LEARNING OUTCOMES
After completing this module, the paramedic will be able to:
Directly translated from its Greek origins, the term anaesthesia means without sensation. (Yentis et al, 2009). In practical terms, the induction of general anaesthesia results in unconsciousness with the triad of amnesia, analgesia and muscle relaxation.
Local anaesthesia relates to the administration of a local anaesthetic drug directly to a body tissue or surrounding a sensory nerve supplying a particular area to result in a local loss of sensation and will not be discussed in detail in this article.
The provision of general anaesthesia to a patient can be divided into three stages: induction (starting to lose consciousness); maintenance; and emergence (return of consciousness). Anaesthesia can be induced and maintained by intravenous (IV) or inhalational agents or a combination of both.
In modern practice in adult patients who are receiving their anaesthetic in the operating theatre, induction of anaesthesia commonly occurs intravenously and is maintained by the continuous administration of inhalational volatile anaesthetic agents.
The provision of anaesthesia to a critically unwell patient outside the operating theatre differs in that IV drugs are used for both induction and maintenance for practical reasons.
Prehospital emergency anaesthesia (PHEA) of critically unwell or injured patients always starts with a rapid sequence induction (RSI) technique to promptly anaesthetise the patient and ensure that optimal conditions for intubation are achieved quickly. This technique was first described in 1970 by Stept and Safar, who aimed to reduce the risk of aspiration of stomach contents on induction by preoxygenation, rapidly administering a cocktail of medication that would produce anaesthesia and paralysis to provide favourable intubating conditions, and not applying positive pressure ventilation until a cuffed endotracheal tube (ETT) had been placed in the trachea.
Although the types of drugs used have changed the technique Stept and Safar (1970) described remains the basis for prehospital anaesthesia.
Indications for prehospital emergency anaesthesia
In current Irish paramedic practice, intubation is undertaken only by advanced paramedics in patients who are in cardiac arrest with no signs of life or in special circumstances and without pharmacological intervention (Pre-Hospital Emergency Care Council, 2018).
In patients who have intact reflexes, anaesthetic drugs are required to safely perform intubation. In Ireland, PHEA is provided by a small number of ambulance service doctors who respond at the request of EMS to provide enhanced prehospital care; however, in other jurisdictions, paramedics are permitted to perform PHEA (Delorenzo et al, 2018).
Based on the UK prehospital experience, PHEA is recognised as a procedure that is necessary in a relatively small number of patients and, if performed incorrectly, could result in unnecessary morbidity and mortality (Crewdson et al, 2019). In some cases, an experienced, PHEA-capable clinician may decide to defer the procedure until arrival at the emergency department where additional skilled anaesthesiology assistance is available.
The Association of Anaesthetists of Great Britain and Ireland (AAGBI) has published guidance on PHEA (Lockey et al, 2017). This states that PHEA should be undertaken as soon as required and to the same standards as in-hospital anaesthesia. The AAGBI also outlines the necessary competence, standards of equipment and monitoring, presence of a trained assistant and clinical governance structures that should be in place.
It should be noted that PHEA is a not a replacement for good-quality essential airway management and that a key aim in the prehospital care of the severely injured or critically ill patient is to ensure adequate oxygenation at all times by the means available at that time based on the skill set available.
Induction of anaesthesia and securing the airway is indicated in cases where: the patient's airway is obstructed and cannot be reliably managed using basic airway manoeuvres; there is an impending airway problem; the patient is obtunded due to a neurological insult or is intoxicated from alcohol and/or drugs and is unable to protect their own airway; there is ventilatory insufficiency with the inability to adequately oxygenate the patient despite the administration of high-concentration oxygen or to control the arterial partial pressure of carbon dioxide in traumatic brain injury; or for humanitarian reasons, e.g. to provide complete pain relief and amnesia (Luck and Morgan, 2019).
Practical aspects
The steps of prehospital emergency anaesthesia are best described by the six Ps mnemonic: preoxygenation; preparation; premedication; paralyse and sedate; passage of the ETT with proof of correct placement; and post-intubation care (Lowes et al, 2016).
Proper patient selection and preparation are key to success. Adequate patient access is required. Trapped patients will require extrication first and rarely is PHEA indicated in a confined space. Good-quality basic airway management should take place until the patient has been extricated or moved to a space that allows 360° degree access and has adequate light.
The preferred location to perform PHEA is with the patient placed on an ambulance trolley, with the trolley not loaded into the ambulance to allow 360° access to the patient and all equipment laid out next to the team (Luck and Morgan, 2019).
The aim of preoxygenation is to replace the nitrogen component of air in the lungs with oxygen; this maximises the available reservoir of oxygen, which helps to prolong the time it takes for the patient to desaturate during laryngoscopy and intubation. This is done by ensuring that the patient has a tight-fitting face mask with oxygen attached. Preferably this should be a Mapleson C circuit but a bag-valve mask device will suffice.
Ideally, a patient should be preoxygenated for 3 minutes or, if possible, instructed to take eight vital capacity breaths. During the preoxygenation phase, a patent airway is essential: if necessary, airway adjuncts—nasopharyngeal, oropharyngeal and manual airway manoeuvres—should be used (Benger et al, 2009).
In some patients, preoxygenation may prove difficult because of agitation resulting from brain injury, hypercapnia or other cause. In this situation, a pre-induction dose of a sedating drug can be administered; this is known as delayed sequence induction (Waack et al, 2018).
Preparation prior to PHEA involves rapidly repeating the ABCDE primary survey to detect any factors that indicate that airway management may be difficult. A life-threatening breathing problem, such as tension pneumothorax requires treatment before PHEA. Major haemorrhage should be controlled and the patient haemodynamically optimised before induction. Ideally, two IV cannulas with running fluid lines should be available. The intraosseous route is also suitable for the administration of anaesthetic drugs (Allman and Wilson, 2016).
A SAMPLE history (signs and symptoms; allergies; medications; pertinent medical history; last ins and outs; events) should be obtained with particular attention to drug allergies.
Anaesthetic drugs should be prepared and an equipment dump laid out with the vital signs monitor positioned in full view.
Drug preparation is an important task and should be performed only by a member of the team who is familiar with the conduct of PHEA and is competent in drawing medication from ampoules and vials into syringes. Some prehospital teams elect to pre-prepare anaesthetic drugs at the start of an operational shift. If this is the case, then syringes should be labelled, dated and capped and carried in a suitable container and comply with local organisation policy.
Cardiac arrest drugs should also be immediately available and include adrenaline 1:10 000, atropine and amiodarone, In addition, vasopressor drugs such as phenylephrine, ephedrine and metaraminol should also be available; these can be sourced in commercially prepared syringes or drawn from ampoules and stored in capped syringes. Any drugs that are drawn into syringes and capped should be disposed of at the end of the operational shift.
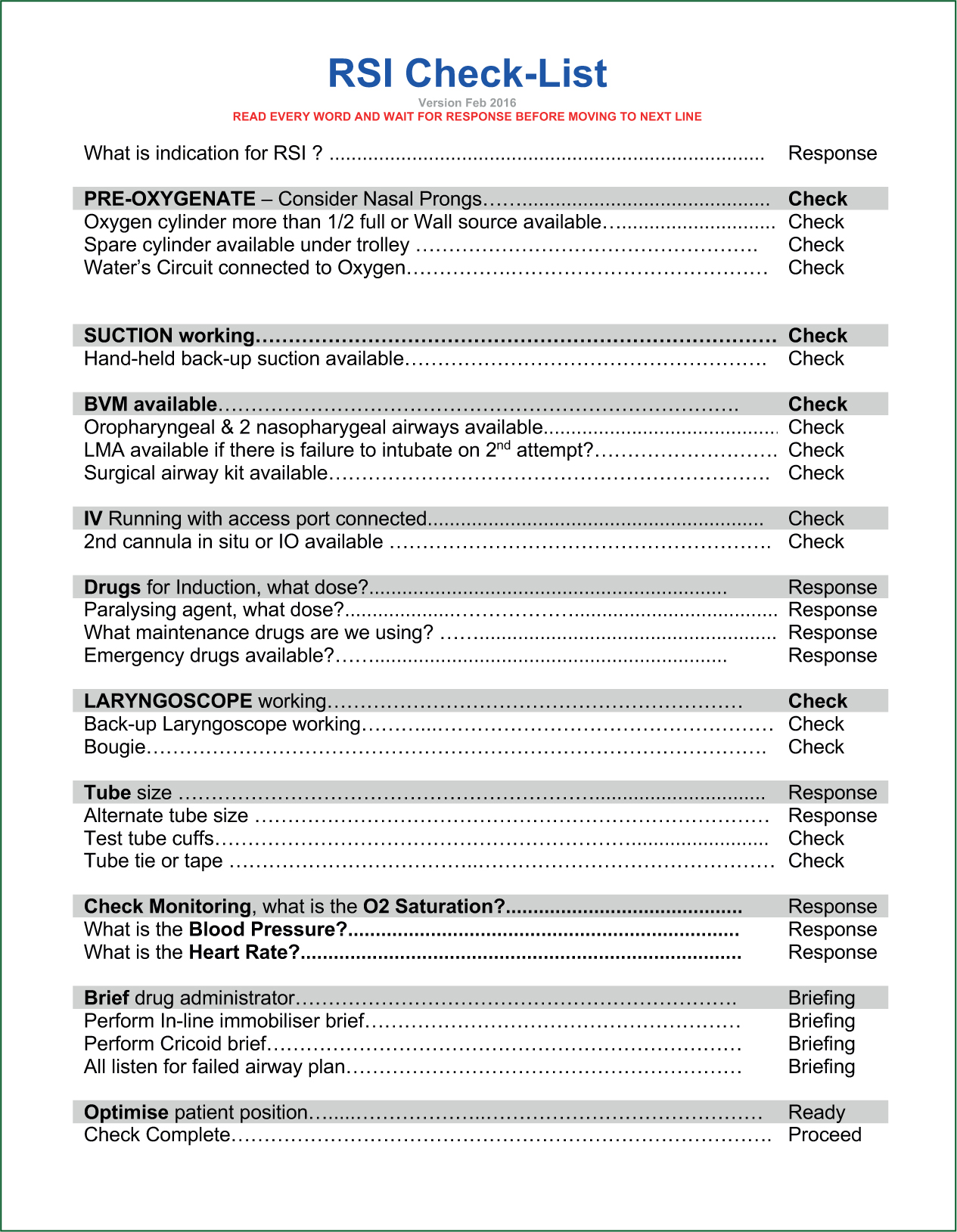
The pre-RSI checklist should now be completed in a ‘challenge and response style’ (Avery et al, 2021) (Figure 1). Correct use of a checklist requires that it is read verbatim by a team member and a response is required by the primary operator for each step before moving on. A failed-intubation plan should also be verbalised as part of the pre-RSI check list.
Drug choice for PHEA can vary, depending on the nature of the indication for anaesthesia and clinician preference. Many enhanced prehospital care teams in other jurisdictions standardise the choice of drugs available.
In general, a fast-acting opiate such as fentanyl is administered to blunt the physiological response to instrumentation of the airway. The dose of fentanyl can vary between 1 mcg/kg and 3 mcg/kg, depending on local guidance or clinical preference; this dose is generally reduced or omitted in patients who are haemodynamically compromised. Ketamine at a dose of 1–2 mg/kg (dose dependent on clinical scenario) is the most commonly used prehospital induction agent because of the haemodynamic stability it offers but propofol may be used judiciously in some patients.
A muscle relaxant is then administered. Suxamethonium or rocuronium are the only two muscle relaxants available that have a rapid onset of action (Lockey et al, 2014). Rocuronium has fewer contraindications and is becoming the drug of choice for RSI. Prefilled atropine and vasopressor drugs should be immediately available in the event of peri-induction bradycardia or hypotension.
As part of the pre-procedure brief, the clinical lead will decide on the type and dose of premedication, induction and muscle relaxant drugs to be administered.
The patient's position is optimised and they are preoxygenated as previously outlined. One team member will then administer all drugs in a rapid fashion followed by a flush of fluid. The time will be noted and laryngoscopy and intubation will occur after the patient has become apnoeic and muscle relaxation occurs. Classically, cricoid pressure would be applied on drug delivery and not released until the cuff on the ETT was inflated and the tube was confirmed to be in the trachea; however, this has become a controversial practice in recent years and is at the discretion of the lead clinician (Lockey et al, 2014).
After intubation, there should be a standard check for misting of the tube, the presence of symmetrical chest rise and air entry in conjunction with evidence of a capnography trace (ETCO2) consistent with ventilation. It is imperative that the ETT is secured and ETCO2 constantly monitored.
After intubation, the patient should be connected to a transport ventilator with suitable drugs available to maintain anaesthesia for the duration of transfer. Bolus doses of morphine and midazolam can be used to maintain anaesthesia.
Ideally the patient should be packaged in a vacuum mattress and environmental temperature loss minimised. It is imperative to understand that patients who have had PHEA have their protective reflexes removed and require constant monitoring.
Procedural complications
PHEA should be undertaken only after a risk versus benefit assessment has been carried out by a suitably qualified clinician.
The prehospital team may decide to continue with basic airway manoeuvres and defer the delivery of an emergency anaesthetic until arrival at the emergency department where additional assistance is available if it is felt the risk of the procedure outweighs its benefits. This may occur if it is anticipated the patient has a potentially difficult airway or transfer time to the emergency department is short. There are no hard and fast rules with regard to making this decision which is why PHEA should be performed only by a lead clinician who is experienced and supported by a team familiar with the procedure.
This also highlights the importance of a close link with hospital critical care/anaesthesiology departments and regular audit of PHEA cases and feedback to those involved (Crewdson et al, 2019).
The delivery of emergency anaesthesia is a high-stakes event and the importance of practitioners developing an understanding of human factors to minimise error has been recommended. The core components of human factors are teamwork, communication and situational awareness (Jones et al, 2018). PHEA carries the same risk as in-hospital emergency anaesthesia with the additional elements of a more challenging operational environment and limited resources, so a good working knowledge and appreciation of human factors is paramount. Paramedics who operate as part of a PHEA-competent team should receive human factors training (Lowes et al, 2016).
The main immediate complication to discuss is a failure of laryngoscopy to provide the operator with a clear view of the laryngeal opening. This could be because of local trauma distorting anatomical structures or poor positioning or other patient factors. It is imperative that an airway assessment is performed as part of the initial patient assessment to identify patient characteristics that increase the likelihood of difficult laryngoscopy and minimise the risk of a failure to intubate occurring.
A backup plan should always be discussed before induction and this usually involves using a supraglottic airway device as a means of rescue. Failing successful placement of a rescue airway and the inability to ventilate the patient using a bagvalve mask, an emergency cricothyroidotomy or front of neck access (FONA) is indicated. FONA is a surgical procedure that involves creating an incision in the cricothyroid membrane to gain access to the trachea and place an ETT. It should be noted that the main priority in a failed intubation attempt should be to ventilate the patient's lungs with high-concentration oxygen by whatever means possible (Higgs et al, 2018).
Because of the nature of the prehospital environment, tube migration or dislodgement is always a possibility. Continuous wave-form capnography and pulse oximetry should be monitored. A note of the depth the ETT was secured at should also be made. Tube migration will usually result in the ETT moving into the right main bronchus, which results in the left lung not being ventilated and high airway pressures occurring. Any loss in wave-form capnography or desaturation should prompt a return to the primary survey to examine whether the ETT is still secured at the appropriate depth, the chest is rising symmetrically, breath sounds are audible bilaterally and if there is any disconnection in the ventilator circuit between ventilation bag and ETT or ventilator and ETT.
Hypotension after intubation can occur for multiple reason. Regardless of the cause, it is well established that it worsens patient outcome if persistent (Sunde et al, 2017). It can result from undetected haemorrhage, secondary to the induction of anaesthesia or a switch from the physiological mode of negative pressure ventilation to artificial positive pressure ventilation. The cause of hypotension should be sought and management may include bolus of IV fluid or vasoactive drugs. (Benger et al, 2008).

