In the UK, there are approximately 1200 spinal injuries per year (McDaid et al, 2019). The majority are caused by road traffic collisions, falls from height or violence (World Health Organization (WHO), 2013). Of these injuries, about 50% occur in the cervical spine, 37% in the thoracic spine and 11% in the lumbar spine.
Damage to the spinal cord can cause a temporary or permanent loss of function that can be complete or incomplete depending upon the extent of cord injury (Diaz, 2019). Spinal cord injury often results in the loss or impairment of motor and/or sensory function, as well as of autonomic function and bladder and bowel control (WHO, 2013).
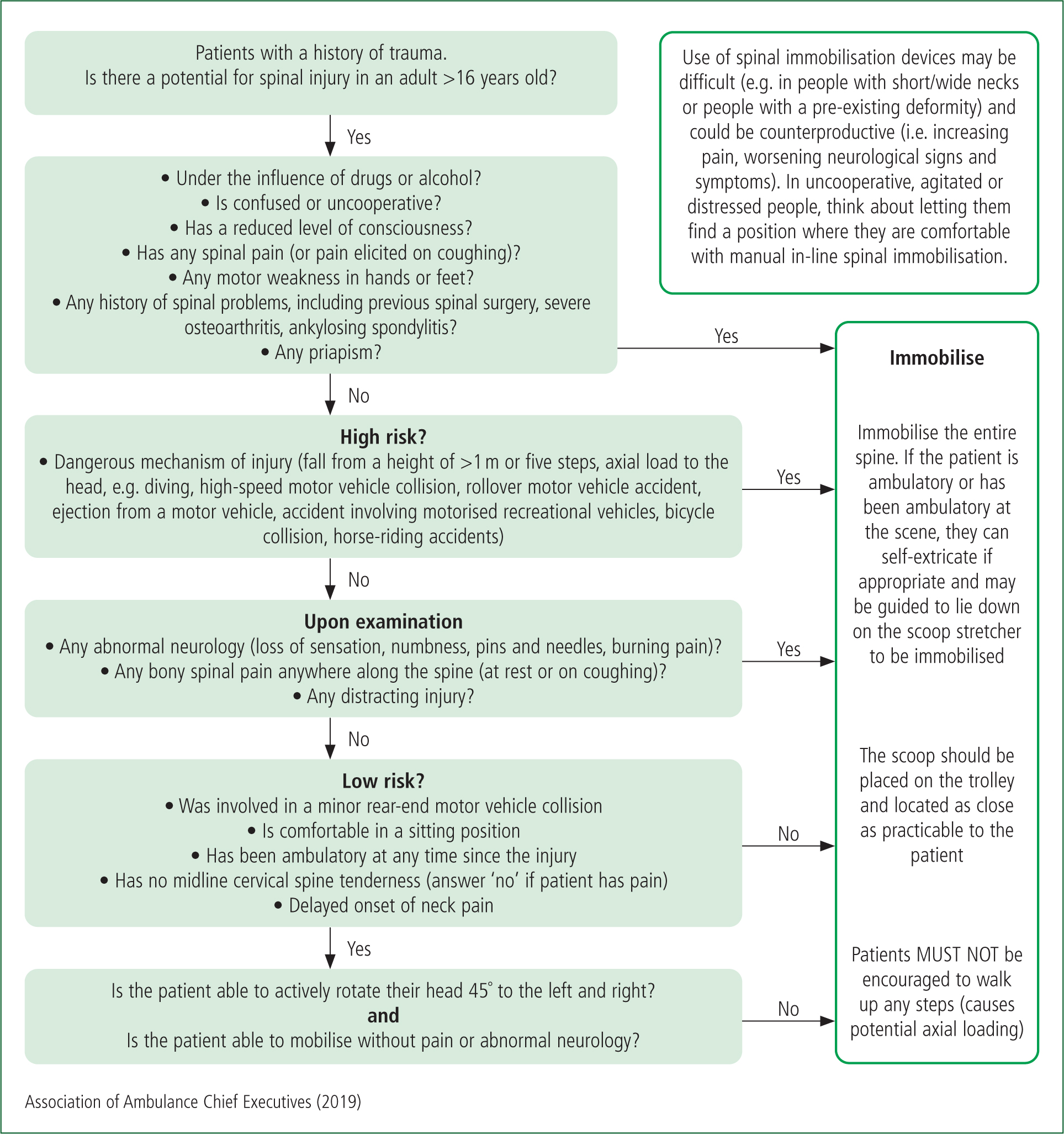
Prevention of movement of an unstable spine causing secondary injury to the spinal cord led to the process of immobilising all suspected spinal injuries in the 1960s (Ellis et al, 2014). The practice became widespread across Europe and North America with spinal immobilisation being included in the Advanced Trauma Life Support guidelines, which were considered the standard of care (American College of Surgeons, 2009). Spinal immobilisation involves maintaining the person in a neutral alignment while positioning them on an orthopaedic scoop stretcher, maintaining the head and neck alignment manually until a semi-rigid collar is applied, then using head blocks to restrict movement. The patient is then secured to the stretcher with straps (Association of Ambulance Chief Executives (AACE), 2019).
The efficacy of semi-rigid collars has been questioned by Clemency et al (2021), and Hawkridge et al's (2022) systematic review found that most studies did not support the prehospital use of spinal collars. Oosterwold et al (2017) identified potential issues with immobilisation as nausea/vomiting, pain, shortness of breath and combativeness/anxiety.
Häske et al (2022) found that the practice of lying on an orthopaedic scoop stretcher for prolonged periods of time can cause pressure ulcers, pain and restrictions to ventilation, which led them to recommend spinal motion restriction as sufficient to prevent unsafe movement when transporting patients. Cowley et al (2022) found that some groups were more prone to issues with scoop stretchers (bariatric, agitated, older and paediatric patients and those with spinal abnormalities) and recommended a clearer assessment of risk before transporting them. Häske et al (2022) and Cowley et al (2022) said further training was needed in tools and protocols to develop greater consistency in practice. Oosterwold et al (2017) demonstrated that paramedics will problem-solve at the scene and may improvise in practice.
Algorithms and checklists have been developed to identify patients most likely to have a spinal injury, thereby preventing people with low-risk or non-spinal injuries being immobilised.
The Canadian C-Spine Rule (Stiell et al, 2001) is used in the National Institute for Health and Care Excellence (NICE, 2016) guideline for the assessment and initial management of spinal injury. NICE recognises there are potential difficulties in applying this checklist to children as a child's developmental stage should be considered. The algorithm used by UK paramedics (AACE, 2019), is based on the NICE (2016) guidelines and Canadian C-Spine Rule (Stiell et al, 2001) (Figure 1).
This study explored how paramedics implemented protocols and some of the factors that influenced their decisions in practice.
Methodology
This research was conducted as part of an MSc in advanced practice (prehospital care) at the University of Greenwich. It was a quantitative survey that used a convenience sample by approaching every eligible frontline clinician in the London Ambulance Service NHS Trust (LAS) (Table 1). Ethical approval was gained from both the university and the trust.
| Inclusion criteria | Exclusion criteria |
|---|---|
| All patient-facing roles: |
|
The survey was developed through drawing on clinical experience, peer group and evidence-based review of the immobilisation algorithm (Appendix A). The questions were written into online survey platform Qualtrics. The platform also checked the proposed questions for flow and ambiguity. A pilot study involving three of the researcher's colleagues was carried out to ensure access and clarity.
The survey was then published on the Trust intranet and made available from 9 March to 4 April 2020. A link to the intranet bulletin containing the survey was emailed to every employee once a week (approximately three times across the period described). There were no responses after 22 March, which was related to the COVID-19 pandemic.
There were 4096 eligible clinicians and 392 responses were received. The data set was cleaned to remove entries with incomplete demographic data (n=38), resulting in a sample of 354.
Data analysis
Univariate analysis was used to investigate whether there were any differences between paramedic and other staff. To investigate the association between frequency of algorithm use and the other study variables, a dichotomous variable was created dividing the responses into frequent versus infrequent users of the algorithm.
To analyse knowledge levels relating to indicators for full spinal mobilisation, a score was derived based on correct and incorrect responses.
Age and length of service were chosen as the variables of interest following the findings of Considine et al (2007). These authors identified that knowledge and experience, age and length of service influenced the triage decision-making process.
Numerical/ordinal variables were tested by either independent sample t-tests or Mann-Whitney U tests depending on the distribution of the data. Categorical variables were analysed by cross tabulation, which produced a chi-square statistic. The cut-off point for rejecting the null hypothesis was P<0.05.
Results
Three hundred and fifty-four paramedic and non-paramedic clinical staff were recruited. The statistics for age and length of service with LAS were as follows: mean age 37.9 years, SD 10.8; length of service mean 9.3 years, SD 8.2.
The type of jobs reported were divided into: advanced paramedics (n=22; 6.2%); paramedics (n=183; 51.6%); paramedic team leaders (n=32; 9%); clinical tutors (n=16; 4.5%); non-paramedic clinicians (n=97; 27.4%); and management roles (n=16; 4.5%). These were then categorised into two groups: paramedics (n=247; 69.8%); and non-paramedics (n=107; 30.2%).
A number of analyses were performed to see if there was any difference between paramedics and other staff. There was no significant relationship regarding age (P>0.3) but paramedics were likely to have been employed for longer: paramedics: n=247, 10.1 years mean, SD 8.1; non-paramedic staff: n=107, 7.8 years mean, 8.3 SD; two-tailed Mann-Whitney U test: U=27.2; P< 0.001.
Frequency of use of the algorithm
Three hundred and forty-four participants responded to the question concerning frequency of use of the algorithm. Answers were converted into a 5-point scale (always=1; never=5), and produced the following statistics: mean 2.65; median 3.00; SD 1.17; range 1–5.
For ease of analysis, they were categorised as more likely (always, most of the time and occasionally) n=261 and ‘less likely’ (hardly ever, never); n=83 (Table 2).
| Use of the algorithm | Frequency | Percentage |
|---|---|---|
| 1, 2, 3 (always, most of the time, occasionally) | 261 | 76% |
| 4, 5 (hardly ever, never) | 83 | 24% |
| Total | n=344 |
There were no significant associations between age (P=0.178), length of time with LAS (P=0.951) and paramedic status (P=0.710) and frequency of use of the JRCALC algorithm. However, those who believed too many people were immobilised unnecessarily had a higher frequency of use of algorithm scores: two-tailed independent sample t-tests: n=191, mean 2.80, SD 1.15; n=123, mean 2.52, SD 1.17; immobilised unnecessarily:not immobilised unnecessarily (t=2.03; P=0.043).
Under the influence of alcohol and drugs
Length of time in LAS was not significantly related to this variable (P=0.342) but older participants were more likely to correctly endorse this item (two-tailed independent sample t-test: n=104, mean 40.2, SD 12.7; n=220, mean 37.4, SD 9.9; yes:no (t=2.17, P=0.031).
Less frequent use of the JRCALC algorithm was associated with not endorsing being under the influence of alcohol and drug as an indicator for full spinal mobilisation at a borderline significant level: two-tailed independent sample t-test: n=219, mean 2.78, SD 1.11; n=103, mean 2.50, SD 1.25; less frequent:frequent, t=−1.93, P=0.054).
Higher knowledge scores relating to indicators of full spinal mobilisation were associated with endorsing this item: two-tailed independent sample t-test: n=104, mean 5.59, SD 0.95; n=221, mean 4.21, SD 1.19; (t=11.2, P<0.001).
Finally, individuals who did not endorse being under the influence of drugs or alcohol were less likely to believe that too many people were being immobilised unnecessarily: two-tailed chi-square tests: n=187 (n=49, 26.2%; n=138, 73.7%; yes, no); n=121 (n=46, 38.0%; n=75, 62%; yes, no); chi-square=4.80, P=0.028).
Knowledge of indicators of full spinal mobilisation
On this occasion, 325 (91.8%) participants completed the questionnaire; data were missing from 29 participants. The results are shown in Table 3. All participants endorsed spinal pain; other correct responses, in descending order, were tingling or numbness in the extremities, reduced Glasgow Coma Scale score, history of a spinal condition or spinal surgery, weakness in any hand or foot, pelvic injury and, finally, being under the influence of alcohol or drugs. One item in the question did not appear in the algorithm, namely e) penetrating injury to the head, and was endorsed by nearly three-quarters of the sample.
| Number | Percentage | |
|---|---|---|
| a) Reduced Glasgow Coma Scale score | 264 | 81.2 |
| b) Spinal pain | 325 | 100.0 |
| c) Tingling or numbness in extremities | 311 | 95.6 |
| d) Under the influence of alcohol or drugs | 104 | 32.0 |
| e) Penetrating injury to the head | 235 | 72.3 |
| f) Weakness in any hand or foot | 218 | 67.0 |
| g) History of any spinal condition or spinal surgery | 219 | 67.3 |
| h) Pelvic Injury | 217 | 66.7 |
These responses were then converted into a knowledge score. All items that were endorsed other than e) were scored as a 1 and item e) was scored −1. The knowledge scores (n=325) were: mean 4.65, median 5.00, SD 1.29 and range 1–8.
There was a very weak and non-significant relationship between knowledge scores and age (r=0.08; P=0.181). Staff who were not paramedics had higher scores than paramedics (two-tailed independent sample t-test: n=225, mean 4.5, SD 1.3; n=97, mean 4.89, SD 1.2; paramedic:non-paramedic (t=−2.18, P=0.030).
Those who felt there was not too much unnecessary immobilisation had higher knowledge scores: two-tailed independent sample t test: n=121, mean 4.84, SD 1.25; n=187, mean 4.54, SD 1.29; not immobilised unnecessarily: immobilised unnecessarily (t=−2.03, P=0.043).
Finally, higher knowledge scores were associated with more frequent use of the algorithm: two-tailed independent sample t-test: n=150, mean 4.83, SD 1.22; n=172, mean 4.51, SD 1.33; frequent:infrequent: t=2.23; P=0.026).
Are too many patients immobilised unnecessarily?
Three hundred and fourteen (88.9%) participants replied to the question on whether they believed too many people were being immobilised unnecessarily. More than 60% (n=191; 60.6%) thought this was the case with nearly 40% (n=123; 39.4%) replying no.
There was no significant relationship between this belief and age (P=0.950) or length of time employed by LAS (P=0.199). Paramedics were more likely to believe too many people were immobilised unnecessarily. The following are the positive responses: two-tailed chi-squared test: n=223 (n=153, 68.6%); n=91 (n=38, 41.7%); chi-square=19.5; P<0.001).
Influence of drugs and alcohol
Table 3 shows that being under the influence of alcohol and drugs was only endorsed by a third of the sample, indicating a knowledge gap.

Discussion
The key findings of the study were:
Recognition of alcohol and drug intoxication
All respondents recognised that patients who met the inclusion criteria of the algorithm (aged >16 years with a history of trauma and a risk of spinal injury) presenting with spinal pain required full spinal immobilisation.
However, only one-third identified that patients under the influence of drugs or alcohol also needed full immobilisation. Older, more experienced respondents were more likely to endorse this correctly. The consensus opinion on validated immobilisation criteria is that patients under the influence of drugs or alcohol cannot have their C-Spine cleared in the prehospital environment (Hoffman et al, 2000; Vaillancourt et al, 2009; NICE, 2016; AACE, 2019). This inclusion is based on the disproportionately high number of spinal injuries in this patient group (Garrison et al, 2004; Stroud et al, 2011; Eldridge et al, 2019).
There is evidence that ambulance clinicians sometimes deviate from correct application of the validated criteria, although no explanation has been provided for this (Domeier et al, 2005; Kreinest et al, 2017; Geduld et al, 2022; Vaillancourt et al, 2023). Myers et al (2009) related this non-compliance specifically to prehospital assessment of intoxicated patients, although Vaillancourt et al (2023) concluded that ambulance clinicians can apply validated criteria safely. Domeier et al (2005) and Sebastian (2001) considered that paramedics, although risk averse, missed injuries when the criteria were not applied appropriately.
A review of immobilisation criteria by Michaleff et al (2012) recommended improved education to facilitate greater use of the rules with particular attention to subjective components such as intoxication as they are frequently misinterpreted.
Knowledge of the algorithm and full spinal immobilisation
It was expected that education and experience would positively influence the use of the algorithm, but paramedics recorded lower knowledge scores regarding full spinal immobilisation than non-paramedics. This may be attributed to the difference in academic pathways of frontline ambulance clinicians, which leads to different styles of clinical decision-making.
University graduate paramedics are educated in hypothetico-deductive reasoning—a structured approach to patient assessment underpinned by deeper learning—while non-paramedic clinicians continue to be educated in the intuitive model, which uses a more superficial approach to learning and involves reliance on checklists and algorithms for decision making (Ryan and Halliwell, 2012; Health and Care Professions Council, 2021; FutureQuals, 2023).
It might therefore be expected that non-paramedics would use the algorithm more readily than paramedics and produce higher knowledge scores on full spinal immobilisation because of their familiarity with it; further research is required to determine if this is the case.
Ebben et al's (2014) study explored the lived experience of paramedics and nurses in applying guidelines, and found that individual experience and the external and organisational environment all influenced paramedic adherence to protocols. A similar study involving UK ambulance clinicians might provide greater insight into the different behaviours identified in this study.
Too many patients being immobilised unnecessarily
While paramedics had lower knowledge scores on spinal immobilisation, they were more likely to believe that too many patients were being immobilised unnecessarily. It is not clear from the data whether paramedics believed that they apply full spinal immobilisation unnecessarily or that the algorithm captures false positives; further investigation is required to explore the context of this.
The findings relate to themes in the literature of disproportionate risk aversion in paramedic decision-making, identification of false positives and overimmobilisation when applying validated spinal immobilisation criteria (Domeier et al, 2005; Vaillancourt et al, 2009; O'Hara et al, 2015). A review of the implementation of the Modified Canadian C-Spine Rule by paramedics (Vaillancourt et al, 2023) concluded that they can safely apply the rules to low-risk trauma patients and reduce the number of patients immobilised during transport; this suggests that, if the algorithm is being applied appropriately, there would be a reduction in unnecessary immobilisation.
Limitations
The study was conducted as part of an MSc degree with fixed time and resource limits.
The questionnaire was released in late February 2020 and responses dropped off sharply as the COVID-19 pandemic escalated. At the beginning of March, LAS dealt with the unprecedented impact of the virus on its services.
The author acknowledges that the sample size was smaller than anticipated but the time restrictions of the MSc course precluded extending the data collection period.
Conclusions
The study has highlighted a knowledge gap on the rules of spinal immobilisation that should be considered in the development and delivery of both paramedic and non-paramedic education.
Further research is required to determine why there is poor recognition that traumatically injured patients need to be assessed for intoxication with drugs or alcohol if immobilisation is to be removed.
The belief that too many patients are immobilised also requires further investigation. Recent evidence showing that paramedics can safely apply rules to low-risk trauma patients and reduce the need for immobilisation during transport suggests knowledge of the algorithm or confidence in its use is insufficient and further education on the rules is required.

