LEARNING OUTCOMES
After completing this module, the paramedic will be able to:
- Understand that patients may present with total coronary occlusion without meeting ST-elevation myocardial infarction criteria on an electrocardiogram
- Recognise that these patients may present with atypical acute coronary symptoms
- Understand the benefits of direct transportation to a percutaneous coronary intervention centre and when this is appropriate
- Identify the criteria for high-risk electrocardiograms
If you would like to send feedback, please email jpp@markallengroup.com
Broadly, acute coronary syndrome (ACS) transport decision-making has involved conveying patients with ST-elevation myocardial infarction (STEMI) to percutaneous coronary intervention (PCI) centres and those with other suspected ACS to the closest emergency department for investigation.
Recent advances in ECG interpretation, in conjunction with a review of the recent literature, prompt the need for paramedics to review their understanding of electrocardiograms (ECGs).
ECG changes not consistent with STEMI criteria are traditionally thought to be linked with partial occlusion (Terlecki et al, 2021). However, advances in ECG interpretation and research indicate that up to 28% of people with non-ST-elevation myocardial infarction (NSTEMI) may be experiencing a total occlusion (McLaren et al, 2022). The incidence rate for NSTEMI is higher than that of STEMI; they account of 60% and 40% of myocardial infarction (MI) cases respectively (Mol et al, 2016). These findings indicate there is a cohort of patients who should be considered for urgent reperfusion at PCI-capable hospitals (Hillinger et al, 2019; Faour et al, 2022).
For this group of patients, definition issues arise through the known limitations of the STEMI versus NSTEMI paradigm (McLaren et al, 2022). This is addressed with occlusion criteria defining an infarction based on the suspected presence or absence of an occlusion (McLaren et al, 2022). Other attempts to identify this cohort of patients have given rise to terms such as ‘STEMI equivalent’ or ‘high risk’ to distinguish them from STEMI and NSTEMI (Palladino et al, 2021; McLaren et al, 2023). This article will refer to these ECGs as ‘high risk’.
Despite the issues surrounding terminology, the literature concludes that patients with a suspected high-risk NSTEMI will benefit from early prehospital treatment and transport to a PCI-capable hospital (Shaul et al, 2017; Anroedh et al, 2018; Terlecki et al, 2021; McLaren et al, 2022). Total coronary occlusions are associated with higher mortality rates than partial occlusions (Terlecki et al, 2021).
Novel guidelines in some services recognise that this cohort of patients may require direct transport to a PCI centre (Reed et al, 2016; Anroedh et al, 2018). Where such guidelines are not in place, if a paramedic identifies a patient with a high-risk ECG and a supporting history of ACS, they could consider transport to a PCI centre.
High-risk patients
Compared to a STEMI, an NSTEMI presentation is more likely to be atypical in nature (Ängerud et al, 2019). As NSTEMI patients are less likely to identify their symptoms as cardiac, this leads to a median delay of an additional hour so medical contact occurs after 2–5 hours (Mol et al, 2016; Ängerud et al, 2019). However, Australian patients tend to call emergency services earlier and are thus less likely to wait than their European counterparts (Mol et al, 2016).
High-risk groups that are more likely to experience an atypical presentation with a delayed time to medical contact include women and those with existing comorbidities including diabetes, heart failure, hypertension, dyslipidaemia and previous acute MI (Mol et al, 2016; Khand et al, 2020; Cha et al, 2022). Of note, patients aged >75 years may benefit more from early PCI than younger patients (Pavasović et al, 2018). This is significance as the world's population is ageing (Pavasović et al, 2018).
Early percutaneous coronary intervention
Minimising delays is essential to improving patient outcomes. Transporting patients with an NSTEMI to PCI-capable hospitals is associated with a higher level of appropriate care (Malta Hansen et al, 2018; Rashid et al, 2020).
Early PCI is associated with a reduction in mortality as it minimises ischaemic time (Anroedh et al, 2018). Similarly, it is associated with a reduction in recurrent ischaemia, recurrent MI and the development of morbidities such as cardiac failure (Mol et al, 2016; Badings et al, 2017; Pavasović et al, 2018; Cha et al, 2022).
Other morbidities and risks for survivors of acute MI include stroke, heart valve complications and arrhythmias such as atrial fibrillation, heart blocks and other bradyarrhythmias and tachyarrhythmias (Johansson et al, 2017; Messika-Zeitoun et al, 2022; Frampton et al, 2023).
For patients experiencing an NSTEMI, early PCI is associated with lower mortality at 30 days (Pavasović et al, 2018). This reduction in mortality is not statistically significant within 1–2 years; however, mortality is significantly lower at 3 years and 5 years after PCI (Badings et al, 2017; Shaul et al, 2017; Pavasović et al, 2018; Mahendiran et al, 2020; Fagel et al, 2021; Cha et al, 2022).
There are limitations to these studies as they do not differentiate between total versus partial coronary occlusion, nor do they assess for morbidity. Only one study included the use of ECGs and not all patients enrolled had ECG changes (Badings et al, 2017). The literature concludes that patients experiencing a total coronary occlusion while not meeting STEMI criteria may also benefit from PCI within 90 minutes, which is unlikely to occur if delays were to happen (Palladino et al, 2021).
Reflection 1
Are you familiar with the cohort of patients at risk of atypical acute coronary syndrome presentations?
Reflection 2
Are you familiar with the features of atypical acute coronary syndrome presentations?
Interhospital transfer delays
Delays may occur where patients self-present or ambulances convey patients to hospitals that are not PCI capable.
A leading factor in this is a lack of prehospital triaging systems that allow these patients to be referred to PCI centres (Demandt et al, 2022). This also leads to an increase in interhospital transfers, further burdening ambulance services (Demandt et al, 2022).
In London, interhospital transfers may add a 35-hour delay to PCI (Reed et al, 2016). Delays with interhospital transfer result in higher rates of cardiac-related death within 2 years (Kang et al, 2021; Rashid et al, 2020).
Where triage guidelines are in place, there is an overall reduction in interhospital transfers and better patient outcomes (Reed et al, 2016).
Direct transport to a percutaneous coronary intervention centre
It is evidenced that delays lead to adverse outcomes, while early PCI leads to improved outcomes (Anroedh et al, 2018; Palladino et al, 2021). Ambulance services therefore have a significant role in advocating for this cohort of patients to be transported directly to a PCI-capable hospital.
The use of ambulance services has been found to be the single most important factor in reducing prehospital times for NSTEMI patients while also reducing mortality (Cha et al, 2022). This may be particularly important where patient delays contribute to adverse outcomes.
For NSTEMI, the use of prehospital ECG is associated with a reduction in mortality, and in-hospital mortality rates are 2.1% lower in PCI-capable hospitals (Rashid et al, 2020; Eckle et al, 2021).
When paramedics convey those with suspected NSTEMI directly to a PCI-capable hospital, this is associated with improved outcomes, with patients being twice as likely to receive early PCI (Koganti et al, 2016; Rashid et al, 2020; Kang et al, 2021).
In addition to this, direct transport and admission to a PCI centre mean patients are more likely to have a consultation with a cardiologist and access to other cardiac services such as coronary artery bypass grafting (Rashid et al, 2020). Similarly, it is associated with an overall reduction in invasive intracoronary procedures (van Steenbergen et al, 2023).
Because demand can be high in a PCI centre, consideration should be given to transporting low-risk patients to a local emergency department (Badings et al, 2017; Fabris and Bhatt, 2021).
Benefits of direct transport and prehospital care are summarised in Table 1.
Table 1. Benefits of direct transport and ambulance care
| Ambulance contact is the single most important factor in reducing prehospital times for NSTEMI patients | Patients are twice as likely to receive early PCI | Prehospital care is associated with a reduction in mortality | In-hospital mortality is lower in PCI-capable centres so overall mortality is lower |
| Reduction in morbidity | Patients are more likely to have a cardiologist consultation | Early access to cardiac services | There is an overall reduction in invasive intracoronary procedures |
NSTEMI: non-ST-elevation myocardial infarction; PCI: percutaneous coronary intervention
Reflection 3
What is your understanding of acute coronary syndrome pathophysiology?
Financial and hospital implications
Beyond improved patient outcomes, direct transport to PCI-capable hospitals has other positive effects. Being able to carry out PCI and associated procedures early on means patients spend less time in hospital (Koganti et al, 2016; Badings et al, 2017; Fagel et al, 2021; van Steenbergen et al, 2023). There are financial savings associated with these shorter hospital stays as well as a likely positive impact on patient flow (Koganti et al, 2016; van Steenbergen et al, 2023).
Direct transport to a PCI centre can reduce financial burdens on healthcare services, with an overall reduction in invasive intracoronary procedures and costs of managing lifelong morbidity (van Steenbergen et al, 2023). However, it is not feasible to transport all suspected ACS patients to PCI-capable hospitals as this would put an unnecessary burden on those facilities (van Steenbergen et al, 2023).
International prehospital systems
In London and the Netherlands, dedicated triaging systems recommend transport to a PCI centre for patients presenting with a suspected high-risk NSTEMI (Koganti et al, 2016; Anroedh et al, 2018). This strategy is associated with better patient outcomes (Anroedh et al, 2018). Similarly, the Queensland Ambulance Service ACS guideline recommends that patients presenting with high-risk ECG changes are transported to a PCI centre (Queensland Ambulance Service, 2022).
For these systems to work, paramedics are required to perform accurate ECG interpretation. An English study concluded that London Ambulance Service paramedics can identify a high-risk ECG in the prehospital environment (Koganti et al, 2016). Similarly, Australian paramedics can identify a NSTEMI with a 76.88% accuracy (Wyld et al, 2023).
Accuracy of interpretation is linked with higher levels of education (Prihatiningsih and Hutton, 2018; Mobrad, 2020; Wyld et al, 2023). Where this is possible, paramedics may consider transmitting ECGs to or consultation with a physician, as these are associated with an increase in ECG interpretation accuracy and a reduction in inappropriate PCI centre activations (Funder et al, 2020; Faour et al, 2022).
High-risk electrocardiograms
As ambulance contact is key to positive patient outcomes, paramedics should be aware of this cohort and of high-risk ECGs. Identification of a high-risk ECG with a supporting history of ACS is associated with earlier PCI (Rashid et al, 2020).
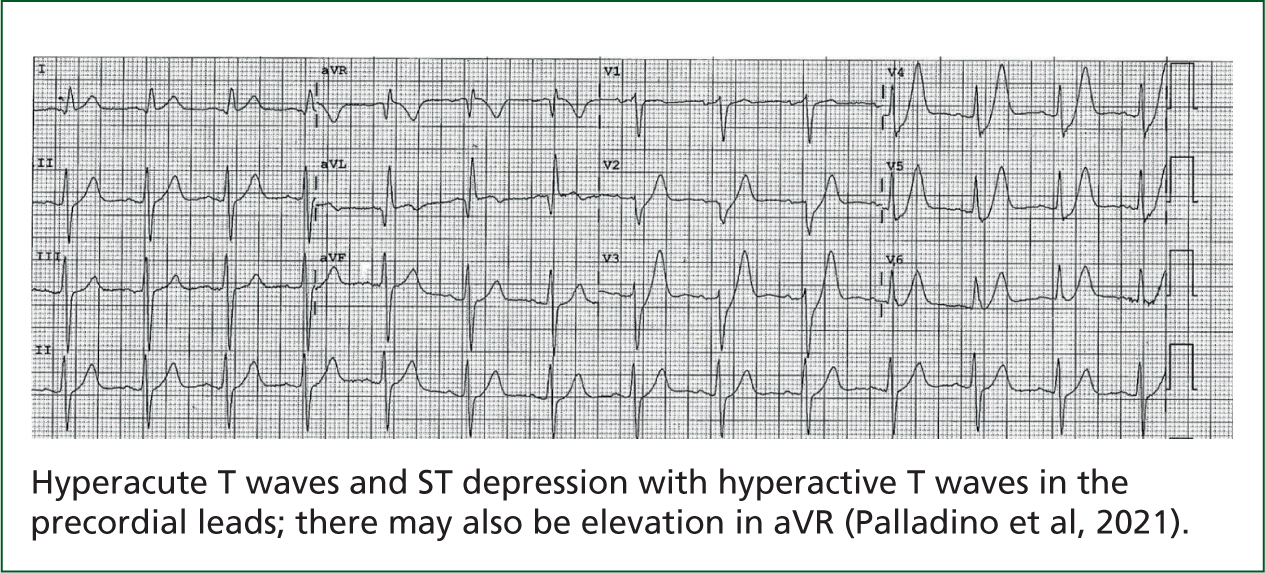
ECG changes of concern include hyperacute T waves and ST depression with hyperactive T waves in the precordial leads shown in Figure 1 (Demandt et al, 2022). Therefore, paramedics should consider transporting patients to a PCI-capable hospital if their ECGs show diffuse ST-depression with elevation in aVR (Figure 2), a de Winter T wave pattern (Figure 1), posterior AMI identified by ST depression (Figure 3), Wellens syndrome (Figure 4) and ST elevation not meeting STEMI criteria (Palladino et al, 2021; Faour et al, 2022; Kubica et al, 2022; McLaren et al, 2022).
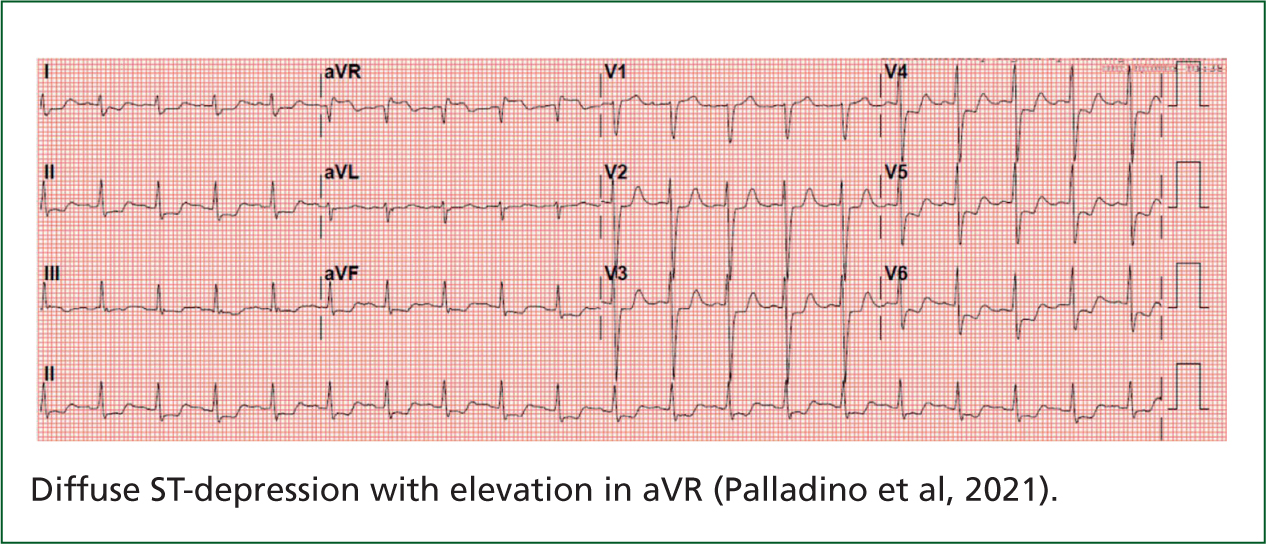

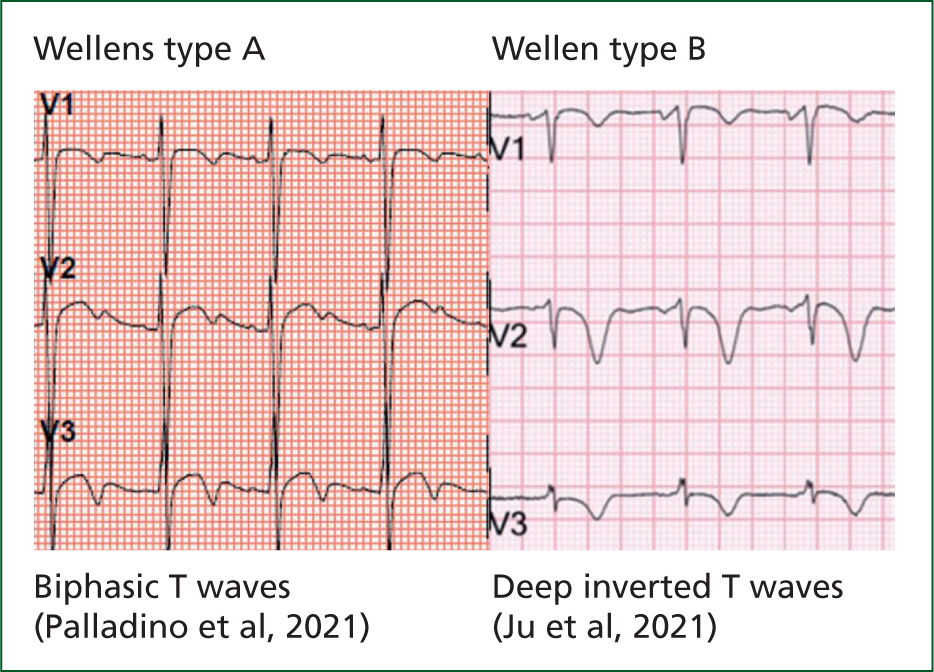
Patients with ECGs that show a left bundle branch block or a paced rhythm that meet the modified Smith-Sgarbossa criteria of ST/S ratios >25% and/or concordant ST depression >1 mm and/or concordant ST elevation >1 mm (Figure 5) are likely experiencing a coronary occlusion (McLaren et al, 2022). Of note, 4.4% of patients who undergo PCI have a prehospital ECG showing Wellens syndrome (Figure 4) or aVR elevation (Figure 2) (Palladino et al, 2021).

Wellens syndrome is a unique presentation of coronary stenosis as it may be pain free, albeit with a history of angina (Ju et al, 2021). ECGs of patients with a history of cannabis and cocaine misuse, pulmonary embolism and cardiomyopathy may show Wellens morphology without coronary stenosis, in a phenomenon referred as pseudo-Wellens (Ju et al, 2021). Paramedics should be aware that ischaemic ECGs will likely evolve, highlighting the importance of serial ECGs for these patients (McLaren et al, 2023).
Reflection 4
Can you identify a high-risk electrocardiogram?
Reflection 5
Could you implement an appropriate transport strategy for these patients suited to your service and area of work?
Conclusion
Supported by the literature and working within the frameworks of their jurisdictional service, paramedics should consider the transportation of patients with a relevant history of ACS and a high-risk ECG to a PCI-capable centre. Continued professional development and education are essential to ensure ECG interpretation is ccurate.


