Suicide by ingestion is a serious health issue, accounting for 30 000 deaths and approximately US$ 1.6 billion in lost income to the US annually. (Goldsmith et al, 2002). Although a problem throughout all age groups, in 2007, suicide was the third leading cause of death for young people aged 15-24 in the US (Center for Disease Control and Prevention, 2011). In the most recent annual report from the American Association of Poison Control Centers, there were 70 294 toxic exposures to antidepressants alone, accounting for 6.5% of the total deaths associated with toxic ingestion (Bronstein et al, 2010).
Tricyclic antidepressants (TCA) are the most common group of medications encountered in antidepressant poisoning (Phillips et al, 1997; Bosch et al, 2000; McFee et al, 2001; Graudins et al, 2002; Arranto et al, 2003; Unverir et al, 2006). Further confounding the danger of TCA ingestion is the predilection for direct cardiac effects. As with other toxic antidepressant ingestions, tachycardia is the most common electrocardiogram (ECG) finding (Fasoli and Glauser, 1981; Niemann et al, 1986; Mills, 2000; Benowitz, 2004; Liebelt and Francis, 2002; Unverir et al, 2006); however, TCA ingestions account for the vast majority of abnormal ECG findings. TCA ingestions have a higher rate of cardiovascular effects—including, conduction disturbances, dysrhythmias, and hypotension (White et al, 2008).
Cardiovascular effects are not the sole concern for the healthcare provider in TCA ingestion as TCAs can also cause coma, seizures, respiratory depression, and gastrointestinal symptoms (Lewis-Abney, 2000; Michael and Sztajnkrycer, 2004; White et al, 2008) and require a higher rate of intubation than any other agents (Unverir et al, 2006).
Prehospital care providers and clinicians face several challenges when managing patients following TCA ingestions. Often, the exact type of ingestion is unknown. Polypharmacy is a common occurrence in toxic ingestion and further confounds treatment. In this article, we present a case of TCA-induced dysrhythmia that was not recognized in the field, and discuss some issues related to making this difficult diagnosis.
Case report
At 23:05 pm, a 911 call was placed from a private residence requesting an ambulance for a possible overdose. An advanced life support (ALS) unit was dispatched at 23:06 pm as an urgent request and arrived on scene within 6 minutes. Patient contact was reported at 23:13 pm. EMS personnel found a 14-year-old white male lying supine in the hallway of his residence. The father reported that he found the victim in the bedroom awake but ‘not acting right’ and ‘unable to stand up’, approximately 30 minutes before calling 911.
On initial prehospital assessment, there was no evidence of trauma and the patient was responsive only to painful stimuli. Due to the patient's unresponsiveness, a limited history was obtained by the paramedics; however, the patient was noted to suffer from depression and migraine headaches.
Physical assessment revealed a respiratory rate of 32, heart rate of 160, blood pressure of 137/60, and initial prehospital Glasgow coma scale (GCS) was 8 (eye opening: 2, verbal: 2, and motor: 4). Initial blood glucose level was 8 mmol/L.
The crew began to administer oxygen to the patient by non-rebreather mask, and a 26-french nasopharyngeal airway was placed in the right nare, with minimal patient response to the procedure. The scene time was 14 minutes. While en route to the emergency department (ED), a 20-gauge peripheral intravenous (IV) catheter was established in the right antecubital fossa with normal saline at a wide-open rate, and 2 mg of naloxone (Narcan) was administered intravenously as per EMS protocol. During the 26-minute transport, the ALS unit was diverted from the closest ED to the Children's Mercy Hospital ED. During transport, the blood pressure gradually worsened (106/53), and the patient became more unresponsive (GCS not documented).
Hospital course
Contact was made to the Children's Mercy Hospital ED, with an 8-10 minute estimated arrival. Following the initial EMS report, a phone call was received in the ED from EMS dispatch, alerting the staff that one of the empty pill bottles found on the scene included amitriptyline.
On arrival to the ED, the patient was noted by the paediatric emergency physicians to be unresponsive to all stimuli with initial GCS of 3. Vital signs on arrival included a heart rate of 134, a respiratory rate of 8, and a blood pressure of 117/61. The initial eye examination revealed 4 mm and sluggishly responsive pupils. The physical examination demonstrated no evidence of trauma or other abnormalities.
Immediately following arrival, the patient was intubated with a 7-0 cuffed endotracheal tube via GlideScope®, using rapid sequence medications in anticipation of imminent respiratory failure. A nasogastric (NG) tube was placed and 50 g of activated charcoal with sorbitol was infused. A 12-lead ECG was performed, demonstrating a wide-complex tachycardia with prolongation of the QRS and QT complexes (Figure 1).
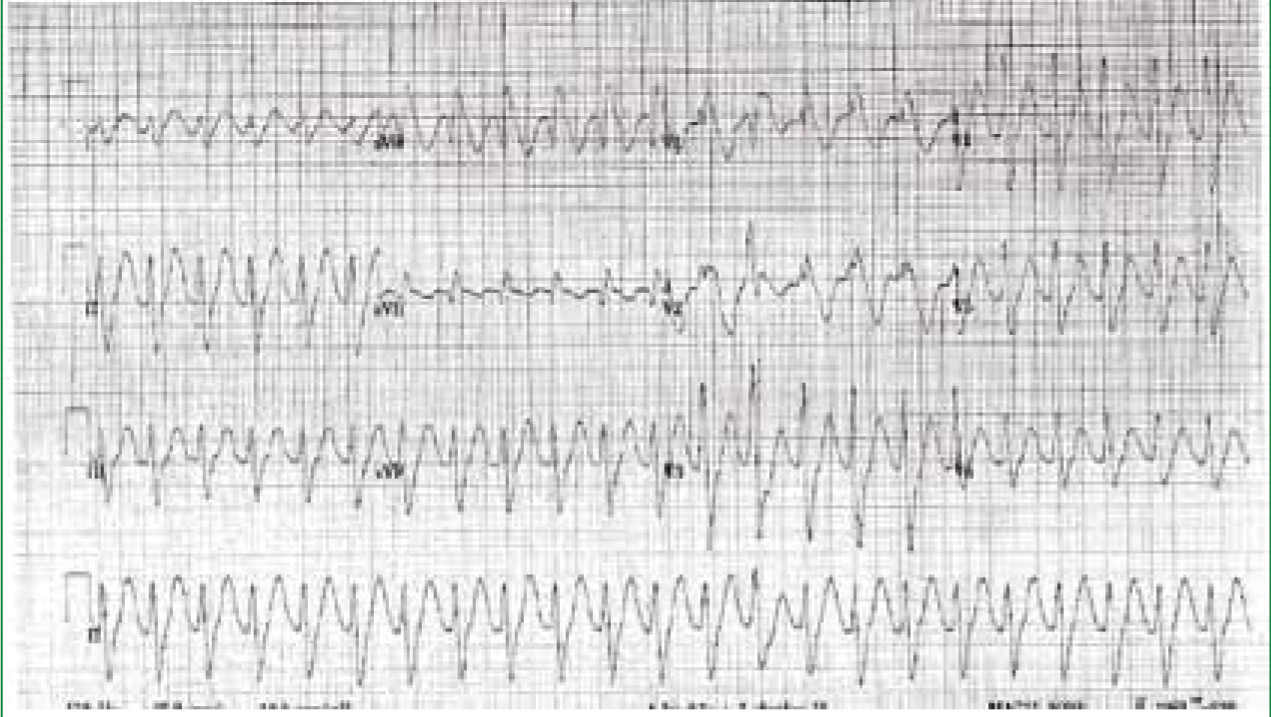
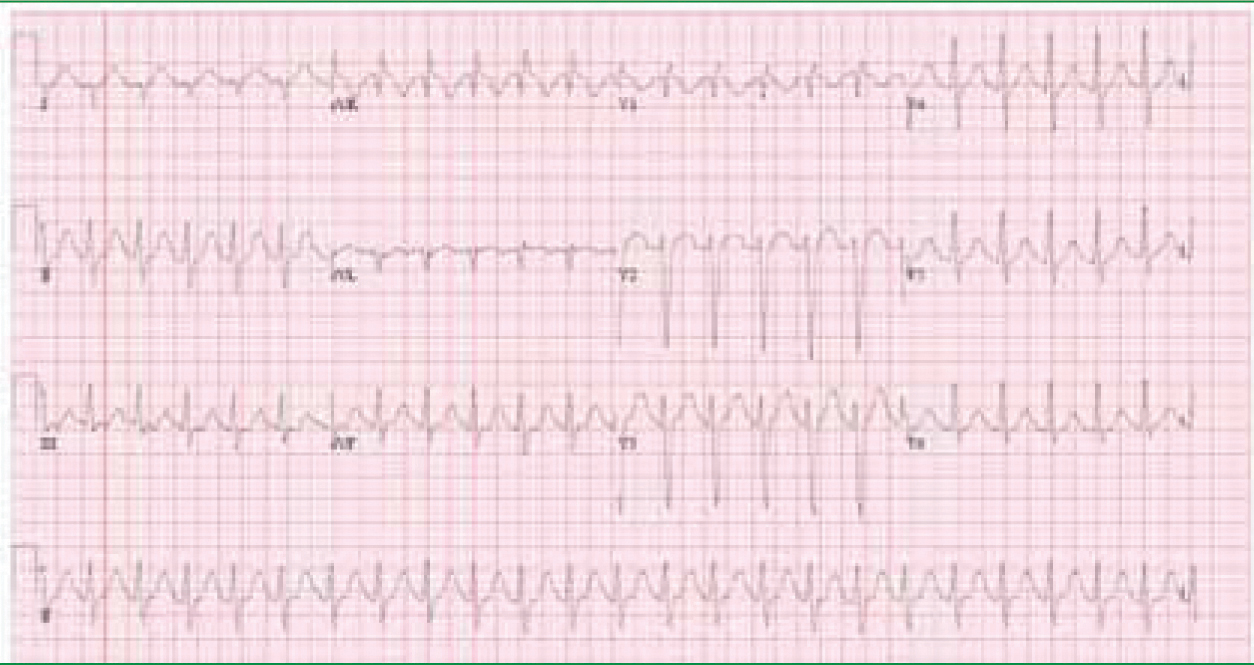
Immediately, the patient was given subsequent 50 mEq boluses of sodium bicarbonate. A repeat ECG, approximately 10 minutes after sodium bicarbonate administration (Figure 2), demonstrated immediate improvement of the ECG morphology and the QRS duration. The patient became increasingly hypotensive (BP 104/52), requiring three one-liter crystalloid boluses (normal saline).
‘Prehospital care providers and clinicians face several challenges when managing patients following TCA ingestions’
An infusion of dextrose 5% in water, with 150 mEq of sodium bicarbonate, was commenced to continue the alkalinization process. Initial laboratory specimens were obtained, and serum/ urine drug tests were sent for evaluation. The patient's neurological status never improved during his 90-minute ED course, and the patient was transferred to the paediatric intensive care unit (PICU) for further monitoring and treatment for presumed TCA ingestion. Toxicology testing was positive for amitriptyline, cyclobenzaprine, oxcarbazepine, and carbamazepine.
The ECG morphology and QRS duration continued to improve in the PICU, with continuous sodium bicarbonate infusion for 48 hours (Figure 3). The patient was extubated 61 hours after arrival in the ED, and the patient was transferred to an inpatient pediatric psychiatric unit following a five-day hospitalization.

Discussion
This case demonstrates the difficulties involved with assessing and treating polypharmacy ingestion in the prehospital setting. Multiple agents are ingested in 44% of fatal pediatric ingestions, underscoring the need for a generalized approach to all patients with unknown ingestion (Kuehl, 2002). The standard of care in the treatment of the poisoned patient includes patient stabilization, limiting toxin absorption, increasing elimination, and providing specific antidotes when indicated.
In the prehospital setting, differing protocols determine how much of this treatment can be initiated by the EMS providers. This patient presented with symptoms common for polypharmacy ingestions, including altered mental status and abnormal vital signs. The EMS crew appropriately placed the patient on a monitor, placed an IV line, and administered oxygen after establishing a nasal airway. However, the prehospital crew did not gather any of the pill bottles at the scene, making them unaware of the potential for tricyclic antidepressant ingestion and the severe risk of a life-threatening dysrhythmia.
The presence of TCAs in this case adds a further layer of complication as they cause cardiac arrhythmias, altered mental status, and even coma (Fasoli and Glauser, 1981; Niemenn et al, 1986; Lewis-Abney, 2000; Mills, 2000; Liebelt and Francis, 2002; Benowitz, 2004; Unverir et al, 2006; White et al, 2008). Without the knowledge of what toxins are ingested, prehospital providers may be unaware of early symptoms which may become fatal if not addressed. In the US, unintentional pediatric toxic ingestions of TCAs average 1500-1700 cases annually (Litovitz et al, 2000; Litovitz et al, 2002).
Narrow safety margin of TCAs
TCAs are generally considered to have a narrow margin of safety, with a recommended dose in children 6 and over of 1.5–5 mg/kg/day (McFee et al, 2001). Most patients who develop clinical symptoms do so after ingesting >5 mg/kg of TCA (Sasynuik et al, 1986). In addition to other pharmaceuticals, this patient ingested 900 mg of amitriptyline (18 mg/kg).
Although initially developed as an antidepressant, TCAs have a narrow safety margin, resulting in fewer prescriptions for TCAs in comparison to newer and safer antidepressants such as selective serotonin-reuptake inhibitors (SSRIs) (Whyte et al, 2003). However, newer indications for TCAs such as migraine prophylaxis have made their overdose prevalence more common in recent years (Punay and Couch, 2003). In addition, TCAs are relatively inexpensive in comparison to the SSRIs and are therefore more prevalent in lower socioeconomic regions.
Sodium/calcium blockers
TCAs primarily act as serotonin-norepinephrine reuptake inhibitors (SNRIs) by blocking the serotonin transporter (SERT) and the norepinephrine transporter (NET). This receptor blockade results in an elevation of the extracellular concentrations of these neurotransmitters, and an enhancement of neurotransmission (Tatsumi et al, 1997; Pancrazio et al, 1998; Gillman, 2007). However, many of the TCAs in high doses also act as sodium and calcium channel blockers, especially in the high levels seen in intentional overdose ingestions (Pancrazio et al, 1998; Mezzacarpa, 1998; Zahradnik et al, 2008). This sodium/calcium channel blockade is the mechanism for the fatal side-effect profile of TCAs, as blocking these ion channels will create cardiac electrical disturbances including the often fatal torsade de pointes (Marx et al, 2006).
In this case, the patient was found with altered mental status and tachycardia. The EMS team placed a 4-lead ECG on the patient and noted him to be in sinus tachycardia at 160 beats per minute. However, the wide-complex tachycardia in the setting of a presumed ingestion was not recognized by the paramedics and was not addressed en-route to the ED. A potential barrier in this instance would be the lack of equipment and training to institute and interpret a 12-lead ECG. Many EMS agencies across the US use 12-lead ECGs as a routine part of their prehospital care.
Traditional ECG criteria for TCA cardiotoxicity are widening of the QRS interval >100 msec, R wave amplitude of >3mm in lead aVR, and abnormalities in the terminal QRS. These findings on electrocardiography are predictive of seizures and ventricular arrhythmias (Niemenn et al, 1986; Liebelt et al, 1995). However, this particular EMS agency does not use 12-lead ECGs; as such, the presence of a wide-complex tachycardia in this patient was much more difficult to recognize and went untreated. If another EMS agency with electrocardiographic capabilities in our area had transported this patient, these abnormalities may have been recognized.
TCA toxicity
The standard treatment for TCA toxicity in patients with conduction delays or arrhythmias is alkalinization with sodium bicarbonate (Pantel and Benowitz, 1984; Sasynuik and Jhamandes, 1984; McCabe et al, 1994; Lewis-Abney, 2000; Michael and Sztajnkrycer, 2004). Sodium bicarbonate itself is not an antidote for TCAs; however, it corrects the metabolic acidosis associated with TCA toxicity and stabilizes the involved tissues (Bradberry et al, 2005). In addition, sodium bicarbonate alkalinizes the urine and enhances excretion of TCAs out of the body more rapidly via the kidneys.
Lastly, the sodium component of sodium bicarbonate is thought to overload the sodium channel blockade caused by the TCA and negate its cardiotoxicity (Bradberry et al, 2005). Sodium bicarbonate is typically given as a starting IV bolus of 1–2 mEq/kg and is titrated to desired effect (Pentel and Keyler, 2001; Liebelt and Francis, 2002; Michael and Sztajnkrycer, 2004). Multiple doses of sodium bicarbonate (and even continuous infusions) are typically required in TCA overdoses.
Sodium bicarbonate
In this case, even if the paramedics had recognized the wide-complex tachycardia in this patient, they would have been unable to administer sodium bicarbonate due to a lack of protocol in their system allowing the administration of sodium bicarbonate for presumed TCA ingestions. In 2007, the American Association of Poison Control Centers issued an evidence-based practice guideline for the out-of-hospital management of tricyclic antidepressant poisoning, recommending that ‘sodium bicarbonate be given in TCA ingestion if there is a protocol for its use’ (Calkins et al, 2003). Based on this recommendation and others, it is imperative that EMS agencies develop protocols and educate their providers to the use of sodium bicarbonate in selective patients. In our region, the two largest-volume EMS agencies have TCA/sodium bicarbonate protocols; however, several agencies do not have such protocols, demonstrating the need for standardization of these prehospital protocols.
The EMS team did recognize that the patient was severely ill and attempted to transport the patient to the closest facility. However, EMS was diverted from the closest facility to the tertiary care children's hospital, increasing the transit time to twenty-seven minutes—thereby delaying definitive airway management and antidote administration. Throughout this period, EMS documented the patient's Glasgow coma score as 8, yet did not provide positive pressure ventilation.
In a patient with a presumed ingestion and low GCS, many paediatric emergency medicine physicians would recommend airway protection and maintenance with an advanced airway. Although this may be difficult without pharmaceutical intervention to allow for rapid-sequence intubation, it is imperative to adequately manage the airway with positive pressure ventilations if a patient is hypoventilating.
Conclusion
This case demonstrates the many challenges that prehospital providers face in diagnosing and treating polypharmaceutical ingestions, specifically those involving tricyclic antidepressants. There are a myriad of organ systems affected by TCA-toxicity—most importantly, the cardiac and neurologic systems. EMS must consistently gather all applicable information from the scene to effectively treat the patient and then to communicate findings to hospital personnel. The awareness of the prehospital team to list/collect all pharmaceuticals and alcohols found on the scene will direct care more effectively and efficiently.
Although the use of TCAs as an antidepressant is waning, the use of TCA for migraine prophylaxis is becoming common. A known history of migraines can suggest that a TCA is the possible toxic agent.
This case also underscores the need for standardization of care across EMS agencies. If this patient had been evaluated and treated by other EMS agencies in our community, the access to resources (electrocardiography) and evidence-driven protocols (sodium bicarbonate) may have affected the patient's clinical course and outcome.
