Paediatric out-of-hospital cardiac arrest (POHCA) resuscitation is a high-stakes, low-frequency event associated with high rates of stress among emergency medical services (EMS) practitioners (Guise et al, 2017).
While significant progress in survival from OHCA has been made as a result of an emphasis on high-quality cardiopulmonary resuscitation through initiatives such as the Resuscitation Academy, little has been made in POHCA survival. A number of studies have documented low-quality CPR as well as delays in critical actions in resuscitation, such as medication administration and airway management during POHCA (Sutton et al, 2016; Bahr et al, 2021).
POHCA is a rare event (Atkins et al, 2009; Kämäräinen et al, 2010; Tress et all 2010; Fink et al, 2016; Okubo et al, 2020). It presents a number of challenges for prehospital providers. Epidemiologic and physiologic differences between children and adults mean that resuscitation algorithms differ between paediatric and adult advanced life support (ALS), and both medication dosing and equipment size vary according to weight and size. These differences have led to suggestions that a resulting increased cognitive load may contribute to adverse safety events, including medication dosing errors and protocol confusion (Hoyle et al, 2020).
One strategy to reduce cognitive load during POHCA resuscitation is the use of cognitive aids and paediatric resuscitation guides (Luten et al, 2002; Bernius et al, 2008; Nelson et al, 2008; McLanders et al, 2017; Moore et al, 2020; Topjian et al, 2020; Jahn et al, 2021). Over the past few decades since the American Heart Association first published the Pediatric Advanced Life Support (PALS) guidelines in 1988 (Topjian et al, 2020), numerous paediatric resuscitation guides have been developed for use in both hospital and prehospital settings (Wells et al, 2013; Lowe et al, 2016; 2017; Manyoni et al, 2019; Wells, 2019). Little is known, however, about the range, scope and field use of these resources, particularly in the prehospital setting.
This brief report examines the current state of resource use in POHCA by EMS providers in the United States. The authors hypothesised that EMS providers use more cognitive aids in paediatric than in adult resuscitation. They also hypothesised that the EMS agencies with a paediatric emergency care coordinator (PECC) or a larger paediatric volume would have a more uniform and efficient approach to resource usage.
Methods
A survey study of 39 EMS agencies across six states of the United States was carried out. The survey (Appendix A, online) was developed as part of a larger study examining preventable serious adverse effects during POHCA with the intention of better understanding organisation-level factors that affect POHCA care.
The survey requested the demographic variables of each agency, including the number of providers, paediatric call volume and presence of a PECC. Subsequent questions focused on the frequency of paediatric training, development of paediatric protocols, paediatric case reviews and types and numbers of cognitive aids used in both adult and paediatric cardiac arrest. The study was approved by the Oregon Health and Science University institutional review boards.
Recruitment emails were sent to the 41 EMS agencies that had previously collaborated on research and had existing relationships with the primary investigators. The authors emailed the medical directors of the agencies and informed them of the purpose of the study.
Two emails were sent 2 weeks apart with links to online survey platform SurveyMonkey. If the online survey had not been completed in 4 weeks, a mail version of the survey was sent to the medical director. Finally, if no response had been received within 8 weeks, they were contacted by phone. The responses were collected from April 2021 to April 2022.
The authors also obtained and evaluated protocols in different states of the country with various EMS system designs. These included: dual advanced life support (ALS); public fire and private transport response; and single ALS response from public ALS transport.
Using these data, the authors analysed the total number and frequency of various cognitive aids. One-way ANOVA was used to evaluate for statistical significance between the groups. The number and type of cognitive aids were stratified by the presence of a PECC and paediatric call volume level.
Finally, the authors requested a copy of each agency's local paediatric cardiac arrest protocol via email and searched online for publicly available protocols. The protocols obtained were then compared to PALS guidelines.
Results
Of the 41 agencies contacted, 39 from various regions in the United States, including California, Georgia, Oregon, Pennsylvania, Washington and Wisconsin, responded to the survey.
Annual paediatric call volume ranged from 15 to 11 000 calls. Using volume categories based on National EMS Data Analysis Resource Center reporting standards, call volume interquartile ranges (EMS Data Center, 2021) and total sample size, the agencies were divided into low (15–165 calls/year), medium (199–656 calls/year), and high (1,207–11 000 calls/year) paediatric call volumes. There were 12, 14, and 11 agencies in each category respectively (two agencies did not answer the call volume question). Fifteen of the 39 responding agencies reported having a PECC.
The number of available paediatric resources for cardiac arrest ranged from 0 to 4. The mean was 2.6 (SD 1.0), with a median of 3. When asked how many resources were used during paediatric resuscitations, the average number was 2.0 (SD 0.5). For comparison, in adult cardiac arrest, the average number of resources available and used were 1.1 (SD 0.7) and 1.1 (SD 0.6), respectively (Table 1).
Table 1. Adult versus paediatric: mean number of out-of-hospital cardiac arrest resources available and used in the field
| Adult | Paediatrics | |
|---|---|---|
| Number of resources available in the field | 1.1 (SD 0.7) | 2.6 (SD 1.0) |
| Number of resources used in the field | 1.1 (SD 0.6) | 2.0 (SD 0.5) |
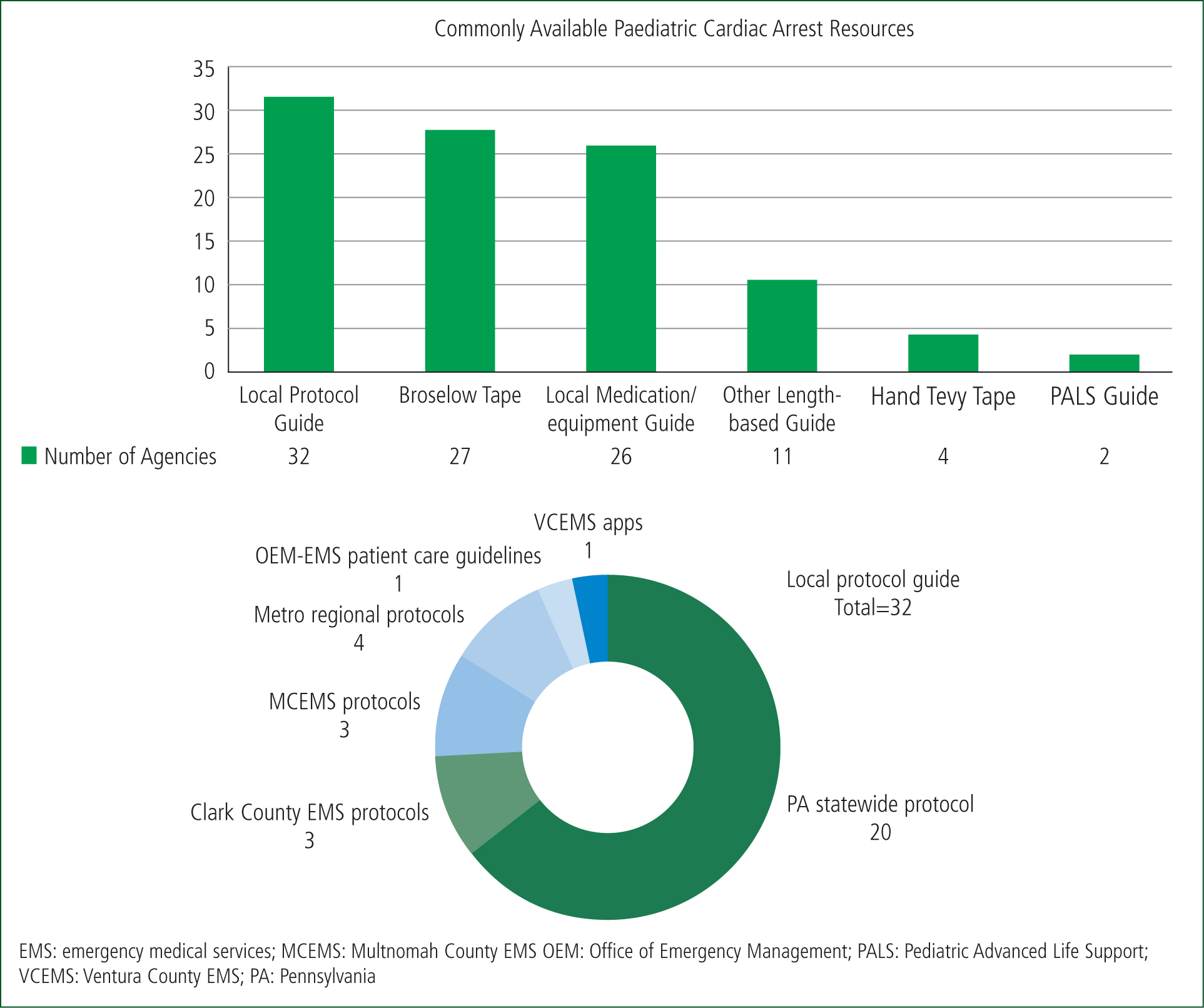
The most commonly available paediatric resource in the field was a local protocol guide (32/39; 82.0%), followed by Broselow tape (27/39; 69.2%) and a local medication/equipment guide (26/39; 66.6%). The least commonly available resource was a PALS card (2/39; 5.1%). The range and frequency of paediatric resources are depicted in Figure 1.
Stratified analysis regarding the presence of a PECC and different call volume categories did not reveal any correlation between in the number of paediatric resources available and used (Tables 2 and 3). To confirm there was no statistically significant difference, two one-way ANOVA tests were conducted to test the variance between PECC groups and call volume categories with respect to their number of resources. No significant difference was found between the presence of a PECC or local call volume and the number of resources (Tables 2 and 3).
Table 2. Mean number of paediatric emergency care coordinators (PECCs) available and used in the field
| PECC present | PECC absent | P | |
|---|---|---|---|
| Number of PECCs available in the field | 2.9 (SD 0.5) | 2.4 (SD 1.2) | 0.46 |
| Number of PECCs used in the field | 2.1 (SD 0.4) | 2.0 (SD 0.4) | 0.79 |
Table 3. Annual pediatric call volume: mean number of resources available and used in the field
| Total number of agencies (n=39) | Low volume (n =12) | Medium volume (n=14) | High volume (n=11) | P | |
|---|---|---|---|---|---|
| Number of resources available | 3.0 (1.0) | 2.6 (1.0) | 2.5 (0.9) | 0.10 | No answer to the call volume question (n=2) |
| Number of resources used | 2.2 (0.4) | 1.9 (0.3) | 2.1 (0.6) | 0.32 |
As most of the agencies (35/39; 89.7%) had multiple resources available, they were asked if any of these resources were combined into a single source. Thirty-two agencies (82.1%) stated that some resources were provided in a combined form. Of these 32 agencies, 25 (78.1%) reported this was provided in a digital format. The remaining seven agencies (21.8%) used a physical book as a combined source (Table 3).
Agencies were asked about the availability of digital resources. Thirty-one (79.5%) reported that at least one resource was available in digital format. Among the agencies that said what these were, the most commonly digitised resource was a local protocol reference (nine agencies). Handtevy was the second most frequently used electronic resource (four agencies).
Finally, the authors obtained local protocol examples by searching online or requesting them from each agency. Nine local protocols were collected. In Pennsylvania, all 20 agencies shared a uniform statewide protocol. In California, Oregon, Washington and Wisconsin, two different protocols were used in each state. The authors were unable to locate the paediatric cardiac arrest protocols for the agencies in Georgia.
Of the nine local protocol references available to the authors, four were modified but similar versions of the PALS algorithm. Three suggested referring to the adult cardiac arrest algorithm with an addendum of paediatric dosing for medication and defibrillation energy. The last two protocols did not include an algorithm but listed possible aetiologies of paediatric cardiac arrest and medication dosing.
Table 4. Availability of combined resources
| Resources combined? | Format | Number of agencies |
|---|---|---|
| Yes (32) | Electronic | 25 |
| Book | 7 | |
| No (7) | Not applicable | 7 |
Discussion
In this study of 39 EMS agencies in six states, a wide range of individual paediatric resources for paediatric cardiac arrest resuscitation were identified. The majority of agencies reported 2–3 separate resources, most commonly in the form of a local protocol book and a separate equipment and medication guide. As hypothesised, the mean number of available paediatric resources for cardiac arrest (2±1) was twice the average reported for adult cardiac arrest (1.1±0.6). While 32/39 agencies had combined multiple resources into a comprehensive digital or paper resource, the most common practice was separating treatment algorithms (the ‘what’ of resuscitation) from medications and equipment (the ‘how’ of resuscitation). This raises concerns as to whether the number and range of cognitive aids reduce or add to the cognitive load during POHCA resuscitation.
No difference in the number of resources between the agencies with a PECC and those without was found. This suggests uncertainty regarding the optimal number of resources in paediatric critical resuscitations as there is no clear guideline on how many resources are most efficient.
Consistent with the direction of general medical references, most of which are now digitised, the majority of the EMS agencies (25/39) surveyed had digitised protocols readily available for use in the field. Conceptually, digital resources, whether PDF files with hyperlinks and searchable functions or a fully developed mobile application, may be easier to use than a physical book. For example, when an EMS provider is looking up the paediatric cardiac arrest protocol on a digital resource, a page may contain hyperlinks to adrenaline dosage and endotracheal tube size according to the patient's estimated weight. Performing the same task with a physical book inevitably takes longer and may be more prone to errors.
A few studies have examined the effect of digitised cognitive aids on EMS providers' performance (Lacour et al, 2021; Siebert et al, 2021; Corazza et al, 2023). A group in Switzerland examined the effects of using a mobile app called Pediatric Accurate Medication in Emergency Situations (PedAMINES) during simulated resuscitations.(Lacour et al, 2021; Siebert et al, 2021). Lacour et al (2021) reported that the paramedics who used the mobile app during simulated cardiac arrest scenarios had smaller changes in stress response than those in the control group. Another study found that when paramedics used this mobile app, the proportion of medication errors and mean time to drug delivery were reduced significantly compared to the conventional methods (Siebert et al, 2021). A more recent study demonstrated that during a cardiac arrest simulation, the group that was using an app (PediAppRREST) had fewer deviations from the American Heart Association (AHA) PALS guidelines and better team performance than the group using reference cards or no resources (Corazza et al, 2023). Given these findings, it is reasonable to encourage the incorporation of digital cognitive aids in a high-stakes task such as paediatric cardiac arrest resuscitation.
PALS cards were available at only two agencies of the 39 surveyed. As PALS from the AHA is regarded as the standard care of paediatric resuscitation in the United States, this finding raises questions. The relatively high cost of PALS certification may be a barrier for many EMS agencies. When the authors compared the available local protocols to PALS, only four protocols out of nine, covering 23 agencies, included algorithms similar to PALS. Even when algorithms resembled PALS, they commonly included modifications. The modifications covered the inclusion of practice scopes at each training level, disposition at the end of the algorithm, such as termination of resuscitation, and specification of medication dosing. The additions and changes likely reflect individual agency needs more precisely. However, it is vital to recognise the risks of modifying national treatment guidelines, and vigilance should be maintained around adhering to a standardised approach to paediatric cardiac arrest.

Three protocols that were used by 11 agencies suggested referring back to adult cardiac arrest algorithms with a section on paediatric considerations. While the basics of cardiac arrest management, such as chest compressions and ventilations, are similar in adult and paediatric patients, the uniform algorithm approach poses a few risks. Adult algorithms may suggest medications and interventions that are less frequently indicated or may even be harmful in paediatric cardiac arrest because of differences in aetiology and physiology. The PALS bradycardia algorithm differs substantially from that for adults.
The authors also identified protocols that list sodium bicarbonate as one of the commonly used medicines in cardiac arrest. Specific indications for sodium bicarbonate, such as hyperkalaemia in end-stage kidney disease, occur more frequently in adults than in children. The routine use of sodium bicarbonate in paediatric cardiac arrest may be harmful (Chang et al, 2021; Cashen et al, 2022).
Another example is airway management. Adult endotracheal intubation is performed relatively frequently by EMS practitioners. This practice is less commonly encountered in paediatrics in the prehospital setting, and substantial evidence suggests that bag-mask ventilation is a reasonable alternative given the high adverse safety event rates during intubation (Gausche et al, 2000; Hansen et al, 2015). Following an adult algorithm may motivate EMS personnel to intubate, which may not be beneficial in the paediatric population.
Conclusion
The authors identified a wide variability of resources available to support EMS providers in the resuscitation of infants and children with out-of-hospital cardiac arrest.
As hypothesised, the number of resources used during POHCA resuscitation was higher than in adult resuscitation.
No differences were found regarding the number of resources available or used for POHCA in agencies that had PECC staff compared with those that did not. This underlines the need for the identification of optimal POHCA resource numbers and use.
Future studies might focus on the most effective way to use cognitive aids in paediatric cardiac arrest and measure their impact on cognitive load and performance.
Key Points
- Paediatric out-of-hospital cardiac arrest resuscitation is rare and associated with high rates of stress in emergency medical services (EMS) practitioners
- The study finds EMS providers use more resources for paediatric cardiac arrest than adults
- There is a notable shift towards digital protocols for better accessibility during critical scenarios
- Variations in local protocols emphasise the need for standardised approaches in paediatric cardiac arrest management
CPD Reflection Questions
- In what ways can EMS providers use resources in paediatric cardiac arrest to lessen their cognitive load?
- Could limiting the number of cognitive aids used in critical clinical scenarios increase efficiency in patient care?
- Does digital form of cognitive aid enhance performance in patient care compared to the physical form?


