LEARNING OUTCOMES
After completing this module, the paramedic will be able to:
- Understand that early recognition and rapid removal are key to the effective management of cord prolapse
- Understand the difference in treatment depending upon the distance from the receiving unit
- Determine whether it is acceptable to allow the woman to walk to the ambulance, depending on the distance, as this is often quicker than the removal of the stretcher to bring to her
- Prioritise the safety and security of the woman in the ambulance, with the awareness that she must always be secured within the 4-point harness
If you would like to send feedback, please email jpp@markallengroup.com
A prolapsed cord is defined as the umbilical cord below the presenting part of the foetus in association with ruptured membranes. It is not always visible as a long loop of cord protruding from the vagina; in cases where midwives are present, the cord may have just been felt on the internal examination. The prolapsed cord is a time-critical emergency and rapid extrication and transport are always required (Figure 1).
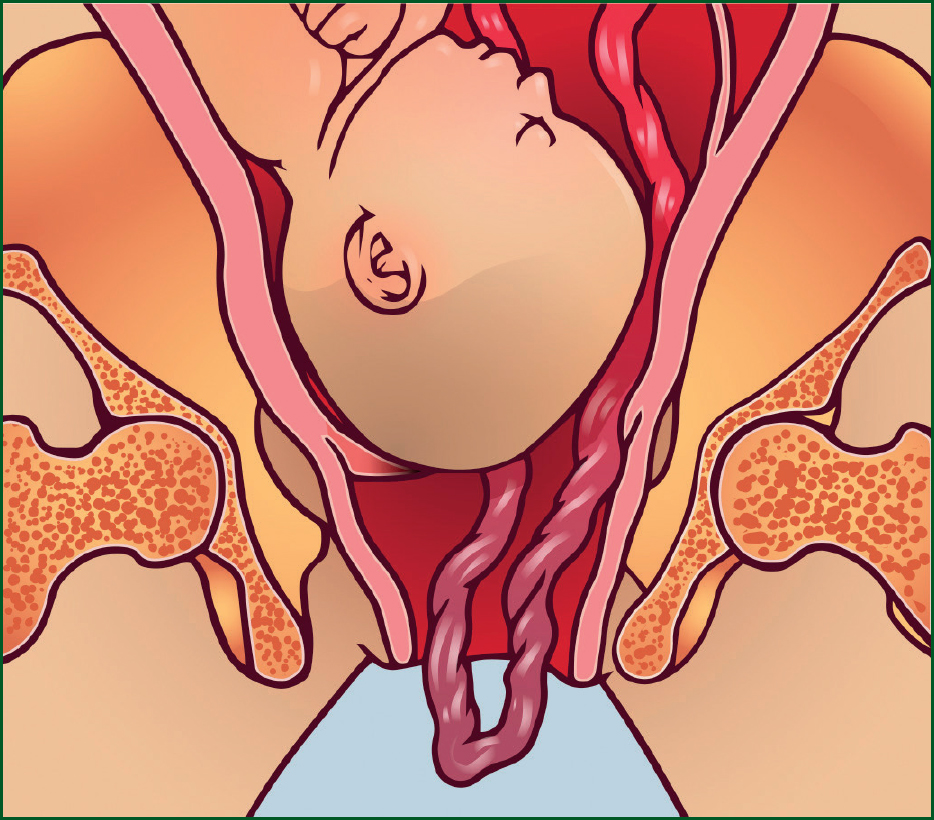
The umbilical cord is the baby’s only source of oxygen. Therefore, pressure exerting on the cord from the presenting part will decrease the amount of oxygen received, putting the baby at increased risk of hypoxia and brain injury.
There is limited evidence available about the correct procedure for prehospital treatment of the cord. There is evidence, however, that overhandling of the cord will lead to vasospasm within the vessels, cutting off the blood supply quicker (Association of Ambulance Chief Executives (AACE), 2024). Therefore, minimal handling is advised. For midwives in the community, carrying a foly catheter to fill the bladder with 500–700 ml ofss saline and wclamping it off will elevate the presenting part during transport to hospital (Royal College of Obstetricians and Gynecologists (RCOG), 2014). This is often performed simultaneously with calling 999 for ambulance transportation.
The incidence of cord prolapse occurs in 0.1–0.6% of pregnancies; this however increases to 1% in the breech presentation (RCOG, 2014). Even when obstetric facilities are available, the outcome from a cord prolapse is usually poor. Prognosis is even worse if this occurs outside a maternity hospital. Some evidence suggests that there is a ten-fold increase in perinatal mortality if a cord prolapse occurs outside of the hospital setting (Kooning et al, 1990).
Cases of cord prolapse consistently feature in perinatal mortality enquiries, because of their high mortality rate – especially prehospitally. One study found a perinatal mortality rate of 91 per 1000 births (RCOG, 2018). Perinatal death has been associated with term babies, especially during home births. Delay in diagnosis because transfer to hospital is required appears to be a contributing factor (RCOG, 2018).
Reflection 1
Have you heard of any cases of cord prolapse from from within your area and are you aware of the outcome?
Risk factors
The main risk factors for cord prolapse are as follows (RCOG, 2014):
- Multiparity
- Low birthweight (<2.5 kg)
- Preterm labour (< 37+0 weeks)
- Fetal congenital anomalies
- Breech presentation
- Transverse, oblique and unstable lie
- Second twin
- Polyhydramnios (increased amount of amniotic fluid)
- Unengaged presenting part
- Low-lying placenta.
Treatment and management
Cord prolaps is a time-critical emergency. It requires immediate intervention, and rapid removal and transfer to a consultant-led obstetric unit. However, it is vital to ensure the safety of the woman and her security in the vehicle at all times.
The cord that has prolapsed ideally needs to be kept warm to prevent spasm. Once a cord prolapse is identified, this is now a time-critical situation.
Solo responders should assist the woman in replacing her underwear containing a clean dry pad. The cradling of the cord against the external genitals should assist to keep the cord warm. The woman should then be placed into the knee-chest position while awaiting the transporting vehicle (Figure 2). It is vital, however, that the woman is never transported in this position. The woman’s safety is paramount so must always be strapped in using the 4-point harness at all times. Then once the ambulance arrives, assist her in walking out to the ambulance.

If arriving as a transporting response, following diagnosis of cord prolapse, time on scene should not be delayed and the woman should be assisted to walk out to the awaiting ambulance immediately following the replacement of her pad and underwear. Sitting on a carry chair should be avoided if possible as this may cause further pressure on the already compromised cord.
Once the mother is secured on the ambulance trolley, she must be positioned into the exaggerated Simms position (Figure 3) with her hips raised as much as possible to relieve pressure on the cord. Place a pre-alert message and travel under emergency conditions asking where possible to be met at the maternity unit door to enable a swift entrance to the unit.

If the woman is in labour and experiencing contractions, the administration of entonox may help to prevent the woman from pushing, which would again increase pressure on the cord. However, if she is in the second stage of labour and the presenting part is visible, the woman can be encouraged to push, as this will expedite the birth. If the woman gives birth and the baby has had a cord compression, be prepared to perform newborn resuscitation.
Again, do not delay time on scene. Transfer the woman quickly and then place a pre-alert to the nearest consultant obstetric facility stating that you have a visible cord prolapse. You may also consider asking the staff to meet you at the ambulance entrance to enable rapid access to the unit. If there is a midwife on scene who has made the diagnosis prior to your arrival, they may consider bladder filling as a midwifery intervention; however, do not delay time on scene by waiting for a midwife to arrive. Proceed with rapid transport to the nearest consultant obstetric facility.
Reflection 2
Complications of birth prehospital remain low. However, how many of these risk factors have you heard of happening or have you witnessed in practice?
Reflection 3
Why is it so dangerous to transport in the knee-chest position? Who is liable if an incident occurs and the patient is not correctly strapped / positioned?
Case study
You are responding to a 38-year-old lady on her 5th pregnancy, having had four previous normal births (G5P4). She has called her maternity unit telling them that her waters have broken and now she can feel something strange dangling out. The midwife tells her to call 999 and sit on the floor with her bottom in the air.
Reflection 4
Do you know the location of all the obstetric units on ‘your patch’? Would you be confident in knowing how to get into them in an emergency situation?
Reflection 5
This will inevitably be an extremely stressful situation for all involved. What phrases could you use to help reassure the woman and calm her?
Case study activity
When you arrive, you find her panicking on the floor and unable to stop crying. What are you going to do?
- Try and calm her
- Gain permission to expose and examine.
You notice a loop about 2 inches long of thick pulsating cord. What are your next actions? Place the following steps in order:
- Place her in exaggerated Simms positioning with safety belts raising hips upward
- Continually explain what is happening
- Pre-alert and time-critical transfer to the nearest consultant obstetric unit
- Keep her calm
- Walk her to the ambulance
- Place a clean dry pad in and replace her underwear.
The correct order of actions is as follows:
- Keep her calm
- Place a clean dry pad in and replace her underwear
- Walk her to the ambulance
- Continually explain what is happening
- Place her in exaggerated Simms positioning with safety belts raising hips upward
- Pre-alert and time-critical transfer to the nearest consultant obstetric unit.
Conclusion
Prompt recognition of the visible cord and rapid transport to the appropriate destination is essential in the attempt to preserve fetal life. Maternal position is vital in order to remove pressure on the cord during transfer. It is imperative that the mother is secured in the ambulance appropriately to prevent further harm, including a 4-point harness.


