
There are approximately 60 000 out-of-hospital cardiac arrests in the UK each year (Ambulance Service Association, 2006) with survival rates of between 6% and 16% declared by the ambulance service NHS Trusts in the latest survival statistics (NHS England, 2015).
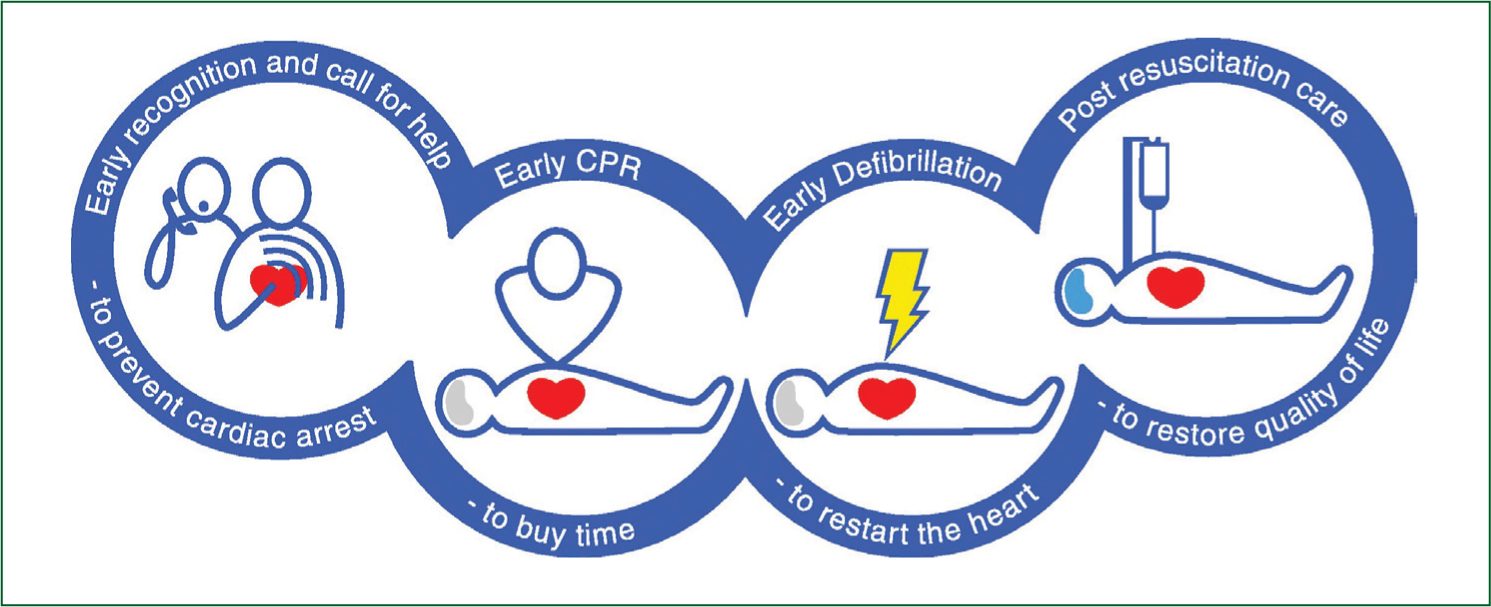
Evidence suggests survival rates could be improved with earlier identification and access to care for victims of out-of-hospital cardiac arrest. In 1988 Mary M. Newman of the Sudden Cardiac Arrest Foundation first described the ‘Chain of Survival,’ four interlinked interventions required to improve outcomes in out-of-hospital cardiac arrest. The chain relies on early identification, early cardio pulmonary resuscitation (CPR), early defibrillation and early advanced care (see Figure 1). This chain has been widely acknowledged and adopted by the bodies promoting resuscitation since that time and was incorporated into the International Liaison Committee on Resuscitation (ILCOR) guidance in 1997.
In spite of a free at point of delivery emergency medical service in the UK the survival rate from out-of-hospital cardiac arrest remains low compared to some areas such as Seattle in the USA where a programme of public education, awareness and accessible defibrillators has led to reported survival rates of around 56% in patients experiencing out-of-hospital cardiac arrest (King County Government, 2013). Current Government targets require UK ambulance Trusts to respond to the most serious life-threatening emergencies, categorised as Red 1, with a defibrillator in 8 minutes; however, survival rates from cardiac arrest deteriorate by approximately 10% for every minute post cardiac arrest. The challenge then is to get CPR and defibrillation to this vulnerable patient group in the quickest possible time. Due to the varied nature of the UK geography this can be extremely challenging for the traditional ambulance model of response, and several schemes have been introduced across the country to improve access to care for patients in cardiac arrest.
The two most common initiatives are community first responders (CFRs) and public access defibrillation (PAD) schemes. CFRs are volunteers living or working in communities who are trained in basic life support and automated external defibrillation, dispatched to life-threatening emergency calls in their locality to start treatment before the arrival of a conventional ambulance response. The implementation of PAD schemes involves mounting defibrillators in publicly accessible locations, commonly in rural communities, or areas of high public footfall like shopping centres, airports and railway stations. The CFR model was initially conceived as a benefit to rural communities, where response times were inevitably longer but many schemes have spread to urban areas with much higher population densities.
The benefits of early CPR and defibrillation together have been shown in studies to potentially increase the rates of survival significantly. Studies in the 1990s indicated that survival rates were best when CPR was started within 5 minutes of the heart stopping and defibrillation, for shockable rhythms, being delivered inside 10 minutes (Larsen et al, 1993; Valenzuela et al, 1997). Relying on traditional ambulance service response would make this unachievable in many cases.
While there is currently no national training syllabus for CFRs in the UK they are usually trained in the following key areas:
CFRs are commonly deployed to emergency calls falling into the following categories:
Schemes are normally made up of volunteers trained by the local ambulance service NHS Trusts although there are many variations, including partnerships with other emergency services such as the fire service, military-based groups and voluntary aid societies such as St John Ambulance (SJA) and British Red Cross. Living and working in the communities where they respond means that CFRs are able to reach patients far more quickly in many cases than the traditional ambulance resource that is dispatched at the same time. In recent data from the scheme run by one Ambulance Service NHS Trust in partnership with SJA, CFRs arrived at over 50% of calls that they were dispatched to before any other ambulance resource arrived on scene (internal management information, SJA).
While 80% of cardiac arrests occur in private dwellings, there are many instances of cardiac arrest in places where large numbers of people gather. There have been several schemes striving to increase the availability of defibrillators in the community, such as the ‘Shockingly Easy’ campaign being run currently by London Ambulance Service NHS Trust (London Ambulance Service NHS Trust, 2013), which aims to increase the number of public access defibrillators (PADs) in the London area by 1 000. Awareness of defibrillators and encouraging the use of them by members of the public is key to driving up survival rates in victims of cardiac arrest. Many sources have said that a defibrillator in a public building should be as common as a fire extinguisher, and that only by this level of normality will people think to look for them when they are needed.
But is there more that can be done? In the UK, only 43% of patients receive bystander CPR prior to arrival of the emergency medical service response. In Stavanger, Norway, this figure is 73%, and the average cardiac arrest survival figure is 25% (Lindner et al, 2011). There are many reasons cited for poor levels of bystander CPR and application of defibrillators:
Clearly there is more that can be done. While European Resuscitation Council guidance states that no specific training is necessary to use an AED, in a recent survey conducted by SJA 71% of people said that they would not be comfortable using an AED on someone suffering a sudden cardiac arrest, and only 43% of people who had been trained in some way in first aid would have confidence to carry out the skills they had learned in an emergency situation (SJA, 2014).
From this it is evident that more needs to be done, not only to bring defibrillators closer to more people in more places, through public access defibrillator and community first responding schemes, but we need to raise awareness of CPR and defibrillation in the wider community. Equipping many more people with the basic skills to save a life and the confidence to use these in the event of a sudden cardiac arrest are essential to reinforcing the Chain of Survival for patients suffering out-of-hospital cardiac arrest, and in turn, increasing the number of patients who survive it, as has been seen in the examples in Norway and the USA, ensuring that all the links are in place and as strong as possible in the critical moments when they are needed.

