English ambulance services resuscitate 28 000 people in out-of-hospital cardiac arrest (OHCA) each year using evidenced-based algorithms in the Resuscitation Council UK's (RCUK) advanced life support (ALS) guidelines (Soar et al, 2021). The majority are adults who arrest from issues of cardiogenic origin (El-Sherif et al, 2010). Around 8% survive to discharge following early recognition of a defibrillatable or shockable ventricular rhythm and early defibrillation within the chain of survival (Soar et al, 2021). In OHCA, 23% of arrests in people aged <65 years have an initial shockable rhythm across all responder types (Nadolny et al, 2018).
Aetiology, bystander cardiopulmonary resuscitation (CPR), time to first defibrillation (TTFD) and presenting rhythm are all variables within an Utstein-based model that gives prognostic relevance of the factors that improve survival outcomes (Baldi et al, 2020). When using this Utstein-based model, 17.4% of patients have a shockable rhythm and one-third of paramedic defibrillations result in event survival (Baldi et al, 2020).
Cardiac arrest outcomes improve with early defibrillation of a shockable rhythm and survival chances diminish by 10% for every minute defibrillation is delayed (Jost et al, 2010; Soar et al, 2021). Despite its significance, TTFD is not a measured outcome within the Out of Hospital Cardiac Arrest Outcomes Registry (OHCAOR, 2018). The lack of research around the influence on TTFD on outcomes may help to explain this data absence.
The European Resuscitation Council (ERC) Guidelines state that paramedics traditionally perform autonomous manual defibrillation (MD) after visual confirmation of ventricular fibrillation (VF) or pulseless (absence of palpable pulse) ventricular tachycardia (PVT) (Soar et al, 2015).
Semi-automatic external defibrillator (SAED) devices use algorithm-based technology to analyse the rhythm and voice prompt the operator to defibrillate VF/PVT (Parry and Higginson, 2013). In-hospital research advocates the use of MD as SAED has longer time frames for analysis and more CPR interruptions, which can reduce survival outcomes (Lang and Ang, 2012).
Since 2015, new technologies have improved both strategies. Audio-visual feedback (AVF) ancillaries have improved the quality of CPR, improving outcomes using both MD and SAED strategies (Miller et al, 2020). The SAED arrhythmia-detecting algorithms have standardised sensitivity/specificity and can now detect VF/PVT with an accuracy of 99% and 75% respectively (Nishiyama et al, 2015; Badnjević et al, 2019). Analysis through CPR (ATC) technologies can offer 70.5% accuracy, with 93.6% sensitivity and 99.5% specificity for VF/PVT (Hu et al, 2019).
It is now pertinent to critically analyse which defibrillation strategy offers better TTFD outcomes, given the ORBIT trial findings, which showed that reducing TTFD increases survival (Morrison et al, 2005). It is worth considering the potential therapeutic influence of AVF and ATC within the same critical analysis.
Guidelines today support the use of biphasic defibrillation (BD) technologies after the ORBIT trial found BD has superior efficacy while reducing myocardium damage, giving ethical justification for BD's use (Morrison et al, 2005; Soar et al, 2021). The biphasic shock completely depolarises the heart, allowing functioning pacemaker cells to reinstate the rhythm (Vaswani et al, 2016). BD technology is available to both MD and SAED devices (Hatlestad, 2004).
Hanisch et al (2020) identified that MD delays meant TTFD was 8 seconds—3 seconds longer than the ERC recommendations to maintain perfusion—and is responsible for more inappropriate shocks. This pattern is evident in other studies (Cheskes et al, 2015). Ruiz de Gauna et al (2014) revealed that SAED sensitivity for detecting shockable rhythms can be reduced by artefact to as low as 58.4%.
There is quantitative research on in-hospital comparisons of MD versus SAED examining TTFD (Soar et al, 2015). In-hospital cardiac arrests occur close to defibrillation devices in well-lit areas, with ALS-trained staff nearby, so in-hospital studies cannot be compared to OHCA TTFD outcomes (Keebler et al, 2017). Randomised controlled trials and systematic reviews for OHCA have proved that a defined period of CPR before defibrillation does not improve the presence of a shockable rhythm or survival outcomes, and that altering guidelines or using different SAED technologies can shorten the pauses in CPR (Jost et al, 2010).
These studies have helped to improve defibrillation but have not directly reviewed which strategy is superior for TTFD outcomes for OHCA attended by paramedics.
Aims
This systematic review aims to conclude whether MD or SAED (control or intervention) is the superior strategy for paramedics in TTFD outcomes. The review identified quantitative comparison (head-to-head) studies where both BD strategies (control/intervention) have been employed in adult, non-traumatic OHCA or simulated adult, non-traumatic OHCA attended by paramedics.
TTFD was defined as the time from paramedic arrival to the first defibrillation (seconds/minutes) (Cheskes et al, 2011).
Methodology
The approach followed was that set out in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al, 2009). No ethical approval was required for this systematic review and no protocol registration was necessary.
A scoping search of Google Scholar, CINAHL, Cochrane and Embase was conducted using the search terms: time to defibrillation in OHCA; and manual defibrillation versus semi-automatic defibrillation. The intention was to locate quantitative research with TTFD outcomes and to identify the relevant population, intervention, comparison and outcomes (PICO) search terms. Furthermore, this would yield a timeline of studies to build an understanding of the background literature and potential systematic review criteria for future comprehensive database searches.
Data sources
A comprehensive database search was then conducted to identify adult OHCA, comparing MD and SAED for TTFD outcomes.
Using the CINAHL/MEDLINE combined and Embase databases via EBSCOhost, the search terms in the PICO criteria (Table 1) were combined with the Boolean operator OR within their relevant PICO groups. All results were combined with AND, and all database results were recorded via screenshots and placed into results tables.
| Population: adult out-of-hospital cardiac arrest | Intervention: semi-automatic defibrillation | Comparison: manual/standard defibrillation | Outcomes: time, delays, speed and pauses |
|---|---|---|---|
| Resuscitation or CPR or cardiopulmonary resuscitation | SAED defibrillat* | ILS shock | Cardioversion time |
| Advanced life support paramedic | SAED shock | ALS shock | Defibrillation time |
| Advanced life support or ALS | Non manual defibrillat* | Standard cardioversion | Speed to defibrillat* |
| Idiopathic ventricular rhythm* | Non manual shock | Manual cardioversion | Speed to shock |
| Lethal ventricular rhythm* | Non-standard shock | Cardioversion | Reduce pre shock pause |
| Shockable rhythm | Non-standard defibrillation | Ambulance defibrillat* | Shock delays |
| VT | Semi-automatic shock | Ambulance service defibrillat* | Defibrillation delays |
| Pulseless ventricular tachycardia | Semi-automatic defibrillator | EMS defibrillat* | Faster shock |
| Pulseless VT | Automatic defibrillation | Paramedic defibrillat* | Faster defibrillat* |
| VF | Semi-automatic defibrillat* | ILS defibrillat* | Time to shock |
| Ventricular fibrillation arrest | SAED defibrillation | ALS defibrillat* | Time to deliver shock |
| Ventricular fibrillation or v-fib | AED defibrillation | Manual standard shock | time delay |
| EMS cardiac arrest | AED shock | Standard manual shock | Delays to shock |
| Pre-hospital cardiac arrest | Semi-automatic defibrillation | Manual shock | Delays to defibrillat* |
| Adult non traumatic cardiac arrest | SAED | Standard shock | pre defibrillation pause |
| Adult cardiac arrest | AED | Manual defibrillat* | pre-shock pause |
| OHCA or out of hospital cardiac arrest | Standard defibrillat* | Time to defib* | |
| Manual standard defibrillat* | Time to first shock | ||
| Standard manual defibrillat* | |||
| Standard manual defibrillation |
Following the application of inclusion and exclusion criteria (Table 2), only studies making a direct head-to-head comparison between SAED and MD were included to reduce confounding bias.
| Inclusion criteria | ||
|---|---|---|
| Type of study | Quantitative comparative studies, English language, after 2005 | |
| Population | Intervention/comparison | Outcomes |
| All adult out-of-hospital cardiac arrest | SAED versus manual comparison | Time |
| Non-traumatic | Biphasic | Speed |
| ALS paramedic qualified in attendance | Pauses or delays to first defibrillation results | |
| Exclusion criteria | ||
| Type of study | Qualitative studies and non-comparison studies. | |
| Population: | Intervention/comparator | Outcomes: |
| Before 2005 | Monophasic | No SAED versus manual comparison |
| Laypersons/BLS-trained person in attendance | Internal defibrillators | No time to first defibrillation results and/or outcomes |
| Non-shockable rhythms | Interventions before the first defibrillation | |
| Paediatric | ||
| In hospital | ||
Screening and appraisal methods
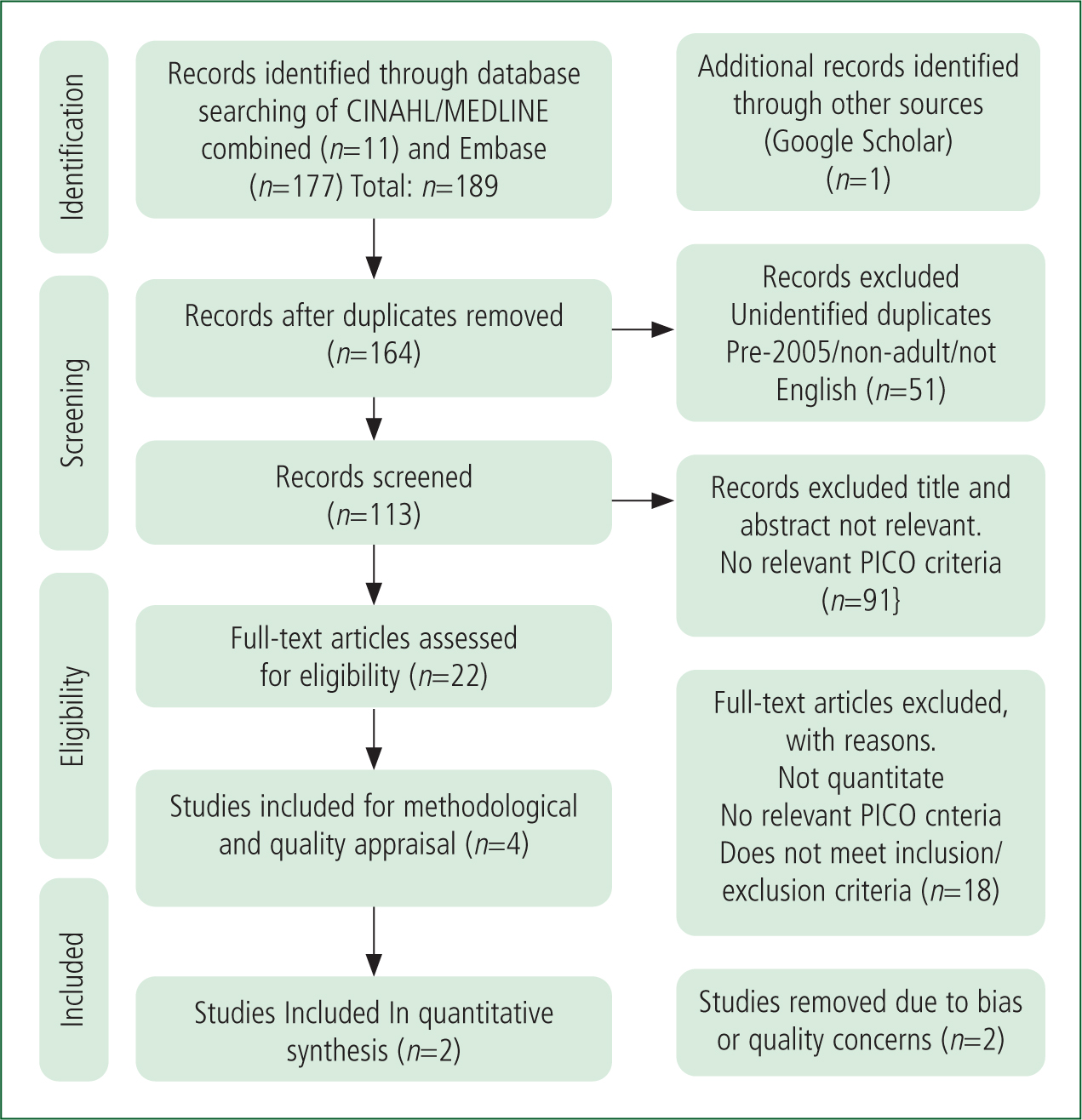
The scoping search located 69 papers, five of which made a quantitative MD versus SAED comparison without monophasic devices and had the required TTFD outcomes. The results of CINAHL/MEDLINE combined returned 11 papers with no duplicates, Embase returned 101 papers after duplicates had been removed. One paper that had not appeared in the database searches was added from the scoping search. A total of 113 papers remained from the first search of titles and abstracts. After titles and abstracts had been screened, 22 papers remained for the full-text screening after 91 were removed as they lacked relevant PICO terms or criteria.
After the second screening results of full-text papers, only four papers remained. Following methodological appraisal and quality appraisals, using the McMaster critical appraisal tool, two further studies were removed. One was Adams et al (2009), which included a monophasic device pertinent to the exclusion criteria. The other, Pytte et al (2007), reported a small sample size, no pilot study, no power analysis and no statistically significant results within the TTFD outcome (P<0.36). Two papers remained for data extraction and data synthesis: Nehme et al (2017); and Kramer-Johansen et al (2007).
These search results are shown in the PRISMA flow diagram (Figure 1); the two papers for inclusion were placed into a summary of characteristics table after appraisal (Table 3).
| Study number (quality score) | Author and year | Study type | Sample size | Meets all PICO | Meets criteria | Oxford levels of evidence* | Significant result |
|---|---|---|---|---|---|---|---|
| 76 (31/34) | Nehme et al (2017) | Time series analysis/quasi experimental | 14 776 | Yes | Yes | 1c | Yes |
| 113 (25/34) | Kramer-Johansen et al (2007) | Cohort study | 223 | Yes | Yes | 2b | Yes |
PICO: population, intervention, comparison and outcomes
Findings
Kramer-Johansen et al (2007) displayed a good study design with limited selection, detection, attrition and reporting bias. They found that MD was 7 seconds faster than SAED for mean TTFD in defibrillation attempts and noted that 50% of defibrillations delivered in the first 30 seconds resulted in a return of spontaneous circulation (ROSC). MD was responsible for 20% more inappropriate shocks.
Nehme et al (2017) reported, in a very robust study, 14 776 episodes of defibrillation, offering statistically significant results (P<0.001; CI 95%; narrow 95% CI reported). The article noted the SAED strategy offered a 10.3% improvement in mean TTFD in 2 minutes and a 68% odds improvement of receiving a shock within 2 minutes. The overall distribution of TTFD within 2 minutes improved from 40–75% to 60–90% when the biphasic SAED strategy was employed.
Nehme et al (2017) noted the likelihood of survival was reduced by 22% for every interruption greater than 5 seconds; the SAED was responsible for increased ‘hands-off time’ and provided no difference to PVT/VF conversion rates.
In conclusion, Nehme et al (2017) deemed MD to be the preferred strategy, despite SAED decreasing TTFD. This was rationalised as SAED led to a 26% reduction in survival. Accountability for these survival outcomes was placed on CPR delays, causing reduced perfusion during SAED rhythm analysis and charging.
Discussion
The studies discussed above investigated the effectiveness of different strategies for defibrillation in OHCA, specifically comparing MD and SAED. The primary outcome measure assessed in these studies was the TTFD, which is a critical factor in the survival of OHCA patients.
Kramer-Johansen et al (2007) found that MD was 7 seconds faster than SAED for mean TTFD in 160 defibrillation attempts. This was attributed to the SAED powering on time, rhythm analysis time and how long it took for the user to follow the verbal prompts.
They noted that 50% of defibrillations delivered in the first 30 seconds resulted in a ROSC, adding weight to the justification for use of MD and the clinical significance of its decreased TTFD in OHCA. However, MD was responsible for 20% more inappropriate shocks, which is consistent with other studies (Hanisch et al, 2020).
Nehme et al (2017) performed a robust study based on 14 776 episodes of defibrillation. This systematic review used only results of biphasic MD outcomes in TTFD from 2008. Nehme et al (2017) established that the biphasic SAED strategy offered a 10.3% improvement in mean TTFD within 2 minutes and a 68% odds improvement of receiving a shock in 2 minutes. Their study analysed results from 2012 to 2015, using more modern, faster and more accurate SAED technologies than those examined by Kramer-Johansen et al (2007). This is the most likely cause for the conflicting TTFD findings for the SAED devices.
Additionally, Nehme et al (2017) noted the odds of survival reduced by 22% for every interruption greater than 5 seconds, and that the SAED was responsible for increased hands-off time and provided no difference to PVT/VF conversion rates. In conclusion, this study deemed MD the preferred strategy, despite SAED decreasing TTFD. This was rationalised by the 26% reduction in the risk-adjusted odds of survival echoed by in-hospital studies and Kramer-Johansen et al (2007). Accountability for these survival outcomes was placed on CPR delays, causing reduced perfusion during SAED rhythm analysis and charging. These delays exceeded the recommended 5-second window in ALS guidelines (Soar et al, 2021). This highlights the need for better SAED technologies that can reduce delays and decrease the risk of inappropriate MD shocks associated with decreased survival outcomes
Nehme et al (2017) and Kramer-Johansen et al (2007), noted the cessation of CPR for rhythm analysis, the duration of analysis, the interpretation of the analysis and the decision to defibrillate affect TTFD outcomes. Within modern SAED equipment, these discrete actions are determined by the device itself (Kramer-Johansen et al, 2007; Israelsson et al, 2017; Nehme et al, 2017). Within MD, these actions are solely the result of autonomous human operation, involving skills that propagate from continued training, exposure and experience of OHCA (Kerle et al, 2019).
Despite training and experience, the survival to discharge rate after OHCA has remained at 8% in the UK for 10 years. Scandinavian nations have yielded greater survival outcomes considering their lower population density (OHCAOR, 2018). This suggests that more training is required to overcome human factors around leadership, skill, communication and competency of paramedics in MD, although this is not without logistical issues (Nehme et al, 2017; Kerle et al, 2019).
It is worth appreciating at this point that SAED algorithm analysis technologies have improved since the Nehme et al (2017) data collection in 2015. SAED devices now have better sensitivity, specificity and analysis speed and can charge in background during analysis. These advances could reduce the delays in both studies and decrease the risk of inappropriate MD shocks. The most up-to-date SAED devices have a sensitivity of 92.2% and a specificity of 95.9%. They can interpret a rhythm in 3 seconds, while simultaneously charging in the background. These new SAED devices could reduce the delays seen in both studies across SAED strategies (Israelsson et al, 2017; Zijlstra et al, 2017).
Furthermore, Kramer-Johansen et al (2007), acknowledged that MD is associated with 10% more inappropriate myocardium defibrillations than SAED, which could cause non-reversible cardiac tissue damage and result in unsalvageable OHCA episodes. Pytte et al (2007) and Hanisch et al (2020) also found inappropriate MD to affect survival outcomes. The SAED technologies that were historically associated with reduced survival have dramatically improved, reducing CPR delays, while their shock accuracy can alleviate the dilemma of unnecessary myocardium damage caused by inappropriate MD. Kramer-Johansen et al (2007) and Nehme et al (2017) state that SAED offers higher accuracy in rhythm interpretation. Zijlstra et al (2017) reinforce this conclusion, showing that some SAED devices have successfully interpreted 100% of the PVT/VFs in 135 attempts, in a fraction over 3 seconds.
Mader et al (2011), when reporting on OHCA outcomes, noted that converted initial shockable rhythms significantly improved survival chances compared to converted non-shockable rhythms. Survival diminishes by 10% with every minute that defibrillation is not available (Soar et al, 2015).
When this is considered with the data within the studies by both Nehme et al (2017) and Kramer-Johansen et al (2007), it demonstrates that decreasing TTFD to identify and accurately convert an initial shockable rhythm is imperative. If current guidelines remain, based on out-of-date and in-hospital research (Lang and Ang, 2012); Ruiz de Gauna et al, 2014; Soar et al, 2015), then useful therapeutic or diagnostic interventions compatible with MD are needed to help reduce human error.
New technologies offering AVF for CPR with perfusion indicators improve overall compression depths, rates, recoils and propagate increased perfusion leading to increased rates of survival (Miller et al, 2020). While these do not improve TTFD outcomes, they do offer MD a supporting substructure for OHCA that improves overall Utstein model-based outcomes for survival. AVF could help support the continued use of MD in line with Kramer-Johansen et al's (2007) and Nehme et al's (2017) conclusions. This could be deemed the cumulative incorporation that finally settles the debate.
This AVF technology, though, is already used in modern SAED devices, with the added option of built-in ATC technology, enabling the modern SAED device to analyse the rhythm during CPR with 70.5% accuracy (Israelsson et al, 2017; Hu et al, 2019). This ATC technology is available to some modern MD devices, presenting an option to further improve the supporting substructure of MD and retain MD for OHCA in line with the guidance (Soar et al, 2015).
These technological advances change the perspective of pre-2015 TTFD results of the included studies. They raise an important question as to whether the pre-shock delays, caused by the SAED devices of the past, is still enough justification to continue with MD, given that SAED reduces TTFD and inappropriate shocks (Kramer-Johansen et al, 2007; Nehme et al, 2017).
There is a lack of evidence directly comparing MD and SAED strategies for paramedic OHCA treatment and TTFD outcomes. This is a critical gap in research because a solution could be found to improve TTFD and, ultimately, improve survival outcomes. Further research is needed to investigate the potential benefits of using MD and/or SAED strategies in paramedic OHCA treatment.
If 23% of 28 000 OHCA have a shockable rhythm, and converted initial shockable rhythms produce improved survival outcomes (Soar et al, 2021), it is pertinent to state that decreasing the TTFD, as an Utstein model-based outcome, increases the chances of survival. Nehme et al (2017) found a biphasic SAED protocol employed by paramedics led to a 10.3% improvement in the TTFD within 2 minutes.
Previous concerns over SAED algorithm delays discussed by Kramer-Johansen et al (2007), need to be considered in the context of the pre-2015 devices. Modern SAED devices can analyse and recommend defibrillation in 3 seconds, can use ATC/AVF and can charge in the background, which reduces interruptions (Israelsson et al, 2017).
Ethically, theoretically and empirically, there are grounds for multiple SAED versus MD open-label randomised controlled trials, using the most modern SAED devices, with AVF/ATC technologies, capable of the fastest rhythm analysis and background charging. These trials can then inform a future OHCA-specific ALS guideline and, additionally, offer data for the OHCAOR so that TTFD can be harnessed as a reportable outcome that directly affects the epidemiology and ‘management of OHCA.
Limitations
This study used comparative head-to-head studies involving both strategies so that both treatment arms were given equal priority and weighting to reduce reporting/confounder bias. Non-comparative studies could have yielded influential results, although this would have reduced precision by increasing variables and denied the systematic review the opportunity to cross-examine both strategies and devices in real-time or simulated OHCA, while allowing human factors to influence the episodes (Higgins and Green, 2008).
Conclusion
In conclusion, the optimal defibrillation strategy for OHCA is a complex issue that requires careful consideration of various factors, including TTFD, inappropriate shocks, CPR delays, initial shockable rhythm conversions, AVF/ATC technologies and overall survival outcomes.
While MD may offer a faster TTFD historically, the modern SAED can offer a shorter TTFD, reduce inappropriate shocks, charge in the background and overcome human factors in defibrillation, plus its science-based ancillaries can dramatically reduce interruptions (Kramer-Johansen et al, 2007; Nehme et al, 2017; Zijlstra et al, 2017; Badnjević et al, 2019; Hu et al, 2019).
This systematic review supports the RCUK (Soar et al, 2021) guidance for the use of MD because head-to-head defibrillation strategy comparison studies of TTFD for paramedics in OHCA and its effect on survival outcomes are lacking. This is a critical gap in research because a solution could improve TTFD and, ultimately, improve survival outcomes. Open-label randomised controlled trials are needed to ascertain which is the superior strategy for paramedic-led OHCA episodes, evaluating both strategies with modern SAED technologies.
Additionally, training programmes should be implemented to ensure that emergency medical personnel are proficient in using both MD and SAED and can make informed decisions about the optimal defibrillation strategy for each patient. Furthermore, technological advances such as AVF for CPR with perfusion indicators should be further explored to improve overall compression depths, rates and recoils, leading to increased survival rates.
Overall, a multifaceted approach incorporating technological advances, ongoing research and training programmes is necessary to ensure that the most effective defibrillation strategy is employed for OHCA patients, ultimately improving survival and reducing mortality rates.

