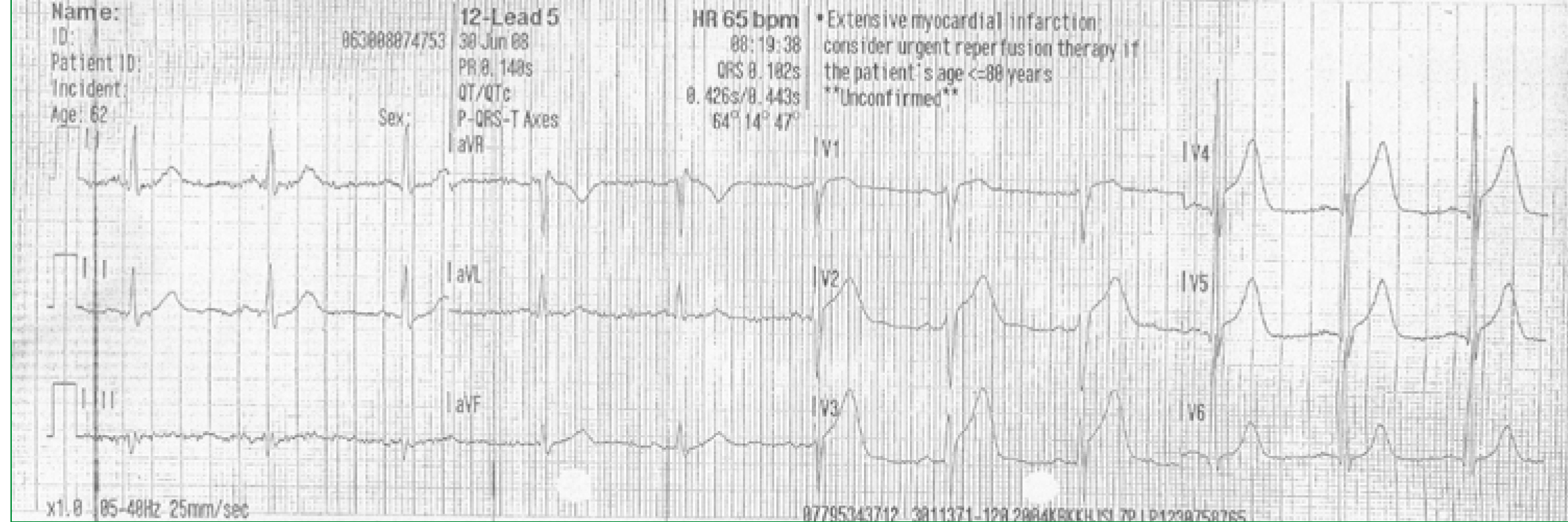
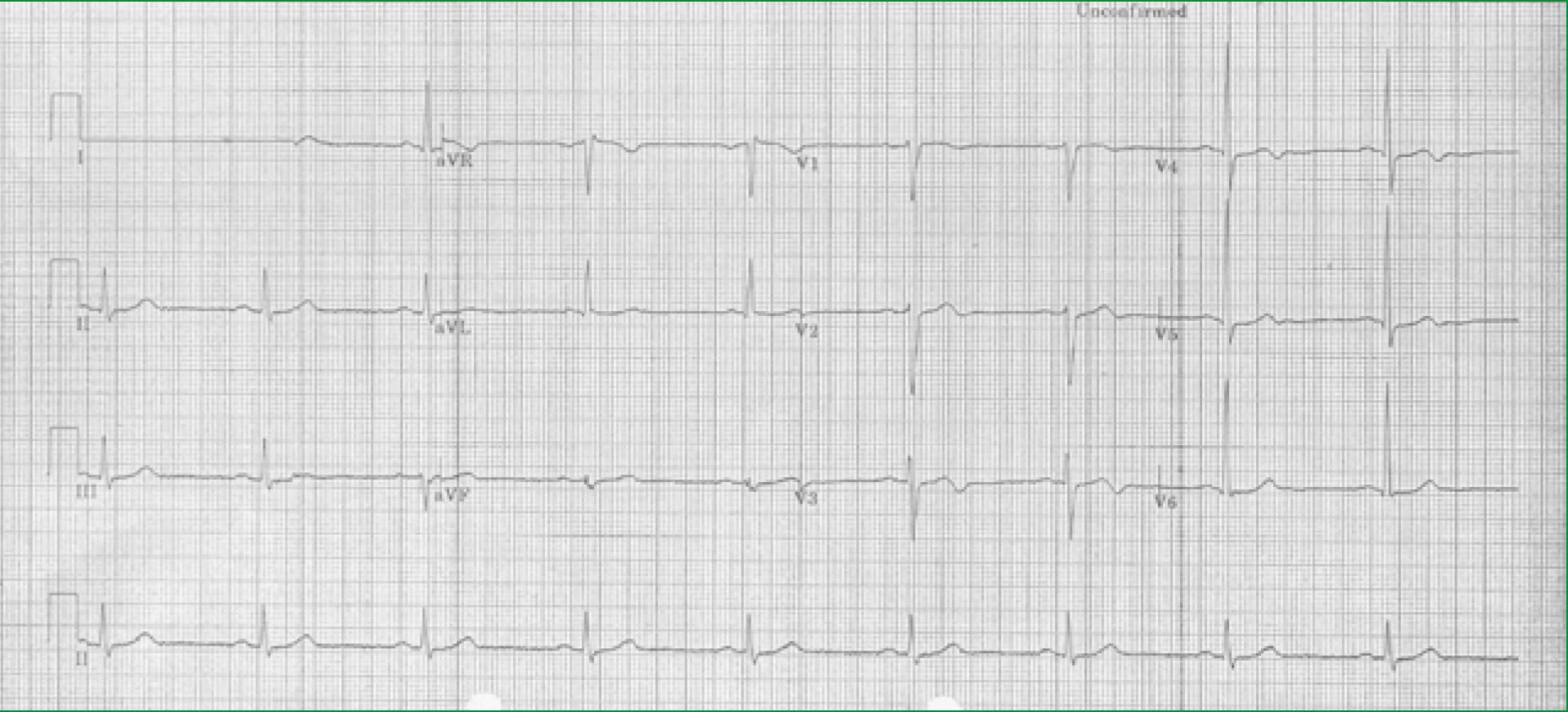
A 54-year-old male smoker living in a rural community over one hour from the regional cardiac centre has chest pain and after 15 minutes calls the emergency services. An ambulance arrives 8 minutes later. The paramedics confirm a diagnosis of myocardial infarction by recording an ECG, which shows ST segment elevation in the anterior chest leads (Figure 1). They give the patient aspirin and, after establishing that there are no contraindications to thrombolysis, administer tenecteplase 15 minutes after arrival on scene. His pain to needle time is 38 minutes. He is pain free on arrival to hospital and his ECG has returned to virtually normal (Figure 2). The following day he has coronary angiography, which reveals a tight stenosis in his LAD, which is treated by stent insertion. Echocardiography is normal and blood tests show a trivial elevation in Troponin T. He is discharged the following day with a diagnosis of aborted myocardial infarction. He has been very well served by prehospital thrombolysis (PHT) but in most parts of the UK this therapy is being abandoned for all but exceptional circumstances in favour primary percutaneous coronary intervention (PPCI), in this case a journey of one hour away. Why is this?
History of treatment of myocardial infarction
Early trials
The role of thrombosis causing coronary occlusion leading to myocardial infarction was originally proposed in the late 19th century (Hektoen, 1892). It was not universally accepted in 1958 when systemic thrombolysis was first administered as treatment for MI (Fletcher et al, 1958). The early trials were small and flawed in design. It was only after the development of cardiac catheterisation and the successful intracoronary application of thrombolysis that the scientific community fully appreciated the role of intracoronary thrombosis and potential benefit of restoring coronary artery patency by thrombolysis (Rentrop, 1979).
A new era of large trials established the mortality benefit of thrombolytic therapy especially when administered early after the start of symptoms (Fibrinolytic Therapy Trialists' (FTT) Collborative, 1994) and attention was then focussed on how to get treatment started as early as possible and how to maintain coronary artery patency in the long term. The best solutions to these two objectives, PHT and PPCI, seem to be mutually exclusive despite many attempts to find the perfect combination of the two.
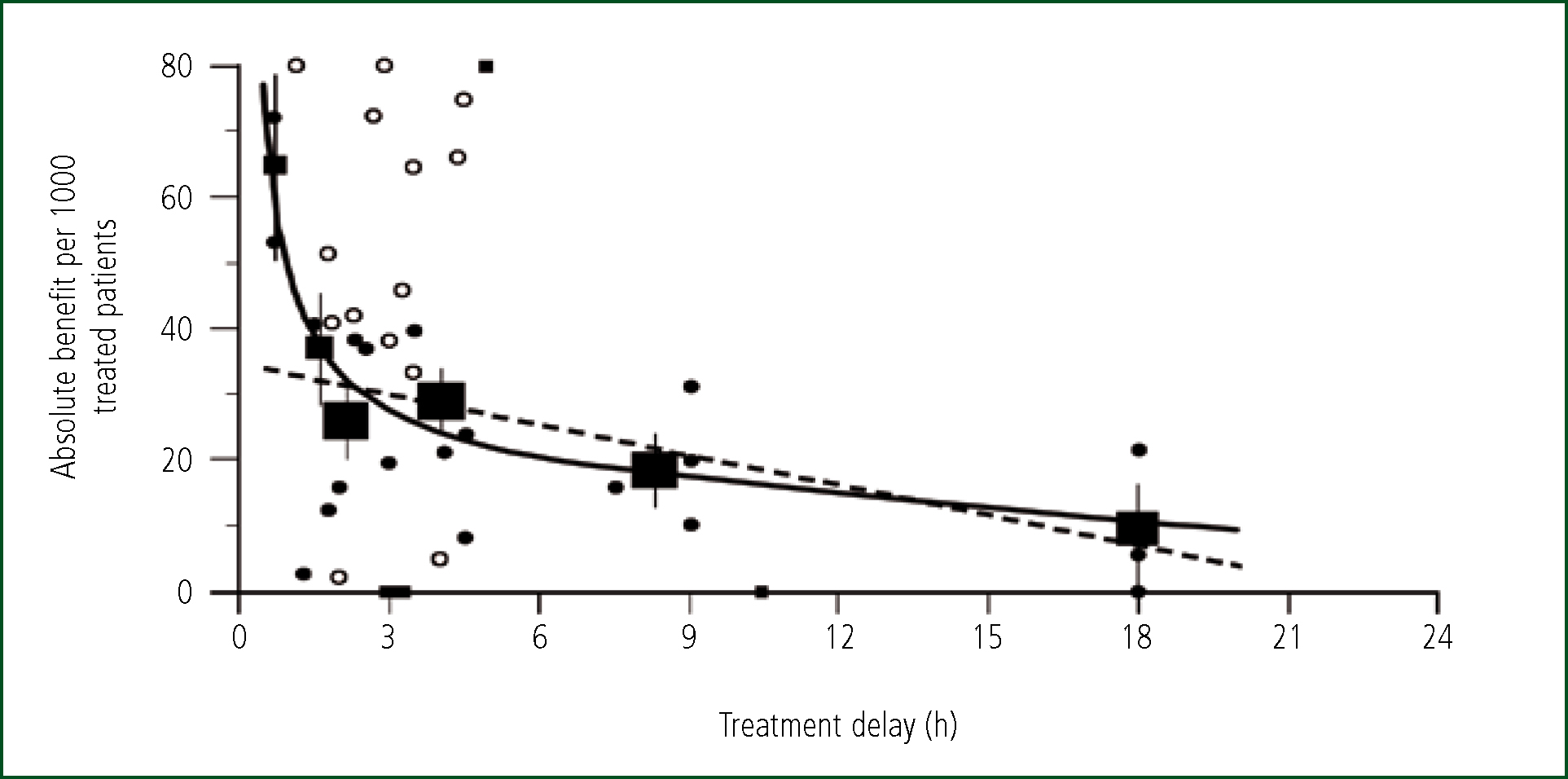
The Boersma analysis of the thrombolytic trials (Boersma, 1996) demonstrated that while benefit from thrombolytic therapy persists for up to 12 hours after the onset of symptoms, the benefit is particularly large if treatment is given within two hours (Figure 3). Fresh thrombus is unorganised and rapidly dissolved by thrombolytic agents restoring blood flow to not yet irreversibly damaged myocardium. Very early treatment may prevent any myocardial damage. Treatment administered later in the course of infarction works less quickly and cannot prevent some muscle necrosis with the consequent long-term effects on ventricular function and electrical stability. To get the most out of thrombolysis, and the most benefit for patients, hospitals sought ways to speed up time to treatment, initially by moving it from CCU (cornonary care unit) to the emergency department (Hetherington et al, 2002). The logical next step was to take the treatment directly to the patient by ambulance.
Pre-hospital thrombolysis
About 20 years ago several clinical trials were undertaken to investigate whether thrombolysis given quickly in the more vulnerable out of hospital environment would result in better outcomes than thrombolysis given later in the more secure hospital environment. The trials differed by geography, provider of thrombolysis (paramedic or doctor), thrombolytic agent and entry criteria, yet all the trials consistently showed a reduction in time to treatment and in all-cause mortality (Morrison, 2000). Greater distances between patient and hospital resulted in greater advantage from PHT. The GREAT trial compared PHT given by GPs in rural north-east Scotland with thrombolysis given in hospital in Aberdeen. PHT was given 139 minutes ahead of in-hospital thrombolysis (IHT) and all-cause death was reduced by 49 % (13/163 (8.0 %) vs. 23/148 (15.5 %) (GREAT group, 1992). Most beneft was secured when patients were treated within two hours of onset of symptoms. There were few adverse advents prior to hospital admission. The four cardiac arrests that occurred on the way to hospital were all in placebo-treated patients.
The UK Government recognised the importance of rapid delivery of thrombolysis to patients with AMI in the National Service Framework (DH, 2000) and in 2000 the NHS Plan (DH, 2000) made a commitment to introduce PHT.
Primary PCI
Thrombolysis is convenient and easy to administer but has several important disadvantages. It may take over an hour from treatment to restore coronary artery patency and over 50 % of arteries do not recanalise at all (Percutaneous Coronary Intervention (ASSENT-4 PCI) Investigators, 2006). Many patients therefore get no benefit but are still exposed to the risks such as intracranial haemorrhage in 0.2-1 % (Califf et al, 1992). Reocclusion of the artery occurs commonly and in about 5 % of patients this results in reinfarction with associated poor outcome (Gibson et al, 2003). Mechanical reperfusion of occluded coronary arteries with angioplasty balloons and intracoronary stents avoids these problems. Coronary artery patency is achieved in up to 95 % of cases and the incidence of early reinfarction is about 1 % (Stone et al, 2002). During the 1990 s, many trials were conducted to investigate whether the potential advantages of primary PCI would be sufficient to benefit the population of patients with acute myocardial infarction despite the inevitable delay to treatment. The meta-analysis of 23 trials by Keeley et al confirmed that PPCI was superior to IHT with significant reduction in death, non-fatal MI and stroke (Keeley et al, 2003).
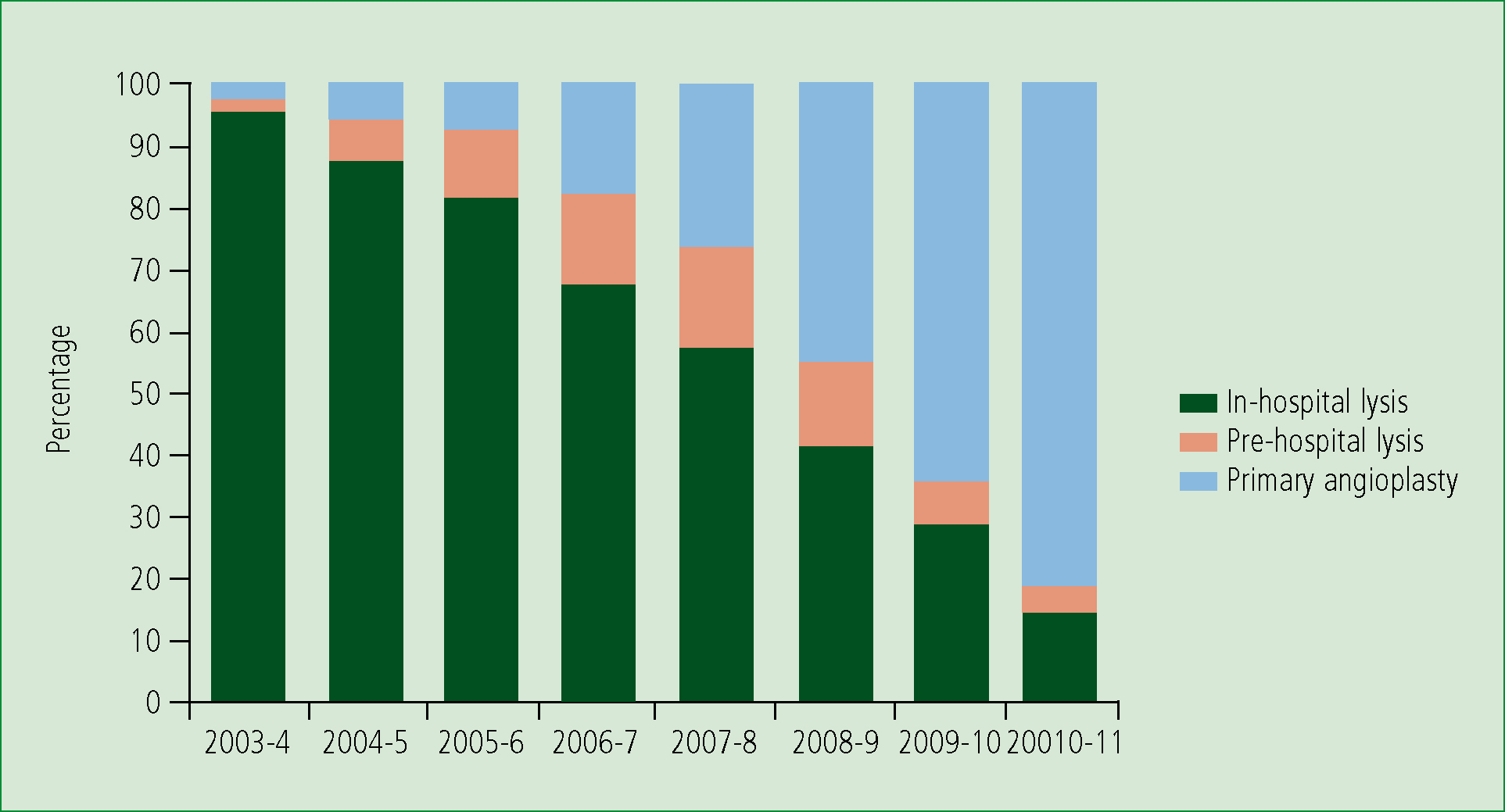
PPCI thus seemed preferable to thrombolysis and, despite the obvious costs required to set up a network of regional centres able to provide 24/7 angioplasty, in 2006 the UK government supported this development on the basis that it had the potential to save 500 lives and prevent 1 000 reinfarctions annually (Boyle and DH, 2006). The latest report from MINAP (Myocardial Ischaemia National Audit Project) (MINAP, 2011) shows that over 80 % of AMI patients suitable for reperfusion therapy are now treated by PPCI, while use of PHT has progressively declined since 2007–8 (Figure 4).
Is there a role for a combination of PPCI and thrombolysis?
Most patients with AMI do not find themselves within a few minutes of an open, staffed catheter laboratory. However, across Western Europe >80% of the population are within 30 minutes travel time to a PPCI centre (Widemsky, 2010). Traditionally, patients have been taken by the emergency services to the nearest hospital, most of which have not had emergency PCI capability, and there a sizable amount of people in rural north England and Scotland for example, that live long distances from any hospital. It seems possible that prompt thrombolysis followed by PCI as soon as it can be arranged afterwards might allow those 50 % patients who do recanalise the occluded artery with thrombolysis to get that advantage while guaranteeing the benefits of an open artery for the whole population with the safety net of emergency PCI.
Facilitated PCI
A generation of trials explored the so-called ‘pharmaco-invasive approach' to see if it could improve on the advantages of PCI. These trials used various combinations of thrombolytics, platelet glycoprotein IIb/IIIa inhibitors and timing intervals between thrombolysis and PCI. A meta-analysis in 2006 found that although those patients who received thrombolysis (n=3 867) were more likely to have normal coronary artery flow at angiography (37 % vs. 15 %) than the PPCI patients (n=3872), overall mortality (5 % vs. 3 %), nonfatal reinfarction (3 % vs. 2 %), major bleeding (7 % vs. 5 %), and haemorrhagic stroke (0.7 % vs. 0.1 %) all favoured PPCI (Keeley, 2006). At the same time ASSENT-4, the largest trial of facilitated-PCI was published (Assessment of the Safety and Efficacy of a New Treatment Strategy with Percutaneous Coronary Intervention (ASSENT-4 PCI) Investigators, 2006). This trial originally planned to enrol 4 000 patients but was stopped prematurely because of excess mortality in the facilitated-PCI arm. Patients were included if they had STEMI and PPCI was available within 1–3 hours of randomisation. After 1667 patients had been included a statistically significant difference in mortality (6 % vs. 4 %), very similar to that of the meta-analysis, was apparent. There may be good reasons why thrombolysis makes PCI more dangerous. The complication of major haemorrhage, especially from access sites, is inevitably increased when thrombolytics are administered before arterial puncture, and is associated with a bad prognosis in acute coronary syndromes (Eikelboom et al, 2006). When damaged myocardium is reperfused following PCI there may be more intramyocardial haemorrhage in the thrombolysed patient, leading to more frequent myocardial rupture (Moreno et al, 2002). Finally thrombolysis enhances platelet activity (Kawano et al, 1998), which may predispose to reinfarction in the facilitated-PCI patients. It may be that these potentially deleterious consequences of thrombolysis cancel the benefit obtained in the relatively small numbers of patients who reperfuse significantly in advance of the emergency angioplasty procedure.
Timing
All the above studies used IHT and enrolled patients within 6 hours of the onset of symptoms. Most did not present within the all-important first two hours (only 14 % in ASSENT-4 for example). In the thrombolysis vs. PPCI studies there was variable use of PCI after thrombolysis. Early use of PCI following thrombolysis has since been shown to improve outcome (Cantor et al, 2009) Is there a group of patients, presenting to the emergency services very early in the course of their myocardial infarction, who would benefi.t from immediate PHT? In CAPTIM, the one study of PHT vs. PPCI 55 % of patients were enrolled within two hours of symptom onset (Steg et al, 2003). Overall there was no difference in primary endpoint between the two arms of the study, but there was a strong trend towards reduction in mortality with PHT in those randomised <2 hours which was statistically significant at five years of follow up (Bonnefoy et al, 2009). Analysis of time intervals in large trials and registries suggest that overall PPCI remains advantageous over thrombolysis if the ‘PCI-related delay' i.e. the difference in time between possible delivery of thrombolysis and balloon inflation is under two hours (Boesma et al, 2006; Pinto et al, 2006) hence the current recommendation that PPCI is preferred if the patient can be delivered to the catheter laboratory in this time (DH, 2008). This recommendation for all-comers may not be best for some patients however. For younger patients, presenting earlier with anterior infarctions a PCI-related delay of over 60 minutes favours thrombolysis (Pinto et al, 2006). Should we be using different treatment strategies for different groups of patients with STEMI?
The case for the status quo
There is some evidence based on analysis of large registries and a small number of events in one RCT that a subpopulation of STEMI patients should be treated differently to the majority. Defining that subpopulation however is not straightforward. Paramedics are very good at recognising STE on a 12-lead ECG (Whitbread et al, 2002). The ability to recognise time of onset of myocardial infarction has not been tested and the reality is that it may be very difficult especially in the elderly (Bayer et al, 1986). Plaque instability precedes the onset of myocardial infarction by days or weeks (Rittersma et al, 2005) and 50 % of patients have prodromal symptoms prior to their infarct (Kouvaras and Bacoulas, 1987), which can be mistaken for onset of infarction. When we studied all the STEMI patients presenting to our hospital and receiving thrombolysis we found that, although PHT was available to all, only 36 % received it. The most common reason for this was that the patient history did not fit the criteria for thrombolysis, usually because prodromal symptoms had been mistakenly identified as time of onset of myocardial infarction (Smith et al, 2011). Criteria for paramedic PHT are necessarily conservative to avoid patients receiving this potentially dangerous treatment inappropriately. However, if a patient is taken to a PPCI centre inappropriately there is little danger of harm to the patient. There is another assessment before the patient receives any treatment by the doctors performing the angiography, and, when the ECG is difficult to interpret, by the result of the angiogram itself. In practice therefore it makes most sense to limit the diagnostic assessment of AMI to identification of ST elevation on the ECG and a binary determination of symptom onset, erring on the side of <12 hours if there is doubt. This can be done promptly and if appropriate the patient can be taken quickly to a heart attack centre for live-saving treatment.
Conclusion
PHT was good treatment. Many ambulance services embraced it and delivered it effectively. The skills that were developed are also required to identify patients for PPCI, an even better treatment. So although thrombolysis is now the reserve treatment, used when logistics prevent access to the catheter laboratory within two hours, it served a very useful purpose in the evolution of the treatment of AMI. In the last 10 years mortality from STEMI has declined every year, and PHT has played an important role in this success story.
There is still scope for further improvement to be made. Myocardial infarct patients with ECGs showing left bundle branch block and posterior myocardial infarction benefit from thrombolysis (FTT Collborative Group, 1994) and it is reasonable to assume would benefit from PPCI but are excluded in many PPCI protocols. ‘False-positive' STEMIs occur and drain resources. There are no published reports from UK hospitals but at least 10 % of patients presenting as STEMI to one US centre did not actually have this diagnosis (NforT et al, 2012).
The treatment of myocardial infarction has come along way since thrombolysis was first administered over 50 years ago. PPCI has been a great advance, but there is still progress to be made in ensuring the all the right patients are getting the right treatment.
