It is estimated that 900 000 people in the UK have heart failure (Petersen et al. 2002) and it is a condition frequently encountered by
paramedics. Heart failure (HF) can be defined as:
‘A complex syndrome that can result from any structural or functional cardiac disorder that impairs the ability of the heart to function as a pump to support a physiological circulation. The syndrome of heart failure is characterised by symptoms such as breathlessness and fatigue, and signs such as fluid retention’
While these symptoms exist in varying degrees in the chronic progression of the disease, HF can present in an acute presentation known as acute heart failure (AHF). HF may precede AHF, however it is the rapid onset of signs and symptoms secondary to abnormal cardiac function that is unique to AHF. AHF is the most frequent cause of urgent consultation in patients with heart disease (Gheorghiade et al, 2005), but the presentation is further confused, as it may occur with or without previous cardiac disease (Ursella et al, 2007).
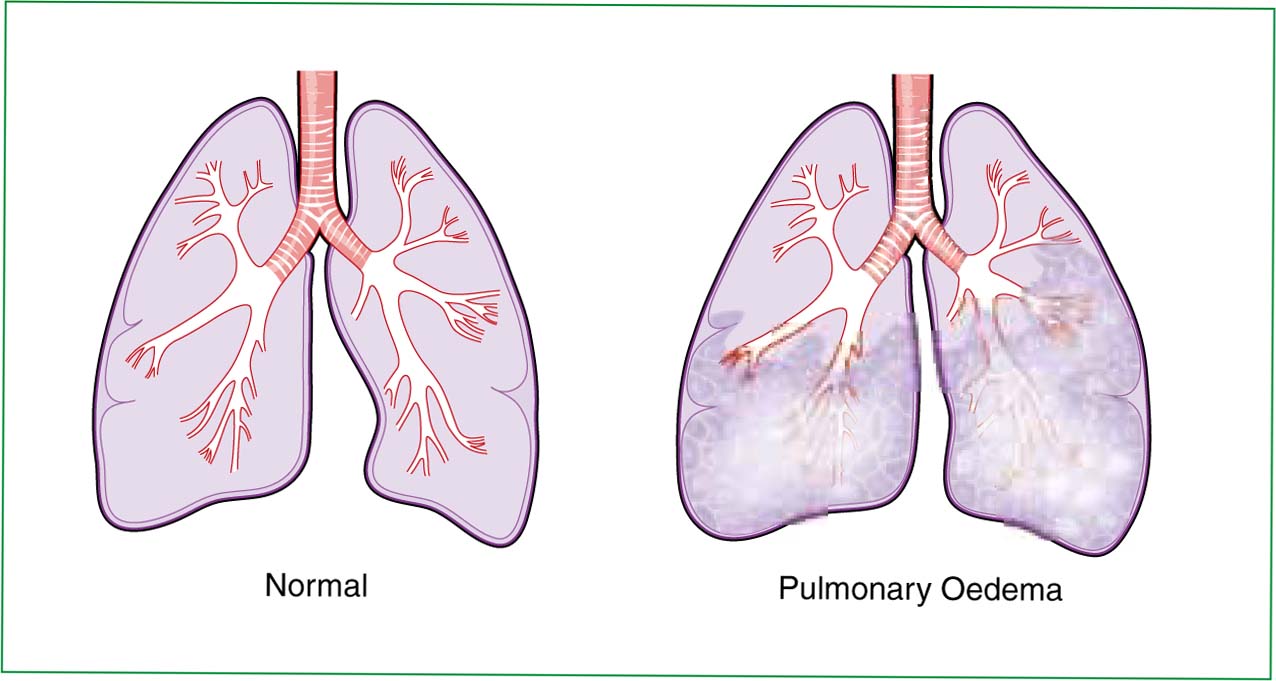
To the paramedic, it is the pathogenesis of AFH that has most lethal implications. As AHF develops, increased back pressure on the pulmonary circulation creates congestion of the pulmonary veins, resulting in increased pulmonary capillary pressure, precipitating leakage of fluid into the alveoli, thus creating a state known as acute cardiogenic pulmonary oedema (ACPO) (Dickstein et al, 2008; Saconta et al, 2008).
When this sequence of events presents in an emergency, the paramedic is confronted with a potentially life threatened, unstable patient. Figure 2 presents key features of the clinical history and presentation of heart failure.
The lethal nature of AHF is reflected in the one year and in-hospital mortality rates associated with ACPO being 40% and 12%, respectively (Nieminen et al, 2005). ACPO is commonly the result of acute coronary syndromes (ACS), dilated cardiomyopathy, valvular insufficiency, acute arrhythmias, and severe aortic stenosis (Gibelin, 2002; Nieminen et al, 2005). The paramedic may need to be aware of the underlying cause, and potential for therapeutic interventions as in ACS or arrhythmias. However, as a quarter of all deaths from heart failure occur suddenly and out-of-hospital (Mehnta et al, 2008), and ACPO is one of the leading causes of respiratory distress in cardiac patients (Saconta et al, 2008), in AHF it is the recognition of ACPO, and appropriate management that is paramount.
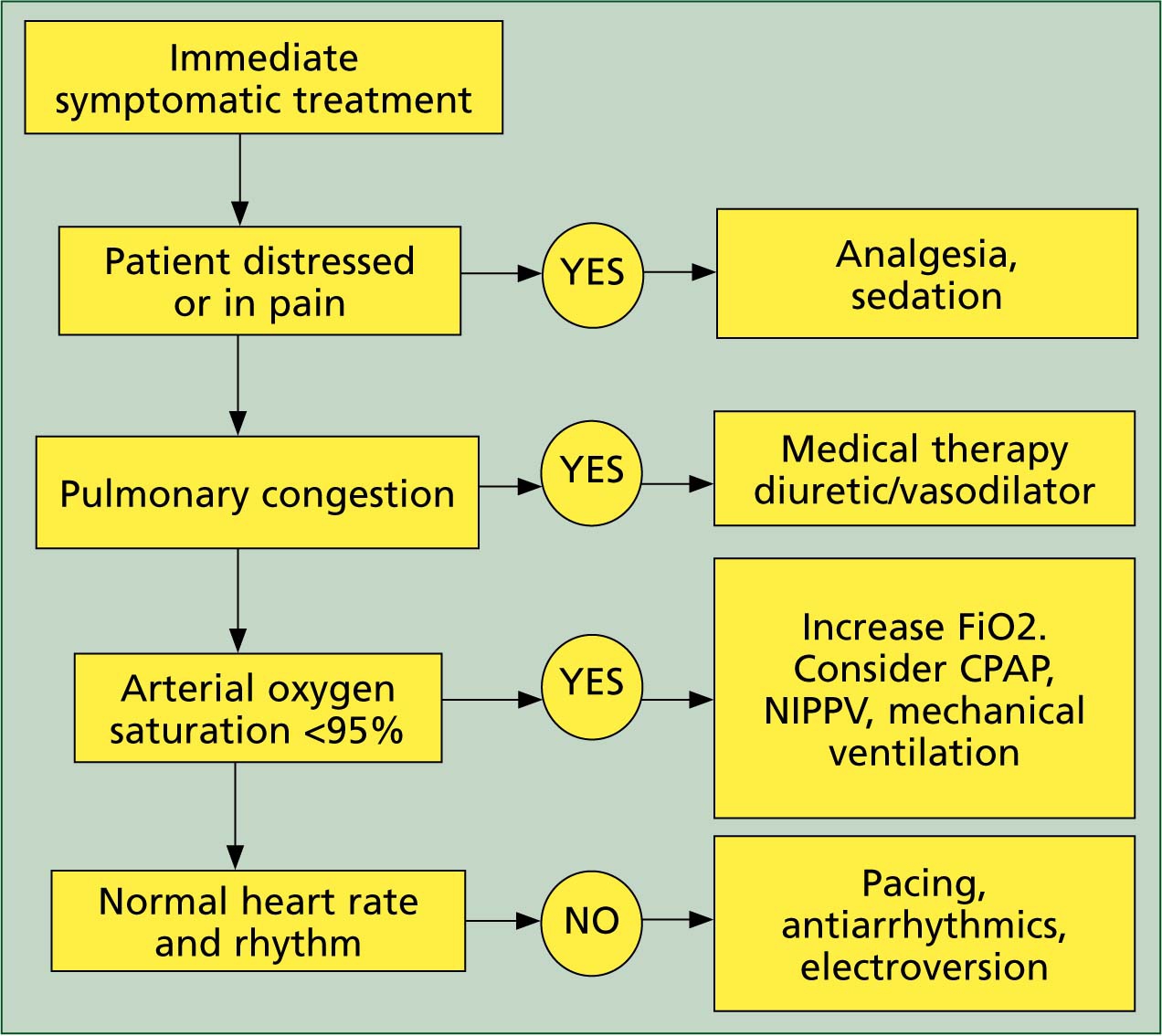
Current UK paramedic guidelines for the management of ACPO published by the Joint Royal Colleges Ambulance Liaison Committee (JRCALC, 2006) advocate administration of high concentration oxygen, assisting ventilation, furosemide, bucal blyceryl trinitrate and salbutamol.
However, there are occasions when this standard treatment may not be sufficient to reduce respiratory distress, and in this instance ventilation support should be initiated rapidly (Ursella, 2007). The in-hospital goals in managing AHF are based on immediate, intermediate and long–term actions. The immediate management maximizes use of medical therapy in line with JRCALC, however the European Society of Cardiology (ESC 2008) recommends vasodilators such as intravenous nitroglycerine at an early stage for AHF in patients without symptomatic hypotension.
Despite questioning the role of non invasive ventilation (NIV), the European Society of Cardiology (ESC, 2008) recommends its use, with the aim of improving symptoms, restoring oxygenation and improving organ perfusion. Subsequently, many clinicians are shifting towards the use of NIV.
Continuous pulmonary airway pressure (CPAP), is a form of NIV—it provides adjunctive airway support in lieu of endotracheal intubation (ETI).
It is pressure controlled ventilation that allows unrestricted spontaneous breathing any time in the ventilatory cycle. CPAP is delivered by a mask that completely covers the face, inclusive of the nose, providing expiratory support, allowing temporary oxygenation and ventilation for respiratory distress (Talman et al, 2008). In-hospital studies have shown improved outcome in patients with ACPO and reductions in the need to ETI (Masip et al, 2005; Peter et al. 2006; Saconato, 2008). Recognizing its value in treating ACPO, JRCALC (2006) advocate its adoption into prehospital practice.
Methods
A comprehensive English language literature search of MEDLINE and CINAHL from 2000 to November 2010 was conducted using a broad search strategy. The subject heading ‘CPAP’ was used including the sub headings of: ‘pulmonary oedema’, ‘pulmonary edema’ ‘ACPO’, ‘heart failure’ ‘pre hospital’ and ‘paramedic’ as key words. A second search was conducted using ‘non invasive ventilation’ as a subject heading along with the all subheadings above. The author decided a priori that randomized control trials, met analysis and systematic review on in hospital CPAP would be deemed eligible.
Case reports, letters, editorials and comments in addition to quantitative studies with a surveillance sample size of less than 25 were excluded. In hospital studies were limited to 10 for review. Review articles that contained no original data were ultimately omitted, but their bibliographies were hand searched. Given relative scarcity in prehospital care literature, all articles regarding miscellaneous topics such as cost, compliance, psychosocial aspects and quality of life were selected for review. These were manually scanned for relevance and eligibility. The search yield is shown in Table 3.
During study review, a database was constructed that documented each paper's first author, year of publication, setting, clinician, method sample size, inclusions, exclusions, outcome measures and results. A total of 52 articles were selected as relevant and eligible for review. Figure 4 summarizes the selection of in hospital papers. A final limit of ten articles was set due to the limitations of a single author review.
CPAP
CPAP does not seek to replace ETI—rather it provides adjunctive airway support in lieu of ETI. The in-hospital literature presents mixed results in improvements in physiological parameters, reduction in risks of pneumonia and need to ETI following application of CPAP when compared with conventional therapy (Crane et al, 2004; Hess, 2005; Masip et al, 2005; Peter et al. 2006). Therefore, careful critique is needed prior to transferring these results into the prehospital setting.
For instance, need to ETI may well be a poor outcome measure in favour of survival, as patients requiring ETI are unstable, critically ill, patients with poor physiological reserves, near to total respiratory failure thus presenting limitations for optimisation of ETI (Matioc, 2005). Wink (2006) identified 790 articles studying CPAP, a 22% absolute risk reduction in the need for ETI (95% confidence interval -34% to -10%) and 13% in mortality (95%CI, -22% to -5%) was shown. However, the mortality rate in the control groups had a wide range (from 0% to 64%), indicating large differences in severity of illness between studies. When studying ACPO and CPAP, controlling for such variance in severity of illness and also differences in the ventilation devices presents a potential threat to the validity of such studies.
Saconato (2008) included 21 studies involving 1071 participants in their systematic Cochran review comparing standard medical care and CPAP in patients with ACPO. Their results suggest that CPAP reduces hospital mortality (RR 0.58, 95% CI 0.38 to 0.88) and need for ETI (RR 0.46, 95% CI 0.32 to 0.65) when compared to standard care. Once again, standard medical care varied widely among the studies, Saconato cites a study which used high doses of Isosorbide Dinitrate, which related to better results in need for ETI. Other potential sources of bias may have been the different thresholds used for ETI.
Based on such results, CPAP has become increasingly used in the treatment of ACPO. As indicated earlier, the ESC (2008) guidelines recognize its in-hospital value, and the potential prehospital use is advocated by JRCALC (2006). JRCALC propose its use when standard treatment is not sufficient to reduce respiratory distress. They cite three in- hospital CPAP studies (Crane et al, 2004; Park et al, 2004; L'her et al, 2004) upon which they conclude that CPAP is feasible in the prehospital setting. However, these studies are dated and there are also methodological limitations with their designs.
Crane et al (2004) randomly assigned sixty patients presenting with ACPO to conventional oxygen therapy, CPAP, or Bilevel ventilation. Expected rises in oxygen saturation did not emerge, in fact they were significantly lower in the CPAP group compared with controls at 10 min (p=0.02) and 30 min (p=0.03). Fourteen (70%) of the control group survived to hospital discharge, compared with 20 (100%) in the CPAP group (p=0.029). In the same study, Crane reported that patients who survived to hospital discharge were given higher Nitrate doses (5.9 mgs vs 4.1 mg; p=0.042), and were more likely to have been given sub-lingual nitrates by ambulance personnel (53% vs 9%; p=0.016). Therefore, one could argue that it is the early administration of nitrates rather than CPAP that is effective in managing ACPO.
Comparing a well balanced group with no significant differences in medical interventions, Park et al (2004) sought to study the effects of oxygen vs CPAP, on the rate of ETI in patients with ACPO through randomized control trial. 11 of 26 patients (42%) received ETI in the oxygen group (p.001). Whilst this study seems to suggest that CPAP significantly averts the need to ETI, no significant differences were reported in mortality to hospital discharge (p<0.61).
The physiological effects and the clinical efficacy of CPAP vs standard medical treatment in ACPO were compared by L'her (2004). At 1 hour, patients assigned to CPAP exhibited a higher PaO2 than those assigned to standard treatment (p<0.00). The study was suspended at 48-h because mortality was significantly lower in the CPAP group (7 vs 24%; p=0.0017), leading to claims that CPAP improves the early 48-h survival rate.
On examining the characteristics of both groups, the oxygen group had a higher incidence of respiratory tract infection 19 (41) vs 11 (26) in CPAP. As the study concerns ACPO, these should not have been included in the study. The groups were also unbalanced, using the New York classifications of heart disease, with 7 of the oxygen group vs 16 in the CPAP group (p=0.02) presenting in class I-IV.
The New York Heart Association classification of HF grades the functional class symptoms prior to the onset of an acute episode, with class IV being most severe (NYHA 1994). The CPAP group were therefore recognised as having an inferior cardiac function to that of the oxygen group.
As this was an un-blinded trial, it could be argued that the recognition of ACPO secondary to heart failure may have influenced the decision to instigate CPAP, and the effects of CPAP may be more to do with their beneficial effects on ACPO versus respiratory tract infection. Since publication of these studies, Gray et al (2009) published the results of the 3cpo trial, the largest UK–based study into CPAP. They conducted a multicentre open prospective RCT of patients presenting with severe ACPO in 26 emergency departments in the UK. Patients were randomized to standard oxygen therapy, CPAP or NIPPV on a 1:1:1 basis for a minimum of 2 hours. 1069 patients were recruited to standard therapy, CPAP or NIPPV. They found no difference in 7-day mortality for standard oxygen therapy (9.8%) and non-invasive ventilation (9.5%; p=0.87).
The combined end point of 7-day death and intubation rate was similar, irrespective of type of NIV (CPAP 11.7% vs NIPPV 11.1%; p=0.81). Compared with standard therapy, NIV was associated with greater reductions in breathlessness (visual analogue scale score 0.7, 0.2–1.3; p=0.008) and heart rate (4/min, 1–6; p=0.004) and improvement in acidosis (pH 0.03, 0.02–0.04; p<0.001) and hypercapnia (0.7 kPa, 0.4–0.9; p<0.001) at 1 hour. They concluded that noninvasive ventilatory support safely provides earlier improvement and resolution of breathlessness, respiratory distress and metabolic abnormality.
However, this does not translate into improved short or longer-term survival. They recommend that CPAP or NIPPV should be considered as adjunctive therapy in patients with severe ACPO in the presence of severe respiratory distress or when there is a failure to improve with pharmacological therapy.
Whilst there is evidence pointing to potential benefits of in-hospital CPAP, the 3Cpo trial robustly reveals that although improvements on physiological parameters can be demonstrated, increased survival does not naturally follow. Despite this, one cannot be sure that earlier application in the prehospital environment will yield similar results.
Factors such as transport pressures, diagnostic uncertainty, equipment failures, and limited clinical expertise, may limit its use. Conversely, the palliative effects on relief of breathlessness, earlier intervention on physiological variables and reducing the need to ETI may present opportunities distinct to the prehospital environment.
Conclusion
ACPO, secondary to AHF, is a common presentation to paramedics and has many lifestyle, genetic medical and environmental factors influencing its aetiology. However, the pathogenesis of AHF leading to ACPO, when recognized, offers scope for paramedic intervention to reduce the spiral of deteriorating respiratory and cardiac function. Adherence to current JRCALC guidelines offers optimum management of ACPO, and the literature reviewed highlights the importance of use of nitrates, with the optimum delivery being intravenous.
When medical intervention has been exhausted, application of CPAP is recommended. These recommendations are based on studies showing improved physiological variables, reduced need to ETI, and palliation of breathlessness. However, when studying CPAP, confounding factors limit the ability to attribute observed benefits to its application. Variance in the standard of medical treatments, co interventions such as use of nitrates, and severity of illness between groups all need controlling for in order to attribute such benefits to CPAP. A more recent well designed UK-based study found similar improvements in physiological variables and palliation of breathlessness, but failed to transfer such improvements into improved survival.
The prehospital phase of care may present opportunities for the use of CPAP unique to the environment. It would offer a non-invasive means of supporting ventilation prior to ETI, palliation of breathlessness may reduce distress associated with emergency presentation, and earlier restitution of physiological variables could ultimately lead to improved mortality. Prior to any such moves, consideration should be given to adherence and maximisation of current medical therapy within JRCALC, and future potential for use of intravenous nitrates.
