There is variability in the reported proportion of the population who identify as LGBTQIA+ (lesbian, gay, bisexual, transgender, queer/questioning, intersex and asexual) because of several confounding factors in data collection. These include differing definitions in surveys when data are being collected (Carman et al, 2020), ambiguity in data collection tools (Australian Bureau of Statistics, 2022) and a suggested reluctance to disclose LGBTQIA+ status in survey responses (Wilson et al, 2020; House of Commons Library, 2023). This lack of data detrimentally impacts the development of policy and understanding of needs, meaning it is not possible to accurately estimate the impact of bias toward this group. However, LGBTQIA+ population estimates are between 3% and 11% in Australia (Australian Human Rights Commission, 2014; Carman et al, 2020) and 6.3% in England and Wales (House of Commons Library, 2023).
Irrespective of the proportion of the population, insights into the community's inequity when accessing healthcare, experiences of stigma and their overall poor health outcomes have been previously documented (Higa et al, 2014; Russell and Fish, 2016; McCrone, 2018; Perales, 2019; Mendes, 2021). A recent scoping review from the UK described negative experiences for LGBTQIA+ patients during diagnosis and treatment of cancer, a lack of acknowledgement of family make-up in palliative care, and greater incidence of various mental health presentations, although these were acknowledged as being interpreted in a way that may not have considered broader societal and cultural influences (McDermott et al, 2021).
Similar inequities, especially regarding the incidence of mental health concerns, have been seen in recent Australian research (Hill et al, 2020).
Three-quarters of LGBTQIA+ people who were surveyed as part of an Australian state LGBTQIA+ health survey indicated a greater willingness to use services if they were accredited as inclusive (New South Wales Ministry of Health, 2022). Recent research suggests that LGBTQIA+ people are less likely to seek help or may delay seeking help from health practitioners because they fear discrimination (Bidell and Stepleman, 2017; Hill et al, 2020) or expect they will be treated as inferior when accessing health services (Quaile, 2018).
In contrast to these negative experiences, health professions espouse an ideal of inclusive, person-centred care, taking holistic consideration of social, societal, cultural and psychological factors that may impact the individual (Clinical Excellence Commission, 2024; NHS England, 2024). This ethos should be fostered throughout a practitioner's education and training, with undergraduate degrees providing opportunities to learn and develop knowledge and gain an understanding of all their future patients. Failure in this can lead to poor health outcomes for the patient, increased stigmatisation of societal groups and an greater health burden for the entire community. Although training and education are evolving to address some of these gaps, routine characterisation of care recipients in health education training as not being diverse regarding gender or sexuality is uncommon (Shepherd and Hanckel, 2021). This omission can result in clinicians who lack the confidence to meet these patients' needs (Quaile, 2018).
Australian paramedics provide high- and lowacuity patient management for a wide range medical and traumatic conditions in diverse locations with the only constant aspect being that it is unplanned. Impromptu care means that neither clinician nor patient can prepare for or mediate the interaction. This, combined with the high stress many patients experience when receiving out-of-hospital care, can exacerbate negative experiences. It is therefore imperative that biases are recognised and addressed to prevent possible stigmatisation. Ultimately, a failure to recognise clinician bias and address community diversity within paramedicine education (or any health curriculum) perpetuates LGBTQIA+ stigmatisation and results in poorer health outcomes for this community.
Several health professions have identified LGBTQIA+ stigma as a concern among their students. McNiel and Elertson (2018) found discriminatory behaviour towards LGBTQIA+ patients was prevalent among student nurses, while a study of over 4000 heterosexual medical students reported that approximately 50% of respondents expressed explicit bias, and over 80% exhibited implicit bias against lesbian and gay individuals (Burke et al, 2015).
Similar bias has been recorded among students studying pharmacy, medicine, nursing, dentistry and midwifery (Sekoni et al, 2017). Encouragingly, some programmes have made changes to curricula and these have had a positive impact, improving knowledge and attitudes toward sexuality- and gender-diverse groups (Sekoni et al, 2017).
Although there have been investigations of LGBTQIA+ paramedicine students (Clarkson et al, 2022) and experiences of gay and lesbian paramedics (Clarkson, 2014), to the authors' knowledge, no original research has investigated paramedicine student bias toward LGBTQIA+ people.
Our research provides foundational knowledge on the prevalence of bias among paramedicine students toward the LGBTQIA+ community. The data are necessary to develop educational or training interventions and to take a small step toward closing the health gap and promote inclusive, person-centred paramedicine care.
Methods
This prospective, cross-sectional, quantitative study used a survey methodology. Participants were Australian or New Zealand students on undergraduate paramedicine courses and were recruited through two large Australian universities (one a multi-campus institution), paramedicine student social media groups and snowballing. Ethics approval was provided by the Western Sydney University Human Research Ethics Committee (H13530).
All participants were invited to undertake an online survey where they completed the Riddle scale (Minnesota State Department of Education, 1994; Gay Lesbian Straight Education Network (GLSEN) Lunch Box, 2002) and several demographic questions. The scale is a validated psychometric scale that seeks to understand people's responses to the LGBTQIA+ community and thereby explore the complexity of individuals' long-held beliefs.
As with any data collection tool, there are limitations and benefits to the Riddle scale. It is now >40 years old but it is still regularly used in research studies and by governmental groups supporting LGBTQIA+ education. Although some researchers commend the use of a continuum rather than the binary perspective of the scale (Maine, 2020), other researchers question the use of the scale in trying to falsely push participants toward a position of nurturance (Rasmussen, 2013).
The scale was initially developed in 1974 by psychologist Dr Dorothy Riddle, who was part of a taskforce lobbying for removal of homosexuality from the Diagnostic and Statistical Manual, and it has been adapted multiple times to encompass diversity or local vernacular (Maine, 2020).
It has subsequently been adapted and used in a variety of settings (Grogan, 2014; Gururaj et al, 2023; McLean et al, 2024), including to assess healthcare trainees' beliefs (Lee et al, 2016). Some of the terminology within the scale—e.g. repulsive—could be confronting for some participants, and a trigger warning was included with the survey.
The version used in this study, which was adapted by GLSEN (Gay Lesbian Straight Education Network (GLSEN) Lunch Box, 2002), is termed the ‘Attitudes toward difference scale’ and assesses attitudes to lesbian, gay, bisexual and transgender people.
The abbreviation used in advertising and for information on the survey was LGBT+ (in keeping with the survey) rather than LGBTQIA+. The Australian Institute of Family Studies (2024) notes the evolving nature of this abbreviation and the need for alteration depending on the audience: LGBT+ was used for clarity at the time of data collection.
Analysis methodology of the Riddle scale (Table 1) varies between scholars and there is no consistent approach. Some authors require respondents to rank each of the 16 statements between 1–5 then use an overall score, taking into account reverse scoring for statements 1–4 (Grogan, 2014). Others use the numbered statements and add statements 1, 2, 3, 4 and 7 and reverse score the remaining statements to provide an overall score (Rubini, 2014). Also, researchers use participants' responses to bracketed pairs of statements (1–2, 2–3, 3–4 etc) to indicate attitudes (Lee et al, 2016). Others use the eight described attitudes and ask participants to choose the most appropriate (Finkel et al, 2003).
Table 1. Riddle scale attitudes and characteristics
| Statement pairs | Attitude | Characteristic |
|---|---|---|
| 1–2 | Repulsion | LGBT people are strange, sick, crazy and aversive |
| 3–4 | Pity | LGBT people are somehow born that way and it is pitiful |
| 5–6 | Tolerance | Life for LGBT people is hard; anti-LGBT attitudes just make things worse |
| 7–8 | Acceptance | LGBT individuals are a fact of life that should neither be punished nor celebrated |
| 9–10 | Support | The rights of LGBT people should be protected and safeguarded |
| 11–12 | Admiration | Being LGBT in our society takes strength |
| 13–14 | Appreciation | There is value in diversity. Anti-LGBT attitudes should be confronted |
| 15–16 | Nurturance | LGBT people are an indispensable part of society. |
Adapted from Riddle (1994)
Because of these disparate methods and a lack of previously published psychometric properties relating to the scale, the approach in the present study is detailed here; it takes note of considerations outlined in the original scale and subsequent publications that have used it. The 16 statements in the Riddle scale were bracketed into sequential pairs corresponding to the attitude and characteristics (Table 1).
To ensure that the authors were not overestimating responses, respondents had to agree to both bracketed statements to be classified as expressing a particular attitude. Participants were able to agree with more than one pair of bracketed statements.
Results
This study received 218 responses; one participant began the survey but did not provide consent at the initial question so was therefore excluded. In the remaining 217, there were 28 partial responses. None of the partial responses completed the Riddle scale and some did not complete various demographic questions. This left 189 valid and complete responses available for analysis.
The size of the student population from which this sample was derived is difficult to calculate as the two universities directly involved in recruitment had approximately 1000 students in total at the time of data collection; recruitment through social media allowed students from other universities to participate which could have expanded the population to ~18000.
To ensure participant anonymity, no data were collected in relation to their location or university.
Paramedicine is typically a 3-year undergraduate bachelor's degree in Australasia, although there are some extended courses, dual degrees and other variants; a degree is required to work as a registered paramedic. Respondents were from all years of study, with 55 first-years, 45 second-years and 89 participants studying in their third year or later.
Demographic information, including religious and political affiliations, are shown in Table 2. Some questions provided an ‘other’ option, and respondents would provide a free text response; these are summarised below the table. Because of the small number of respondents at each year level as well as in demographic and Riddle scale category, it was not feasible to undertake a statistical analysis to determine correlation between any demographic data and Riddle scale response.
Table 2. Participant demographics
| Trait | Number (%) |
|---|---|
| Gender | |
| Male | 135(71.5%) |
| Female | 45 (24%) |
| Non-binary | 6 (3%) |
| Transgender | 3 (1.5%) |
| Sexuality | |
| Heterosexual | 112 (59.5%) |
| Bisexual | 38 (20%) |
| Gay | 7 (3.5%) |
| Lesbian | 15 (8%) |
| Othera | 15 (8%) |
| Prefer not to say | 2 (1%) |
| Age | |
| 18–24 years | 148(78%) |
| 25–29 years | 22 (12%) |
| 30+ years | 19 (10%) |
| Race | |
| Caucasian | 159 (84%) |
| Aboriginal or Torres Strait Islander | 1 (0.5%) |
| Middle Eastern | 5 (2.5%) |
| Asian | 12 (6.5%) |
| Otherb | 12 (6.5%) |
| Religion | |
| Anglican | 7 (3.5%) |
| Baptist | 1 (0.5%) |
| Buddhist | 3 (1.5%) |
| Catholic | 26 (14%) |
| Islamic | 1 (0.5%) |
| No religion | 132 (70%) |
| Otherc | 19 (10%) |
| Political preference | |
| Strongly left wing | 28 (15%) |
| Moderately left wing | 65 (34%) |
| Slightly left wing | 28 (15%) |
| Neutral | 58 (31%) |
| Slightly right wing | 5 (2.5%) |
| Moderately right wing | 3 (1.5%) |
| Strongly right wing | 2 (1%) |
Included pansexual, demisexual, queer and asexual
bIncluded mixed race, southern European, European, Pacific Islander, Australian and Hispanic/Latina
cIncluded atheist, agnostic, spiritual, Orthodox, Christian, Pentecostal and Neopagan
Participants were asked if, to their knowledge, they had any interactions with LGBTQIA+ people and nearly all expressed that they had some interaction. Of them, 181 advised that they had LGBTQIA+ friends, 78 said they had LGBTQIA+ family members and 173 said they interacted with LGBTQIA+ people on a regular basis, defined as more than once per month. Many participants responded affirmatively to multiple categories.
Contrary to the positive interactions with LGBTQIA+ people, the students' experiences of LGBTQIA+ education in their curriculum was generally negative. When asked how well their paramedicine degree addressed LGBTQIA+ education, 36 respondents believed it was very poorly done, 77 said poorly, 42 indicated it was fair, 28 noted it was well done and only six believed it was very well covered.
There were a higher number of responses at the appreciation and nurturance end of the Riddle scale, where participants agreed there is value in diversity, that homophobic attitudes should be confronted and that LGBTQIA+ people are an indispensable part of society. However, there were also a few responses (n=33; 4%) at the repulsion end of the scale, showing agreement with the statement that ‘LGBT people are strange, sick, crazy and aversive’ (Gay Lesbian Straight Education Network (GLSEN) Lunch Box, 2002) (Figure 1).
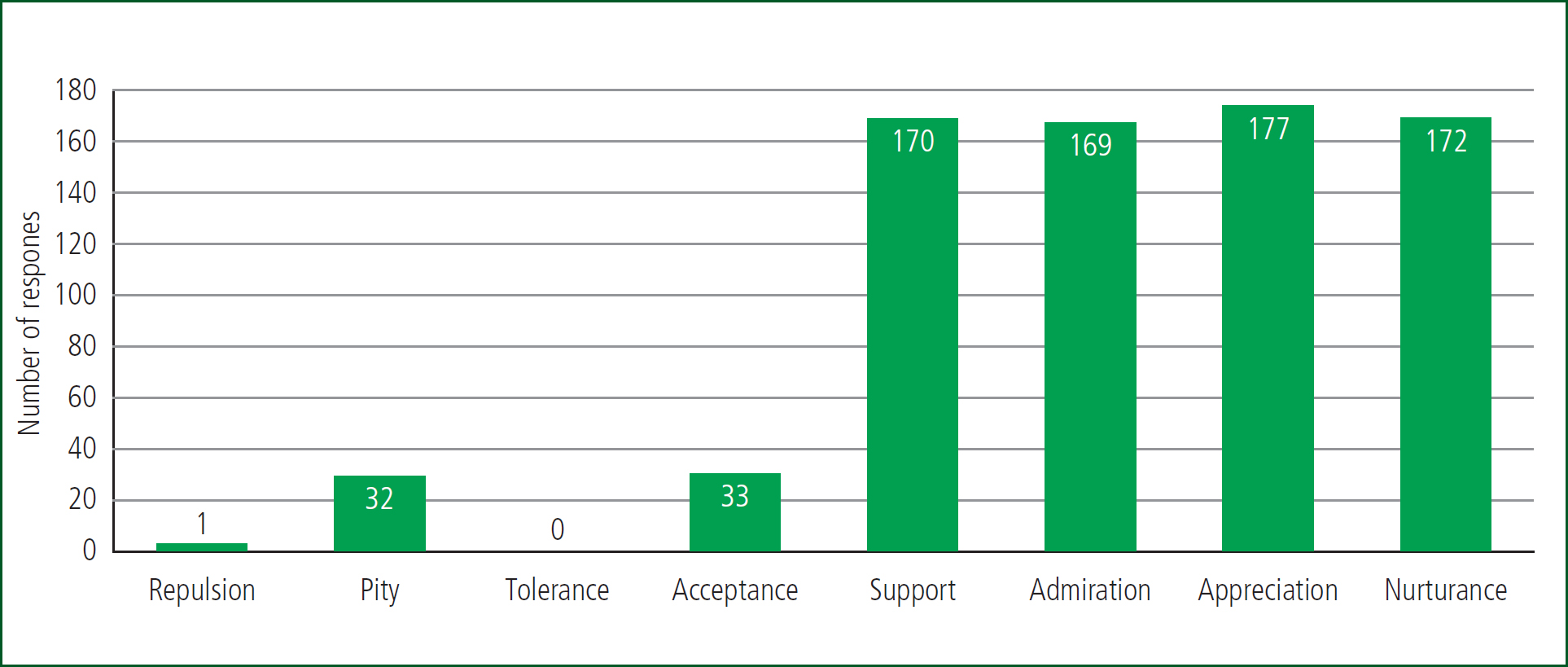
Some participants agreed with more than one attitude so the number of responses is not equal to the number of participants.
Discussion
Our study presents valuable insights into paramedicine student bias toward members of the LGBTQIA+ community. The majority of the Riddle scale responses were positive, suggesting respondent support or appreciate of the LGBTQIA+ community, although reactions of pity and repulsion were also recorded. Although this was not unexpected considering previous literature (Burke et al, 2015; Sekoni et al, 2017; Sileo et al, 2022; Hatzenbuehler et al, 2024), holding such beliefs is likely to perpetuate stigma which can, in turn, contribute towards inequitable healthcare experiences. This is of particular concern when stigmatising beliefs are held by the next generation of healthcare workers.
The main tension we identified was the mismatch between students' positive support and empathy for the LGBTQIA+ community in most cases and their poor experiences of LGBTQIA+ content in paramedicine curricula. Paramedicine curricula have rapidly evolved in the past 20 years from a focus on technical skills to a person-centred care model similar to that for other allied health professions (O'Brien et al, 2014). Yet person-centred care—defined as having mutual respect, sharing clearly communicated information and involving family or carers (Australian Commission on Safety and Quality in Health Care, 2024)—would be challenging to achieve after having undertaken a curriculum lacking LGBTQIA+ content. Omission of content discussing LGBTQIA+ people and their health in curricula can reinforce systems that sideline this community in both education and health; this may lead to clinicians avoiding conversations, miscommunicating or perpetuating underlying biases (McCann and Brown, 2018) and subsequently contributing to the poor health outcomes of the LGBTQIA+ community. Hatzenbuehler et al (2024) discussed the role of structural stigma where policies, institutions and cultural norms can contribute to stigma beyond the interpersonal connections that patients might have with a healthcare worker. This highlights the critical nature of paramedic education designed to examine and deconstruct stigmatised views of members of the LGBTQIA+ community to promote more equitable outcomes.
The poor educational experience is problematic when training future clinicians to work as person-centred paramedics and it also impacts LGBTQIA+ students. Of the survey respondents in the present study, 41% did not identify as heterosexual and therefore are likely to be detrimentally impacted by undertaking a degree where the heteronormative curriculum excludes them. Previous research in paramedicine (Clarkson et al, 2022) and other health professions (McCann and Brown, 2018) has identified similar concerns where LGBTQIA+ students were afraid to discuss their identity for fear of negative responses from both peers and academics.
As would be expected of such a complex problem, there is no single intervention to redress this. Building upon this initial insight, future research that gathers large-scale quantitative or qualitative data may provide insights into contextual factors and guide future work in this area.
Previous authors have noted the important role of critical reflection to identify and amend heteronormative biases (Enson, 2015), appropriate terminology and communication skills education, cultural competence training in both undergraduate programmes as well as ongoing continuing professional development (McCann and Brown, 2018).
Because there has been a historical focus on practical education within paramedicine, it will be essential that future clinical simulations include LGBTQIA+ education and case-based learning that extends beyond stereotypical examples that are likely to reinforce rather than overcome biases (White et al, 2015).
Limitations
As with any study, our research had some limitations and the results should be considered in light of these.
Although an exact response rate could not be calculated as the size of the whole population was not known, there are considerably more paramedicine students in Australasia than there were respondents. This limits the generalisability of these results and also highlights the need for larger studies. Literature from both Australia and the UK has demonstrated that these concerns extend beyond Australasia, and the increasing movement of the paramedic workforce between these countries could support a multinational study.
The group who completed the survey reflected the age and year of study of the wider student population but varied in relation to sex (more natal men responded than in the wider student population) and sexual diversity (greater diversity was present in the sample than reported in the general population). The greater sexual diversity may indicate a self-selection bias although this must be balanced against previous research indicating that people are often uncomfortable reporting sexual identity even in anonymous surveys (Wilson et al, 2020).
Previous critics of the Riddle scale (Rasmussen, 2013) have suggested there may be a response bias, with respondents providing answers they believe are right or desired. These limitations, however, relate to its use in face-to-face groups rather than anonymous surveys as provided in this study.
Conclusions
Australasian paramedicine students are mostly positive in their feelings of support toward members of the LGBTQIA+ community, but generally have a poor opinion of the LGBTQIA+ education within the paramedicine curriculum.
In addition to the detrimental impact on patient care that this may have, previous research would also suggest it negatively influences paramedicine students who identify as LGBTQIA+.
Both findings support the need for further investigation of paramedicine student perceptions of LGBTQIA+ individuals and, most importantly, for concurrent steps to be taken to introduce LGBTQIA+ education into the paramedicine curriculum to generate a learning environment where all students feel safe and understood so can therefore learn to the best of their ability.
Key Points
- LGBTQIA+ people generally have poorer health outcomes than others because of the stigma they experience when accessing healthcare
- The future paramedic workforce – paramedic students – hold mostly positive views toward LGBTQIA+ people, yet a small proportion exhibit repulsion or pity
- The student experience of LGBTQIA+ teaching within their paramedicine curriculum is overwhelmingly poor
- Further research into exemplary educational practices to support paramedics to provide best treatment for LGBTQIA+ patients is required
CPD Reflection Questions
- Undertake the Riddle scale and reflect on your results
- What, if any, education, or training have you received to support your treatment of LGBTQIA+ patients? Was this effective? Why or why not?
- What one change you could make to your practice so that all patients, irrespective of background, feel accepted for who they are?


