High quality cardiopulmonary resuscitation (CPR) has been linked to improved survival outcomes for cardiac arrest patients (Kramer-Johansen et al, 2006; Babbs et al, 2008; Christenson et al, 2009; Stiell et al, 2014; Sutton et al, 2014; Vadeboncoeur et al, 2014; Idris et al, 2015; Perkins et al, 2015a; Perkins et al, 2015b; Talikowska et al, 2015). To promote the delivery of high quality CPR by healthcare professionals, a number of Emergency Medical Services (EMS) worldwide have introduced CPR feedback devices into routine clinical use. An example of one such device is the Q-CPRTM developed by Laerdal Medical and Philips Healthcare. It comprises a force sensor and an accelerometer, and, placed underneath the hands of the rescuer, it delivers both visual and (optional) auditory feedback to the user in real-time about their CPR performance. Specifically, it provides feedback on parameters such as compression depth, compression rate, adequate chest recoil and time without compressions (‘hands-off time’). In addition, information about ventilation rate is captured by measuring transthoracic impedance using the multifunction defibrillation pads (Laerdal Medical Corportation, 2016, Philips Healthcare, 2011).
In July 2014, St. John Ambulance Western Australia (SJA-WA) introduced Q-CPR as a mandatory tool for all metropolitan ambulance crews to use when attempting to resuscitate victims of out-of-hospital cardiac arrest (OHCA). Initial usage rates were as high as 43% of attempted resuscitations within the first month; however, they gradually declined, dropping to 13% in December 2015. The reasons for this were not clear. In the literature there are limited reports that shed light on the possible reservations of clinical staff towards using such devices. One study of a helicopter EMS (HEMS) in Turku, Finland, found that among the eight physician respondents, the most common reason cited for not having used CPR feedback was that the Q-CPR device had not been transported to the scene (Sainio et al, 2013). In another study by Perkins et al (2005), hand and wrist pain was frequently reported by participants using the CPREzyTM feedback device during simulated cardiac arrest. Similarly, van Berkom et al (2008) stated that CPR feedback had been associated with rescuer complaints such as ‘stiff wrists’. To investigate why Q-CPR implementation rates were low and declining over time, and to identify specific, paramedic-reported barriers towards the usage of CPR feedback devices, SJA-WA issued survey to a sample of the metropolitan ambulance workforce.
Methods
A voluntary, anonymous survey was distributed to SJA-WA paramedics participating in clinical refresher and research training courses from September 2015 to December 2015. The survey consisted of 11 questions that required participants to either select a binary or multiple choice answer or provide a rating on a five point Likert scale ranging from ‘strongly agree’ to ‘strongly disagree’. For three questions, free text answers were permitted. A copy of the survey form is available in Appendix A.
SJA-WA paramedics of all levels of experience were given an opportunity to participate in the survey, ranging from ‘on-road’ undergraduate paramedic students to senior positions such as that of Clinical Support Paramedic and Area Manager. The survey did not request information that would allow the participant to be identified, such as name, date of birth or staff ID. While hard copies of the survey were distributed and collected by SJA-WA on their premises, data analysis was performed by researchers at the Prehospital, Resuscitation and Emergency Care Research Unit (PRECRU) at Curtin University. Ethical approval was obtained from the Human Research Ethics Office at Curtin University (RDHS-209-15).
St. John Ambulance WA
SJA-WA is the sole provider of road EMS in Perth, Western Australia. Perth has a population of approximately 2.0 million within a land area encompassing approximately 6 418 square kilometers (Australian Bureau of Statistics). At the time of the survey, SJA-WA employed 769 paramedics to service this area. Use of the Q-CPR device is mandated in OHCA resuscitations of patients 8 years of age or older, with the exception of those cases where the LUCAS (Lund University Cardiopulmonary Assist System) mechanical compression device is in use (St John Ambulance Western Australia, 2016). Q-CPR devices are carried by all metropolitan ambulance vehicles, whilst the LUCAS device is carried by two on-duty Clinical Support Paramedics and three Area Managers who transport it to the resuscitation scene using a designated support vehicle. Two ambulance vehicles, staffed by two paramedics per vehicle, are dispatched on Priority 1 (lights and sirens) to every OHCA. A Clinical Support Paramedic or Area Manager also attends all attempted resuscitations.
Data analysis
Sample size calculations showed that 257 responses were required in order to produce an error margin of 5% (Australian Bureau of Statistics – National Statistical Service, 2015). Descriptive tables and figures were generated in Stata SE13.1 (StataCorp LP, College Station, Texas USA) or Microsoft Excel Version 14.0.7166.5000 (Microsoft Corporation, Redmond, Washington, USA). Stata was used to perform chi-squared tests where comparisons were made between groups of respondents. All statistical tests were assessed at the 5% level of significance.
Results
Description of respondents
There were 264 survey responses received, representing an estimated response rate of over 80% of those paramedics who were given the opportunity to participate. Respondents' level of experience ranged from ‘Student’ to ‘Level 3’ Paramedic. In total 255 respondents (96.6%) were qualified career paramedics, six respondents were undergraduate students (2.3%) and two were Community Paramedics (0.8%) who provide training, clinical and operational support to volunteer ambulance sub centres. One respondent did not provide identifying information. All respondents are governed by the same requirement for mandatory use of Q-CPR. ‘Level 3’ paramedic is the highest qualification attainable for SJA-WA paramedics; this group represented 45% of all respondents (n=119). Almost three quarters of respondents (n=190) were male.
Usage of Q-CPR
Ninety three percent of all respondents (n=246) indicated that they had attended a cardiac arrest within the past year, in other words, within the timeframe during which use of the Q-CPR was compulsory. However, of those, 41% (n=100) reported having used the Q-CPR during their last attempted resuscitation.
Reasons reported for not having used Q-CPR
The primary reason reported for not having used the Q-CPR was that the LUCAS mechanical compression device had arrived on scene; this was reported in 40 cases (37% of 109 valid responses) (Table 1). The second most commonly reported reason, cited in 22 cases (20%), was that respondents prioritised other interventions such as securing the airway, setting up an intravenous (IV) line or administering therapeutic drugs over use of the Q-CPR. The third most commonly reported reason, cited in 19 cases (17%), was that use of the Q-CPR was associated with pain experienced by the person doing chest compressions. Other reasons were less frequently reported. Valid responses were considered to be those that featured only a single response to question seven instead of having multiple responses selected; nevertheless had multiple responses been permitted, this did not change the distribution of the top three reasons for not having used Q-CPR.
| Reason reported | Number of responses | Percentage of responses |
|---|---|---|
| Clinical Support Paramedic or Area Manager arrived with the LUCAS device | 40 | 37% |
| We saw other procedures as a priority | 22 | 20% |
| Q-CPR causes pain to the person doing chest compressions | 19 | 17% |
| Worried about damage to the patient's chest | 2 | 2% |
| “Other”(variety of other reasons) | 26 | 24% |
Anticipating the arrival of the LUCAS device
As stated previously, the arrival of the LUCAS device was the most commonly cited reason for not having used the Q-CPR. In another section of the survey that required respondents to rate their answers on a scale ranging from ‘strongly agree’ to ‘strongly disagree’, 43 respondents (18%) from among the 234 who provided a valid response, agreed or strongly agreed that they would intentionally delay initiating use of the Q-CPR in anticipation of the arrival of the LUCAS device on scene.
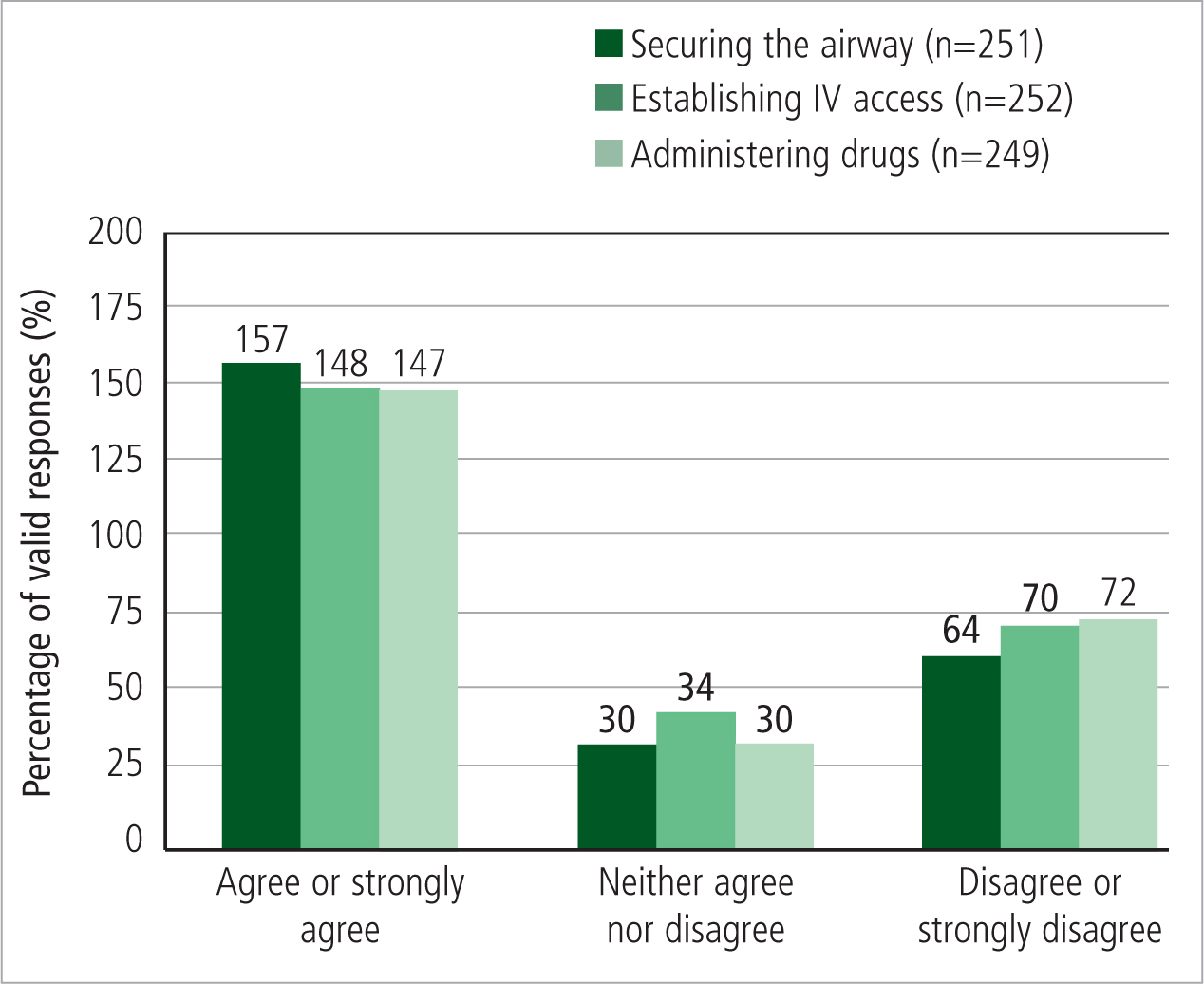
Prioritisation of other procedures above use of the Q-CPR
Approximately 60% of respondents agreed or strongly agreed that they would prioritise other interventions over use of the Q-CPR (Figure 1). This does not mean that they would prioritise other interventions over performing chest compressions in general; 235 (96%) of those who provided a valid response rated chest compressions as the first or second most important intervention when managing a confirmed cardiac arrest patient. However, the majority would postpone using the Q-CPR device in favor of securing the airway, establishing IV access or administering therapeutic drugs.
Pain experienced while using the Q-CPR
Over three quarters of respondents (n=190) either agreed or strongly agreed that using the Q-CPR on a manikin during training caused pain (Figure 2). Significantly more women reported pain than men (c2(2, N=247)=9.7135, p=0.008). In regards to using the Q-CPR on a patient, 141 (62%) either agreed or strongly agreed that it caused pain. Again significantly more women agreed or strongly agreed than men (c2(2, N=227)=6.3625 p=0.042). A sensitivity analysis was performed to compare responses between those who had reported using the Q-CPR during their last attempted resuscitation versus those who had not. Significantly fewer of those who had used the Q-CPR reported experiencing pain compared to those who had not used it (c2(1, N=221)=5.0503, p= 0.025). Nevertheless 55% (n=53) of respondents who had recently used Q-CPR reported pain.

The Q-CPR appeared to cause pain during short as well as long resuscitations; only 49 respondents (22%) agreed or strongly agreed that the Q-CPR is only painful during long resuscitations (Figure 2). Approximately half (n=112) either disagreed or strongly disagreed with this statement. In a sensitivity analysis that compared responses between those who had reported having used the Q-CPR during their last attempted resuscitation and those who had not, significantly more of those respondents who had recently used the device agreed or strongly agreed that pain results only from extended use of the Q-CPR (c2(1, N=214)=5.1355, p= 0.023).
Of the free text comments that were received at the end of the survey, the largest number were complaints about the current design of the Q-CPR (n=22), together with complaints about pain associated with use of the Q-CPR (n=20) (Appendix B).
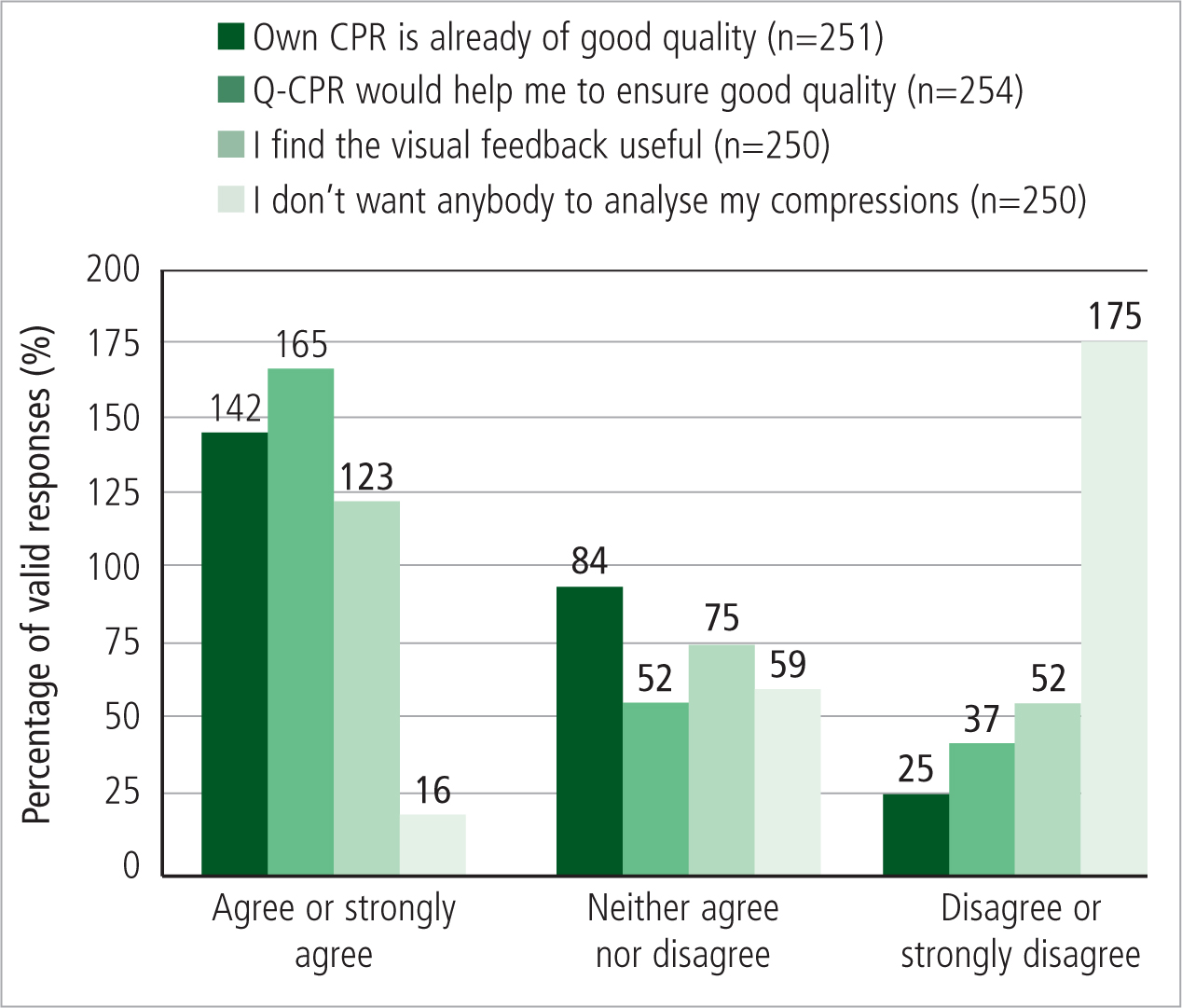
Opinions of quality of own CPR and usefulness of Q-CPR
Over half of respondents (n=142) agreed or strongly agreed that their CPR was already of “good quality” while only 25 respondents (10%) either disagreed or strongly disagreed with this statement (Figure 3). At the same time, 165 respondents (65%) either agreed or strongly agreed that using Q-CPR would help them to ensure that their CPR was of good quality. A total of 123 respondents (49%) found the visual feedback from Q-CPR useful. Only 16 respondents (6%) either agreed or strongly agreed that they did not want anybody analyzing the quality of their chest compressions.
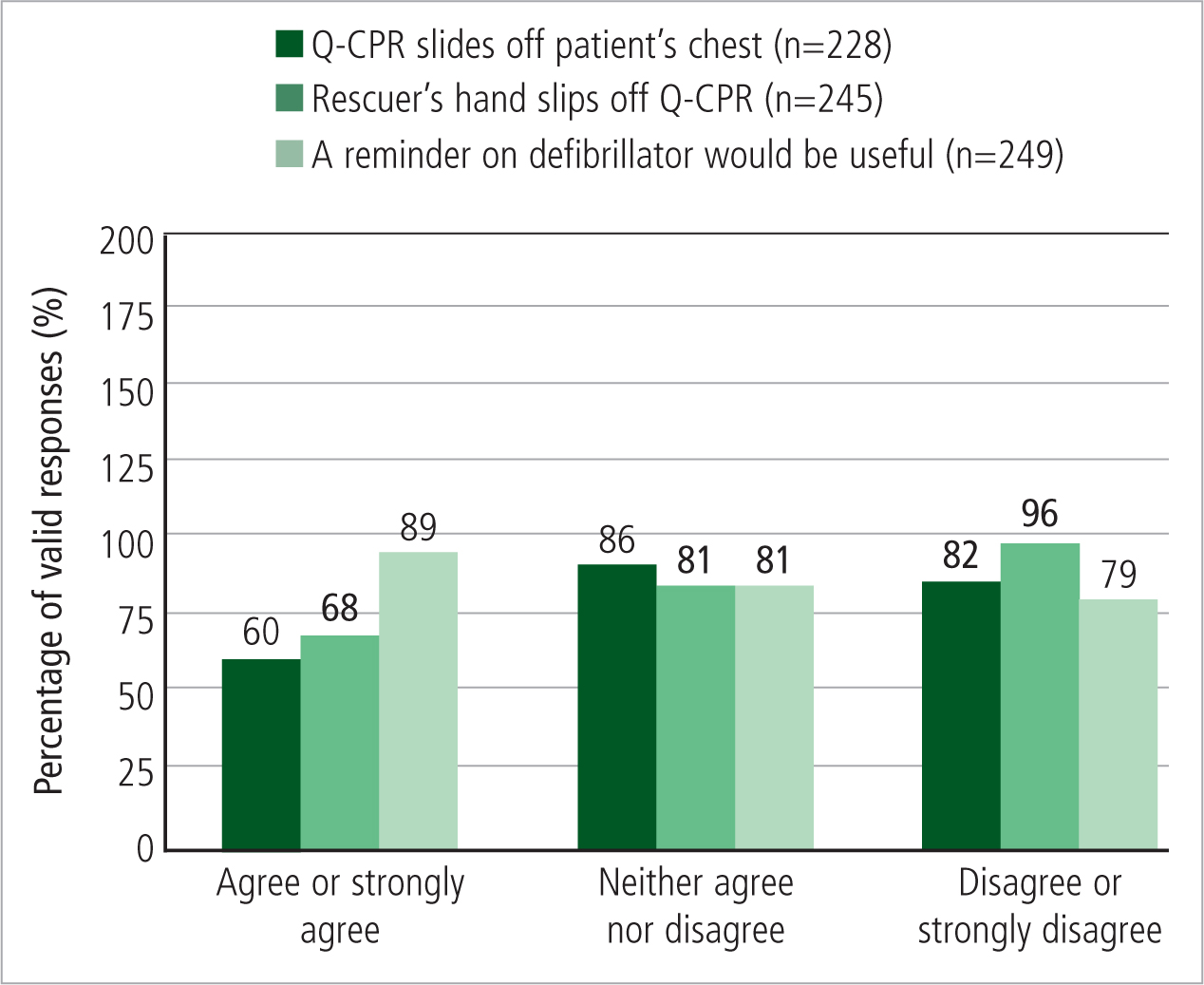
Practical considerations associated with use of Q-CPR
Twenty six percent of respondents (n=60) either agreed or strongly agreed that the Q-CPR slides off the patient's chest when in use (Figure 4). Twenty eight percent (n=68) either agreed or strongly agreed that their hand easily slips off the Q-CPR when doing chest compressions. Thirty six percent (n=89) agreed or strongly agreed that an additional reminder on the Philips HeartStart MRx defibrillator would prompt them to use the Q-CPR.
Discussion
Although 65% of respondents agreed or strongly agreed that using Q-CPR would help them ensure that their CPR is of good quality, implementation rates fell notably short of this number. Rates were comparable to those reported by Sainio et al (2013) for the helicopter EMS in Finland, where, over a period of 18 months, Q-CPR was used in 28% of attempted resuscitations. In the case of SJA-WA, survey results revealed that the most frequently reported reason for its non-use was its lower prioritization in the OHCA response algorithm by respondents compared to other equipment and other interventions.
Specifically, the primary reason reported for not having used the Q-CPR during respondents' last attempted resuscitation was that the LUCAS device arrived on scene. The SJA-WA dispatch model for OHCA in Perth recommends that two ambulance vehicles are dispatched on Priority 1 to the scene, subsequently joined by one of two on-duty Clinical Support Paramedics or one of three Area Managers who arrive on Priority 1 with the LUCAS device. There can therefore be a delay between the arrival of the first dispatched crew, who will likely have been the closest available crew, and the Clinical Support Paramedic or Area Manager (carrying the LUCAS device) who could have been located anywhere within either the northern or the southern metropolitan area. Since all metropolitan ambulance vehicles carry the Q-CPR, in many cases an opportunity exists for crews to initiate use of the Q-CPR prior to the arrival of the LUCAS. In addition, SJA-WA records indicate that the LUCAS device was deployed in less than half (approximately 40%) of attempted resuscitations; it is primarily indicated for use by SJA-WA during the transportation of patients. Therefore it appears that some respondents may be missing an opportunity to apply the Q-CPR early in the resuscitation, prior to the arrival of the LUCAS.
The second reason most commonly reported for not having used the Q-CPR was that respondents prioritized other interventions, such as the administration of therapeutic drugs, setting up an IV line or securing the airway, over use of the Q-CPR. In fact approximately 60% of respondents agreed or strongly agreed that they would prioritize such interventions over use of the Q-CPR. While there is evidence that high quality CPR, in particular compressions of adequate depth and rate improves survival (Stiell et al, 2014; Vadeboncoeur et al, 2014; Idris et al, 2015), there is limited clinical evidence that other interventions such as the administration of adrenaline or the application of an advanced airway increase patient survival (Soar et al, 2015). Therefore earlier use of CPR feedback devices in the resuscitation effort should be promoted.
While approximately two thirds of respondents reported that the Q-CPR would help them to ensure that their CPR was of good quality, over half already considered their CPR to be of good quality. Without the automated measurement of CPR quality during resuscitation it is difficult to confirm whether this is true. Reports in the literature demonstrate that CPR quality is often suboptimal, even among trained rescuers (Abella et al, 2005; Wik et al, 2005). In regards to the measurement of CPR quality, only 6% of respondents expressed concern with having their CPR quality analysed. Nevertheless, if respondents already considered their CPR to be of good quality, this may have influenced the priority placed on using the Q-CPR.
Over three quarters of respondents reported experiencing pain while using Q-CPR during training and over 60% while using Q-CPR on a patient. The latter figure was reduced when considering only those respondents who explicitly reported having used the Q-CPR during their last attempted resuscitation, suggesting that Q-CPR may not be as painful in real arrests as paramedics would extrapolate from training. Nevertheless over half of those who had recently used the Q-CPR on a patient reported pain (55%). In an evaluation of the CPREzyTM feedback device during simulated cardiac arrest, Perkins et al (2005) found that 95% of participants reported discomfort in the heels of their hands and wrists. In addition, one participant sustained a soft tissue injury as a result of using the device. Similarly in a study by Zapletal et al (2014) one participant sustained an injury when using the CPR meterTM. In another study, van Berkom et al (2008) sought to determine whether using the CPREzyTM required any additional force compared to standard chest compressions performed without a feedback device. The investigation was carried out as a result of rescuer complaints of stiff wrists, as well as the perceived requirements for more force and increased rescuer fatigue. Results indicated that no additional force was required to achieve a given depth when using CPREzyTM however 21-26.5% more work was required to compress the CPREzy in addition to compressing the chest wall. In the SJA-WA survey, while a notable number of respondents reported experiencing pain when using the Q-CPR, less than one fifth reported this as the primary reason for not having used Q-CPR in their last attempted resuscitation. This suggests that most respondents would still consider using Q-CPR despite the discomfort that might be associated with its use.
One common feature of the above-mentioned CPR feedback devices that potentially could have contributed to the reporting of pain is a bulky and rigid design. In the free text comment section of the SJA-WA survey, there were several instances of paramedics calling for a flatter, wider or more flexible design. A change in design could potentially improve the comfort profile of the device, as well as minimizing the occurrence of other usability issues such as the feedback device sliding off the patient's chest or the rescuer's hand sliding off the device. Ideally such a design should be achieved without compromising on data accuracy or ease of recording.
Finally, although high quality CPR has been shown to be associated with improved patient survival (Stiell et al, 2014; Vadeboncoeur et al, 2014, Christenson et al, 2009; Idris et al, 2015; Perkins et al, 2015a; Perkins et al, 2015b) the link between the use of CPR feedback devices specifically, and improved patient survival has not been well established (Perkins et al, 2015a; Perkins et al, 2015b). Therefore the European Resuscitation Council Guidelines for Resuscitation 2015 call for CPR feedback or prompt devices during CPR to only be considered as part of a broader system of care that should include comprehensive CPR quality improvement initiatives rather than as an isolated intervention (Perkins et al, 2015a).
Limitations
The survey represented approximately one third of the SJA-WA paramedic workforce. In addition, only those who participated in refresher or research training programs were given the opportunity to partake in the survey. However, all paramedics are required to attend these training programs and therefore there is minimal risk of selection bias. While the responses of undergraduate paramedic students were included in the results, they represent 2.3% of all respondents and are governed by the same requirement to use Q-CPR during a resuscitation as qualified paramedics. This survey represents the personal opinions and experiences of paramedics; there has been no quantitative measurement of pain scores nor any form of objective measurement in relation to the use of the Q-CPR in this study apart from the tracking of usage rates. Only SJA-WA paramedics were surveyed, and as such the results may not be transferrable to other EMS in other locations.
Conclusion
Lower usage rates of the Q-CPR feedback device by SJA-WA paramedics within the Perth metropolitan area appeared to be primarily attributable to respondents assigning Q-CPR a lower prioritization within the OHCA response algorithm relative to other devices and interventions; and secondly due to pain experienced by paramedics when using the device. Pain was a frequent complaint among respondents both during training and when Q-CPR was used on a patient, however it did not appear to be the primary driver of paramedics' reservations towards using the device. While CPR feedback devices have the potential to improve CPR quality, their widespread uptake may be limited by the above-mentioned factors.
‘ Feedback devices for CPR have the potential to improve CPR quality among trained respondents’
