use of endotracheal adrenaline in acute asthma, some equivalency may be considered when looking at studies of nebulised adrenaline. Nebulised drug therapy, in its pharmacokinetics, also uses the extensive pulmonary vascular bed. A meta-analysis of randomised control trials showed that 2 mgs of nebulised adrenaline was as effective as 5 mgs of nebulised salbutamol in treating moderate-severe acute asthma (Rodrigo and Nannini, 2006).
It was noted that during the arrest management, some improvement in the expiratory phase was noted with external cardiac compressions. Dynamic hyperinfation has also been identified with the pathophysiology of respiratory arrest in NFA. Dynamic hyperinflation is over-inflation of the lungs and in its mechanism bronchospasm and airways obstruction from mucous plugging prevents or prolongs the expiratory phase of ventilation. It has been hypothesised in many case reports that external chest compression may be a treatment strategy in patients with air trapping due to acute asthma (Rosenfeld et al, 2006; Fisher et al, 2001; Williams et al, 2007; Harrison, 2010). While in our case report the external chest compression was not a treatment choice to overcome air trapping, (rather, it was intended as a response to cardiac arrest), it was noted that when the chest compressions coincided with the expiratory phase of ventilation, there was an improvement in expiration and an audible ‘whoosh’ as air was expelled. Although it didn't appear to improve the ease of the inspiratory phase of ventilation, it is reasonable to surmise that the ECM was a factor in the successful resuscitation of the case study subject.
Summary
The instillation of endotracheal adrenaline in out-of-hospital respiratory/cardiac arrest due to asthma is a procedure that can be considered if conventional methods of ventilation are failing. The results described here were too immediate for the operator to doubt that the improved active phase of ventilation was due to its administration. The severe bronchospasm encountered when trying to ventilate patients with asphyxic asthmatic arrest is well known. As is the β2 agonist effect of adrenaline on reversing bronchospasm. The direct application of adrenaline to the absorptive pulmonary surface of the airways, allows for a more direct route for the drug to act on the smooth muscle. It may be that this is particularly important when comparing it with the potential haemostatic delay when administering the drug via the intravenous/ intramuscular route. The resultant improvement in ventilation has resulted in reversal of hypoxia and restoration of spontaneous circulation. The role of chest compression and its effect on the passive phase of ventilation is also acknowledged in this case.
