An emergency call was placed to emergency medical services (EMS) requesting an ambulance for a patient whose implantable cardioverter-defibrillator (ICD) had fired. An advanced life support (ALS) unit arrived to find a 70-year-old male in no acute distress. The initial electrocardiogram (ECG) showed ventricular tachycardia (VT). The patient was then shocked by his ICD, which converted him back into a paced rhythm. The patient again went into VT and was shocked an additional four times by his ICD prior to the arrival of the transporting ambulance.
The ambulance crew found the patient awake and alert, and complaining only of chest pain from the ICD fring. Vital signs were as follows: heart rate 70 beats per minute and regular, blood pressure 118/80 mmHg, respiratory rate 16 breaths per minute, and pulse oximetry 99% on room air. The patient's 12-lead ECG showed a paced rhythm. The patient had a past medical history of coronary artery disease, hypertension, high cholesterol, and congestive heart failure. His surgical history included coronary artery bypass grafting and multiple cardiac stents. His medication list included clopidogrel, furosemide, amiodarone, simvastatin, and carvediol. The patient was transported to the emergency department without need for further intervention.
Discussion
Background of implantable cardioverter-defibrillators
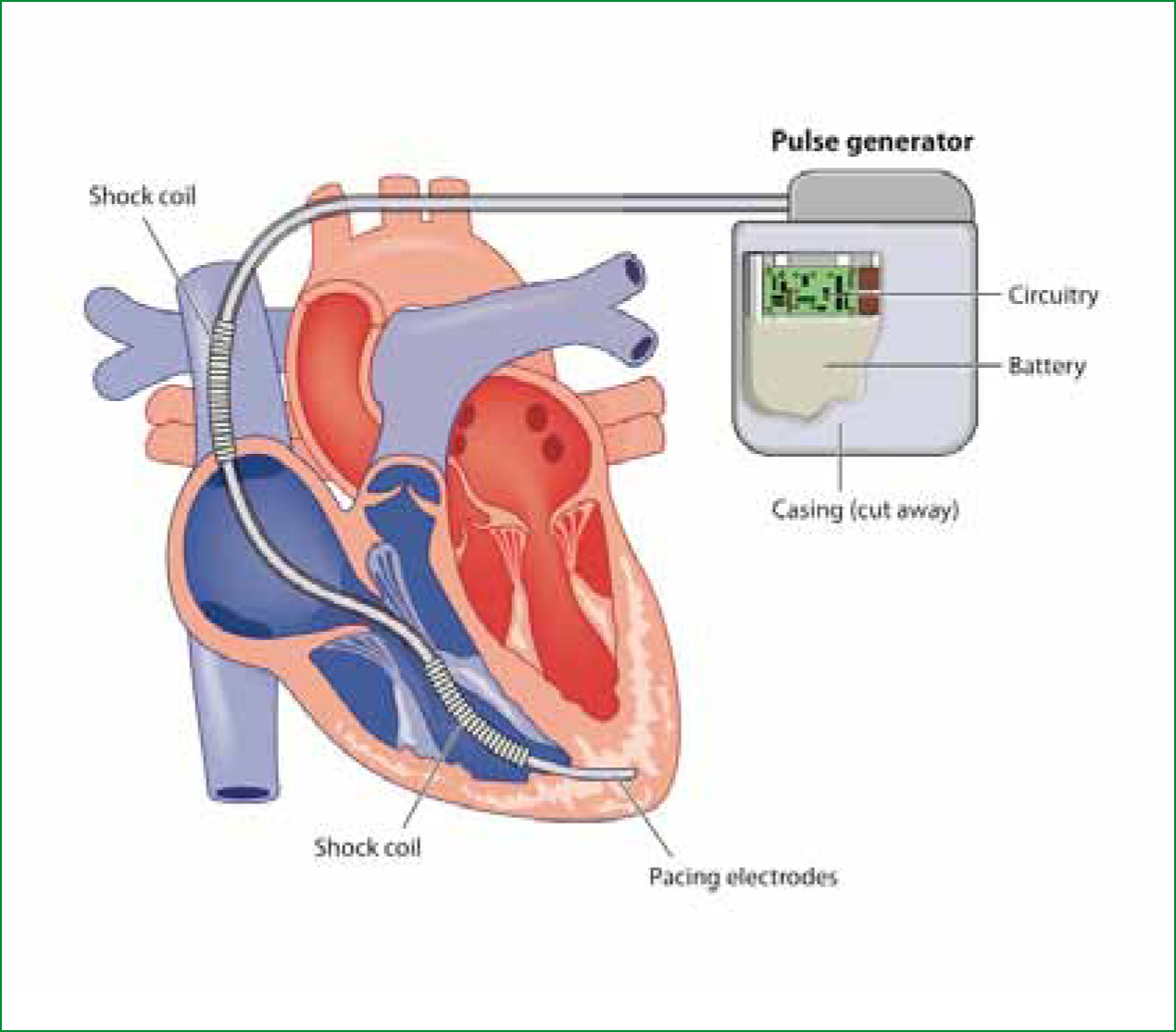
The first implantable cardioverter-defibrillator (Figure 1) was placed in 1980 (Mirowski et al, 1980). Since that time, the number of patients with ICDs has grown exponentially. There are several indications for implantation of an ICD (Goldberger and Lampert, 2006). The major indication is the survival of cardiac arrest caused by ventricular fibrillation (VF) or ventricular tachycardia (VT). Other indications for ICDs are for patients with cardiomyopathies and ejection fractions less than 35%. ICDs are also placed in patients at high risk for VF arrests, such as those with congenital long QT syndrome or Brugada syndrome.

The most common method to insert an ICD is to implant the pulse generator in the chest wall through a small incision, and foat the lead through the left subclavian vein, superior vena cava, into the heart (Gehi et al, 2006). The large lead, which acts as a sensor, pacemaker, and defibrillator, is placed into the apex of the right ventricle. The lead can also be implanted on the epicardial surface of the heart (Figure 2).
ICDs work by sensing changes in the cardiac rhythm through preprogrammed algorithms. When ventricular tachycardia is sensed by the ICD, it uses one of three modalities to correct the rhythm. During episodes of slow ventricular tachycardia, the ICD can use anti-tachycardia pacing, also known as overdrive pacing (Sweeney, 2004). In the anti-tachycardia pacing mode, the ventricles are paced at a faster rate than the ventricular tachycardia, blocking the arrhythmia from propagating. This modality successfully terminates VT 90–95% of the time. Anti-tachycardia pacing is painless and cannot be felt by the patient.
If anti-tachycardia pacing does not work or the patient is in a rapid ventricular tachycardia, the ICD will attempt to cardiovert the patient at approximately 5–10 joules. This shock may be felt by the patient. If the cardioversion is unsuccessful or the cardiac rhythm degenerates into ventricular fibrillation (VF), the ICD will defibrillate the patient at approximately 35 joules.
The batteries in ICDs last between 4–9 years and have the capability of delivering up to 100 shocks (DiMarco, 2003). The cost of an ICD ranges between $10 000 to $40 000 (USD) and the cost of implantation ranges between $6000– $12000 (USD).
An ICD is interrogated by placing a sensor over the ICD. The evaluation can be done by a cardiologist or by a specially trained technician from the ICD manufacturer. Interrogation of the ICD can determine how many times anti-tachycardia pacing has been used, how many times the device has cardioverted or defibrillated a patient, and the patient's cardiac rhythm at the time of electrical intervention. There is no danger to a healthcare provider if he or she is touching a patient who is shocked by an ICD. The electrical impulse is a very small amount of electricity and is directed into the apex of the heart. If a pre-hospital provider needs to defibrillate or cardiovert a patient with an ICD, the defibrillator paddles or pads should not be placed on top of the device. However, it is perfectly safe to deliver a shock using an anterior–posterior or sternum– apex positioning of the pads or paddles.
There are four common scenarios that pre-hospital providers many encounter when dealing with a patient whose ICD fired: a single shock, phantom shock, inappropriate shocks, and multiple shocks.
Scenario 1: a patient receives a single shock from an ICD
In this scenario, the patient has usually been restored to a stable rhythm by the time pre-hospital providers arrive. Treatment consists of supportive care including oxygen, cardiac monitoring, and a 12– lead ECG. Many ALS protocols call for establishment of IV access in case a patient's condition deteriorates, although there is little data to support this practice. If a patient is complaining of chest pain, palpations, syncope, or shortness of breath, appropriate treatment protocols should be followed. If the chest pain appears to be a result of the ICD shock, administration of an opiate is appropriate.
Although most EMS systems will opt to transport all patients who receive a shock from an ICD, patients who are asymptomatic after a single shock do not necessarily need an emergency department evaluation. The current recommendation for an asymptomatic patient who receives a single ICD single shock is to follow up with his/her cardiologist within one week for an interrogation of the ICD (DiMarco, 2003). Patients with ICDs often have serious co-morbidities and are at high risk for adverse events. We therefore recommend that pre-hospital providers discuss the decision not to transport a patient after an ICD shock with direct medical oversight.
Scenario 2: phantom shock
A phantom shock is the sensation of feeling a shock when the ICD has not actually discharged. The etiology of phantom shocks is unknown. However, the only way to differentiate between a real shock and a phantom shock from is to interrogate the ICD. Therefore, EMS providers should follow the same recommendations as for a patient who is asymptomatic after a single ICD shock.
Scenario 3: inappropriate shocks by an ICD
ICD trials have reported a rate of inappropriate shocks between 13 and 22% (Gehi et al, 2006). Inappropriate shocks usually result from the ICD misinterpreting a supraventricular tachycardia, such as atrial fibrillation with rapid ventricular response, as VT. Inappropriate shocks can also result from the ICD double-counting QRS complexes or over-sensing T waves.
One option for terminating inappropriate shocks from an ICD is to place a magnet over the device to deactivate the defibrillation function (Miller and Hsia, 1996). However, few pre-hospital providers carry a magnet. Therefore, treatment of inappropriate ICD shocks in response to a supraventricular tachycardia is to slow the underlying rhythm. EMS providers should follow their appropriate treatment protocol for atrial tachydysrthymias. By slowing the supraventricular tachycardia, the ICD will not attempt to shock a rhythm it interprets as ventricular tachycardia.
Scenario 4: ICD fres appropriately more than once
When an ICD fres continuously in response to an appropriate rhythm such as VF or VT, it is referred to as an electrical storm. The ICD is functioning appropriately by shocking the patient; however the device is unable to terminate the VT or VF.
Treatment is two-fold. First, medical treatment should be aimed at terminating the underlying dysrhythmia (Miller and Hsia, 1996). Because the patient is being cardioverted or defibrillated appropriately, the ICD should not be deactivated. Antidysrhythmics such as amiodarone or lidocaine can be administered to terminate the VT, though there is little research involving these medications in the pre-hospital environment. Procainamide is an alternative antidysrhythmic, though not often used in the pre-hospital setting (Zipes et al, 2006).
Second, if the patient is conscious, treatment for electrical storm should include analgesia and sedation of the patient. Opiates and benzodiazepines should be administered liberally as repeated fring of the ICD causes pain and anxiety to the patient. Intubation for pain control may be necessary in severe cases.
Although ICDs can be lifesaving by preventing sudden cardiac arrest, they often result in end of life difficulty. ICDs significantly prolong the lives of young patients with congenital cardiac arrhythmias, such as Brugada syndrome, for which there are no other effective treatments. However, a larger number of ICDs are implanted in older people with diseased hearts. As patients reach the end of their lives and their cardiac function worsens, an ICD can be a barrier to a quiet death.
Case continued
The patient remained in a paced rhythm for the first twenty minutes in the emergency department. The patient then went into VT and was shocked by his ICD. This reoccurred four times in the following five minutes. The patient was loaded with amiodarone at a dose of 150 mg over 10 minutes. The first dose of amiodarone did not terminate the VT and the patient was shocked an additional three times. The patient was given large doses of fentanyl and lorazepam but continued to complain of severe pain. An electrophysiologist was consulted immediately who attempted to reprogram the ICD.
The patient received a total of 12 shocks in the emergency department and despite best efforts, continued to recurrent VT. After consultation with the electrophysiologist and discussion with the patient, the patient was intubated by the emergency department staff and sedated for comfort. In the hospital, the patient underwent an unsuccessful electrophysiology study in which cardiologists attempted to ablate abnormal electrical foci in the heart. He then underwent surgical repair of a left ventricular aneurysm as a palliative measure. During the surgery, the patient deteriorated, became hypotensive, and expired.
Conclusion
Pre-hospital personnel can expect to encounter patients after an ICD shock more frequently as this device is implanted into patients with increasing regularity. For a single shock, a patient may or may not need transport to an emergency department. Pre-hospital personnel must be able to assess a patient receiving multiple shocks to determine whether the shocks are appropriate.
If the shocks are not appropriate, the pre-hospital personnel must either treat the underlying dysrhythmia or provide analgesia and sedation until the ICD can be deactivated. If the ICD is appropriately shocking an unstable ventricular rhythm, paramedics must be prepared to provide anti-arrhythmic therapy coupled with analgesia and sedation. Although the approach to patients with an ICD firing follows a straightforward algorithm, managing a patient who is receiving frequent shocks can be distressing to both the patient and the provider.
