The NHS, the UK's publicly funded healthcare system, faces significant challenges, including an ageing population, increasing service demands, and budgetary constraints (NHS England, 2019). These challenges underscore the critical importance of effective leadership at all levels to navigate these complexities and ensure the delivery of high-quality, patient-centred care (Rolewicz et al, 2024). The COVID-19 pandemic has exacerbated these problems, highlighting the critical importance of strong leadership in ensuring high-quality, patient-centred care (Rolewicz et al, 2024).
In response to these issues, there is growing recognition of the importance of clinical leadership in driving healthcare improvements (Jonas et al, 2011; West et al, 2015). Clinical leadership involves influencing and inspiring others to achieve common goals, while drawing on clinical expertise, interpersonal skills and a deep understanding of the healthcare system (Jonas et al, 2011).
While doctors and nurses have traditionally held leadership roles within the NHS, there is increasing acknowledgement of the potential for other health professionals, such as paramedics, to contribute to leadership at different levels and in various settings (Hou et al, 2013; Finn et al, 2013).
Paramedics possess unique clinical expertise, decision-making skills and adaptability, honed through their experiences in challenging, dynamic environments (Clompus and Albarran, 2016). These attributes make them well suited for leadership roles, particularly as the NHS shifts towards integrated care and community-based services (Finn et al, 2013; Wankhade, 2016).
However, research on paramedics as healthcare leaders remains limited, and recent studies have highlighted ongoing problems. For instance, Mausz et al (2023) found that women, despite comprising 40% of the active-duty paramedic workforce and having higher rates of university education, were nearly 70% less likely to hold leadership positions than men in a Canadian paramedic service.

This article aims to address this gap in the literature by critically analysing the potential of paramedics to be healthcare leaders within the NHS. By examining recent literature, leadership theories and case studies, it will highlight the key attributes that make paramedics suitable for leadership roles and discuss the potential benefits of increasing their involvement in healthcare leadership. Additionally, it will explore the challenges and opportunities around promoting paramedics into leadership positions and make recommendations for nurturing their leadership potential within the NHS.
Leadership theory and paramedics
Various leadership theories can be applied to understand the potential of paramedics as effective healthcare leaders.
Transformational leadership, a prominent theory in the field, focuses on inspiring and motivating followers to achieve common goals by appealing to their values and emotions (Bass and Riggio, 2006). This theory emphasises the importance of having leaders who can create a shared vision, challenge existing assumptions and empower their followers to perform beyond expectations (Bass and Riggio, 2006).
Paramedics, who often work in high-pressure situations, are well positioned to employ transformational leadership techniques, inspiring their teams to embrace new protocols and technologies that improve patient care, even when additional training is required (Wankhade and Mackway-Jones, 2015; Clompus and Albarran, 2016). By communicating a clear vision and providing support and encouragement, the leader can foster a sense of purpose and motivation among their team members (Wankhade and Mackway-Jones, 2015).
Situational leadership theory, another prominent approach, emphasises the importance of adapting leadership styles to followers' needs and the situation's demands (Thompson and Vecchio, 2009). This theory suggests that effective leaders must be able to assess the readiness and ability of their followers and adjust their leadership style accordingly, with approaches ranging from directive to supportive (Thompson and Vecchio, 2009).
Paramedics, who often work in dynamic, unpredictable environments, must be able to assess complex situations quickly and adapt their leadership approach to ensure the best possible outcomes (Hou et al, 2013; Givati et al. 2018). Empathy, listening and empowerment are crucial skills for healthcare leaders. As frontline health professionals, paramedics are well positioned to understand their patients' and colleagues' needs and concerns.
Research by Leyenaar et al (2019) on community paramedicine highlights the broad range of assessments paramedics conduct, emphasising their unique position to understand and address patient needs. This patient-centred approach, combined with their ability to adapt to various situations, enhances paramedics' potential as effective leaders.
The ability to adapt leadership styles to different situations is particularly important for paramedic leaders. For instance, when managing a critical patient, a paramedic leader may need to employ a more directive leadership style, providing clear instructions and close supervision to ensure all team members work efficiently and effectively (Hou et al, 2013). In contrast, when coordinating with other health professionals to develop a patient care plan, the same paramedic leader might adopt a more collaborative approach, fostering open communication and shared decision-making (Clompus and Albarran, 2016). Adapting leadership styles to different situations is crucial for paramedic leaders, as it enables them to manage the complex challenges they face in their roles effectively (Hou et al, 2013).
Applying transformational and situational leadership theories to the work of paramedics highlights their potential to become influential leaders within the NHS and beyond. By leveraging their unique skills, experiences and adaptability, paramedic leaders can inspire and motivate their teams, drive improvements in patient care and contribute to developing a more resilient and responsive healthcare system (Hou et al, 2013).
While these leadership theories highlight the potential of paramedics as leaders, recent research has identified psychological factors that may limit leadership development. Kerkez and Öztürk (2023) found a negative correlation between intolerance of uncertainty and leadership orientation scores among paramedic students. This suggests that addressing psychological factors, such as anxiety and uncertainty, is crucial in developing effective paramedic leaders. Leadership development programmes for paramedics should therefore incorporate strategies to build resilience and help them cope with uncertainty in high-pressure situations.
Transferable skills and care delivery
Paramedics possess transferable skills essential for effective leadership in healthcare settings. Their clinical expertise and ability to make rapid, complex decisions in high-pressure situations (Hou et al, 2013) enable them to provide robust clinical leadership and improve patient care.
For example, a paramedic leader in an emergency department may use their clinical knowledge and decision-making skills to efficiently allocate resources and coordinate patient care, resulting in improved patient flow and reduced waiting times (O'Meara et al, 2016).
A literature review by Perona et al (2019) explored the factors influencing paramedic judgement, decision-making and cognitive processing. The authors highlighted the importance of these skills in ensuring patient safety and improving outcomes, emphasising the need for ongoing education and training to support paramedics in their critical decision-making roles.
Similarly, research by Givati et al (2018) explored the importance of paramedic communication skills in building trust and rapport with patients. Their qualitative study highlighted the role of professionalism and effective communication in shaping patient perceptions of paramedic care, emphasising the need for paramedics to develop strong interpersonal skills alongside their clinical expertise.
Moreover, paramedics' experience in managing critical situations and making swift decisions can be invaluable in leadership roles that require quick thinking and adaptability (Hou et al, 2013). This skill set can be particularly useful in crisis management situations, such as during the COVID-19 pandemic, where leaders must make rapid decisions based on evolving information to ensure the safety of patients and staff (Hou et al, 2013; Mercer et al, 2018).
In addition to their clinical expertise and decision-making skills, paramedics are skilled communicators, capable of interacting with patients, families and other health professionals effectively (Clompus and Albarran, 2016). This ability to build rapport, convey information clearly and collaborate with diverse stakeholders is crucial for successful leadership in the NHS, where effective communication and teamwork are essential for improving healthcare delivery (West et al, 2015). Paramedic leaders can leverage their communication skills to foster a culture of open dialogue, ensuring that all team members feel heard and valued, increasing job satisfaction and better patient outcomes (Clompus and Albarran, 2016).
Furthermore, paramedics' communication skills can be valuable in leadership roles that involve engaging with patients and communities. For instance, a paramedic leader spearheading a community health initiative may use their ability to build trust and rapport to educate and empower patients to take control of their health, leading to better health outcomes and lower healthcare costs.
These attributes are vital for healthcare leaders, enabling them to support and motivate their teams, foster a positive organisational culture, and maintain their wellbeing in challenging circumstances (West et al, 2014). Paramedic leaders who display empathy and emotional intelligence can create a supportive work environment that encourages open communication, collaboration and innovation (Clompus and Albarran, 2016).
Moreover, the resilience demonstrated by paramedics in their daily work can be a valuable asset in leadership roles, where the ability to adapt to change, overcome obstacles and maintain a positive outlook is essential (Hou et al, 2013). Paramedic leaders who model resilience can inspire their teams to persevere through difficult situations and maintain high standards of patient care, even in the face of adversity (Clompus and Albarran, 2016).
The transferable skills paramedics possess, including decision-making, communication, emotional intelligence, empathy and resilience, alongside their clinical expertise, are highly relevant to leadership roles within the NHS and the broader healthcare sector. By leveraging these skills, paramedic leaders can drive improvements in patient care, foster positive work environments and contribute to developing a more resilient and effective healthcare system (Hou et al, 2013).
Case studies and examples
There are numerous examples of paramedics successfully transitioning into leadership roles within the NHS and the broader healthcare sector. These case studies demonstrate the positive impact that paramedic leaders can have on patient care, organisational performance and healthcare innovation.
Admission prevention
One notable example highlights the potential for paramedics to lead initiatives that help reduce hospital readmissions and improve patient outcomes.
In a study by Abrashkin et al (2016), a community paramedic programme was developed to provide acute care at home for patients with advanced illness. This involved a team of paramedics trained to provide in-home care to patients with long-term conditions. Over a period of 12 months, the programme resulted in a 50% reduction in hospital admissions and a 90% patient satisfaction rate. This success highlights the potential for paramedics to lead initiatives that improve patient outcomes and reduce healthcare costs. By leveraging their clinical expertise and collaborating with other healthcare providers, community paramedics were able to reduce hospital readmissions and enhance patient care. This initiative demonstrates the value of paramedic leadership in driving innovative, patient-centred care models that can improve health outcomes and reduce healthcare costs (Abrashkin et al, 2016).
Another example is that of a paramedic leader who was crucial in successfully implementing a new electronic patient record system across an NHS ambulance trust (O'Meara et al, 2016). Drawing on their frontline experience and understanding of the challenges faced by paramedics, this leader effectively communicated the new system's benefits, provided training and support to staff, and worked collaboratively with IT professionals to ensure a smooth transition. As a result, the trust saw improvements in data quality, patient safety and operational efficiency (O'Meara et al, 2016).
These case studies provide compelling evidence of the positive impact that paramedic leaders can have on healthcare organisations. By leveraging their unique skill set, clinical expertise and frontline experience, paramedic leaders can drive improvements in patient care, foster innovation and contribute to developing a more resilient and effective healthcare system (Hou et al, 2013; Thompson et al, 2015).
The potential for paramedics to take on leadership roles in healthcare is not limited to the UK. Globally, there is a growing recognition of the valuable skills and expertise that paramedics bring to healthcare organisations. In Australia, for example, the role of paramedics has been evolving to include a greater focus on leadership and management, with paramedics taking on key positions in healthcare administration and policy development (O'Meara et al, 2016).
Similarly, in Canada, paramedics are increasingly recognised as important members of the healthcare leadership team, with opportunities for advancement into management and executive roles (Tavares et al, 2016).
Primary care
In addition to leadership roles in emergency medical services, paramedics have demonstrated their potential to become leaders in primary care settings. The evolving role of paramedics in primary care has been recognised as offering a valuable opportunity to improve patient care and reduce the burden on GP practices (Eaton et al, 2018). As the NHS continues to face pressures to integrate care services and shift more care into the community, paramedics' leadership skills and expertise will become increasingly valuable in transforming primary care and ensuring the sustainability of the healthcare system.
Paramedics' unique skill sets, including their abilities to assess and manage acute conditions, provide patient education and collaborate with other health professionals, position them well to take on leadership roles in primary care (Eaton et al, 2018). By leveraging these skills and working closely with GPs and other primary care team members, paramedic leaders can contribute to developing and implementing innovative care models that improve patient outcomes, increase access to care, and optimise resource use.
Policy
The influence of paramedics on healthcare extends beyond leadership roles in clinical settings. Paramedics have also shaped healthcare policies and guidelines, contributing their expertise to developing evidence-based practices. For example, paramedics played a significant role in developing the UK's National Institute for Health and Care Excellence (NICE) (2016) guidelines on assessing and managing suspected sepsis.
Sepsis is a life-threatening condition that requires early recognition and prompt treatment. Paramedics are often the first health professionals to assess and treat patients with suspected sepsis, making their input invaluable in developing effective guidelines. The involvement of paramedics in the NICE guideline development process ensured that the recommendations were practical, feasible and relevant to the prehospital setting (NICE, 2016).
The contribution of paramedics to the NICE (2016) sepsis guideline highlights their growing influence on healthcare policy and their ability to shape clinical practice at a national level. By bringing their frontline experience and clinical expertise to policymaking, paramedics can help to ensure that guidelines and policies are evidence-based, patient-centred and reflect the challenges faced by health professionals in real-world settings.
Areas for improvement
While these case studies demonstrate the positive impact of paramedics in leadership roles, recent research has identified areas for improvement in paramedic education.
Kerkez and Öztürk (2023) found that paramedic students had low levels of knowledge about crime scene management, a critical skill for effective leadership in emergency situations. This finding indicates a need for more focused training on incident scene management within paramedic education programmes. Enhancing these skills could significantly improve paramedics' leadership capabilities in complex emergency situations and contribute to better patient outcomes.
Role evolution
As paramedics' roles continue to evolve and expand, their involvement in shaping healthcare policies and guidelines will likely become increasingly important. By leveraging their unique perspectives and skills, paramedics can contribute to developing more effective, efficient and responsive healthcare systems that meet the needs of patients and communities (Finn et al, 2013).
As the NHS continues to face significant pressures, including an ageing population, increasing demand for services and financial constraints, the need for strong clinical leadership has never been greater (NHS, 2019). By recognising and nurturing the leadership potential of paramedics, the NHS can tap into a valuable resource for driving improvements in patient care, organisational performance and healthcare innovation (Hou et al, 2013).
Challenges and opportunities
Despite the potential benefits of paramedics as healthcare leaders, there are some problems to be addressed.
Historically, leadership roles in the NHS have been dominated by other health professionals, such as doctors and nurses (Timmins, 2015). This professional hierarchy can create barriers for paramedics seeking to transition into leadership positions, as they may face resistance or scepticism from established power structures (Hou et al, 2013).
Additionally, paramedics may lack access to formal leadership training opportunities, hindering their ability to develop the necessary skills and knowledge to succeed in leadership roles (Hou et al, 2013; Wankhade and Mackway-Jones, 2015).
To overcome these barriers, the NHS must actively promote a culture of interprofessional collaboration and inclusivity (West et al, 2015; Reeves et al, 2017). This can be achieved by implementing interprofessional education and training programmes that foster understanding and respect among health professionals (Reeves et al, 2017). By breaking down silos and encouraging cross-disciplinary collaboration, the NHS can create a more supportive environment in which paramedic leaders can thrive (Hou et al, 2013).
Additionally, the NHS can support the development of paramedic leaders by investing in targeted leadership training and mentorship programmes (Hou et al, 2013). Such initiatives should equip paramedics with the necessary skills and knowledge to succeed in leadership roles while providing ongoing support and guidance as they navigate the challenges of healthcare management (Hou et al, 2013).
Bowles et al (2017) emphasised the importance of empowering paramedics to lead in their study on the four dimensions of paramedic practice in Canada. They argued that leadership and professional development are essential components of paramedic practice and that healthcare organisations should support paramedics in developing their leadership skills. Organisations can foster a culture of innovation and continuous improvement by providing opportunities for paramedics to take on leadership roles and engaging them in decision-making processes (Bowles et al, 2017). This may require changes to recruitment and promotion practices and the development of interprofessional education and collaboration opportunities (Hou and Rego, 2013).
An example of such an initiative is the NHS Leadership Academy's (2024) range of leadership development programmes, which provide structured development opportunities for health professionals, including paramedics, to enhance their leadership skills and gain exposure to strategic decision-making (NHS Leadership Academy, 2024). By participating in programmes like this, paramedics can build the confidence and competencies needed to take on leadership roles within the NHS (Hou et al, 2013; Bowles et al, 2017).
Moreover, paramedic leaders' unique perspectives and experiences can benefit the NHS. As frontline professionals, paramedics deeply understand the challenges patients and staff face and can provide valuable insights into improving service delivery and patient outcomes (Hou et al, 2013). By embracing paramedic leaders and creating opportunities to contribute to decision-making processes, the NHS can foster a more diverse and representative leadership team that is better equipped to tackle the healthcare system's complex challenges (West et al. 2015).
However, recent studies have identified specific problems in developing paramedic leaders. Mausz et al (2023) found women were significantly underrepresented in paramedic leadership roles despite having comparable experience levels to men, highlighting potential gender biases or barriers in career progression. Additionally, Kerkez and Öztürk (2023) noted deficiencies in paramedic students' knowledge of critical skills such as incident scene management, suggesting gaps in educational programmes. These findings underscore the need for targeted interventions to promote diversity in leadership and enhance the practical skills necessary for effective paramedic leadership.
While this article argues for expanding paramedic leadership roles, it is important to acknowledge potential challenges. Some argue that paramedics lack the broader organisational experience necessary for high-level leadership positions (Wankhade and Mackway-Jones, 2015). Additionally, there might be concerns about paramedics' ability to effectively lead multidisciplinary teams beyond their traditional context (Hou et al, 2013). Conversely, O'Meara et al (2016) suggest that the unique frontline experience of paramedics can bring fresh perspectives to leadership, potentially leading to innovative solutions in healthcare delivery.
In summary, while there are barriers to be overcome in promoting paramedics as healthcare leaders, there are also significant opportunities for the NHS to benefit from their unique skills and perspectives.
Recommendations
Based on the review of relevant literature and the analysis presented in this article, the author proposes a new framework for developing paramedics as effective healthcare leaders within the NHS (Figure 1).
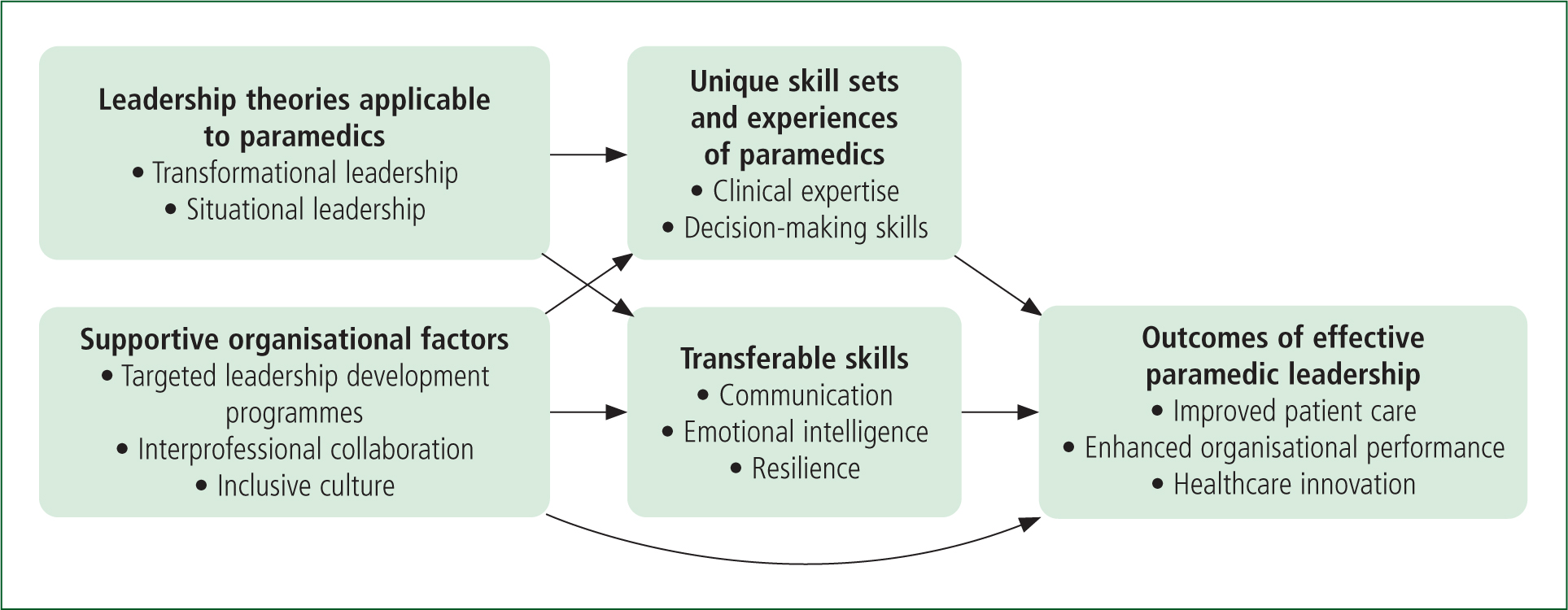
This original framework, developed specifically as part of this analysis, synthesises the key factors contributing to paramedic leadership development. It highlights paramedics' unique skill sets and experiences, their transferable skills, applicable leadership theories and the supportive organisational factors required to foster their leadership potential. By addressing these elements, healthcare organisations can create an environment that enables paramedics to become effective leaders, ultimately leading to improved patient care, enhanced organisational performance and healthcare innovation.
Several recommendations can be made to support the development of paramedic leaders within the NHS based on the evidence in this article.
Healthcare organisations should consider implementing targeted leadership development programmes for paramedics that include mentoring, coaching and formal education opportunities. These programmes can help paramedics acquire the skills and knowledge needed to succeed in leadership roles and foster a supportive environment for their growth and advancement.
Additionally, policymakers should prioritise the development of interprofessional collaboration frameworks and guidelines that promote the inclusion of paramedics in leadership roles. By recognising the value of paramedic leadership and creating opportunities for their involvement in decision-making processes, healthcare systems can benefit from their unique perspectives and expertise.
Based on recent research, the author would also recommend the following:
- Implementing targeted leadership development programmes and mentoring initiatives, particularly for women and other underrepresented groups in paramedicine, to address the leadership gap identified by Mausz et al (2023)
- Enhancing incident scene management and related leadership skills training in paramedic education curricula, addressing the knowledge gaps identified by Kerkez and Öztürk (2023)
- Incorporating strategies to build resilience and manage uncertainty into leadership development programmes, recognising the impact of psychological factors on leadership capabilities (Kerkez and Öztürk, 2023).
These additional recommendations aim to address specific issues identified in recent research and complement the broader strategies for developing paramedic leaders within the NHS.
Future research
Furthermore, research is needed to evaluate the impact of paramedic leadership on patient outcomes, healthcare costs and organisational performance. Such research could inform evidence-based strategies for supporting and advancing paramedic leaders and help build a stronger case for their inclusion in leadership positions across the healthcare sector, not just in prehospital care.
Future research should also focus on quantifying the impact of paramedic leadership on key healthcare metrics. This could include studies comparing patient outcomes, staff satisfaction, and operational efficiency in departments led by paramedics versus those led by professionals from other backgrounds. Such research would provide empirical evidence to support or challenge the arguments presented in this article about the unique value of paramedic leadership. Additionally, longitudinal studies tracking the career trajectories of paramedics who take on leadership roles could provide insights into the long-term impact of paramedic leadership on healthcare organisations and identify any specific support needs for these leaders as they progress in their careers.
Future research should also focus on:
- Empirical testing of the proposed framework for developing paramedic leaders
- Longitudinal studies tracking the career progression of paramedics who have undergone leadership training
- Comparative studies examining paramedic leadership across different healthcare systems internationally
- Investigation of the specific barriers faced by underrepresented groups in attaining leadership positions in paramedicine
- Evaluation of the impact of paramedic leaders on patient outcomes, staff satisfaction and organisational performance.
Such research would provide valuable insights into further developing and refining strategies for nurturing paramedic leaders in healthcare systems.
Limitations
The first limitation of this review is that the analysis is based primarily on literature from the UK and a limited number of other countries, so may not fully represent the global perspective on paramedic leadership. Second, the proposed framework for developing paramedic leaders has not been empirically tested.
Conclusion
Paramedics possess unique clinical expertise, decision-making skills and personal attributes that make them well suited for leadership roles within the NHS and the broader healthcare sector. The combination of their frontline experience, adaptability and ability to work effectively in high-pressure situations positions them as valuable assets in healthcare leadership.
Applying leadership theories such as transformational and situational leadership to paramedic practice shows these professionals have the potential to become influential leaders. Their transferable attributes, including clinical expertise, effective communication skills and resilience, are highly relevant to the complex challenges experienced by the NHS.
Case studies and examples from the UK and internationally demonstrate the positive impact that paramedics in leadership roles can have on patient care, organisational performance and healthcare innovation. However, problems remain, including historical professional hierarchies, a lack of formal leadership training opportunities and the underrepresentation of certain groups in leadership positions.
To harness the full potential of paramedic leaders, the NHS must invest in targeted leadership development programmes, foster a culture of interprofessional collaboration and create opportunities for paramedics to contribute to decision-making processes.
The proposed framework for developing paramedics as effective healthcare leaders provides a roadmap for addressing these issues and leveraging paramedics' unique strengths.
As the healthcare landscape continues to evolve, the role of paramedics as leaders will become increasingly important. By recognising and nurturing the leadership potential of paramedics, the NHS can create a more resilient, efficient and patient-centred healthcare system that is better equipped to meet future challenges.
Key Points
- Paramedics' clinical expertise, adaptability, empathy, emotional intelligence and skills in decision-making and communication make them well suited for healthcare leadership roles
- Transformational and situational leadership theories illustrate paramedics' potential to inspire and motivate teams, drive improvements in care and contribute to developing a more resilient and responsive healthcare system
- Paramedics' abilities are highly relevant to NHS leadership roles and can drive improvements in patient care, foster positive work environments and contribute to the development of a more effective healthcare system.
- Paramedic leaders can help reduce hospital readmissions, improve patient outcomes and implement new technologies and care models
- The NHS should invest in targeted leadership training and mentorship programmes for paramedics, foster a culture of interprofessional collaboration and create opportunities for paramedics to contribute to decision-making
CPD Reflection Questions
- What skills and attributes do you have that could contribute to your effectiveness as a leader in your organisation? What steps could you take at work to foster a culture of interprofessional collaboration and inclusivity, and how might this contribute to your personal and professional development as a leader?
- Consider a challenging situation you have faced in your professional life. How might applying transformational or situational leadership theories have helped you navigate that situation more effectively, and what lessons can you draw from this reflection?
- Consider an initiative or project you could undertake at work to drive improvements in patient care or service delivery, and consider how you might leverage your leadership skills to achieve this. Would you benefit from leadership development, and how would you access this?


