Supracondylar humeral fractures account for approximately 60% of all fractures at the elbow, and up to 13% of all paediatric fractures overall (Omid et al, 2008). They occur most commonly between the ages of 5 and 8 years when the capsule and ligaments around the elbow have been shown to have greater tensile strength than the bone itself, which is weaker due to extensive remodelling that occurs at this age.
This results in an increased likelihood of fracture of the more vulnerable bone in the supracondylar region when force is applied across it (Beals, 1976; Lins et al, 1999; Ogden, 2000). They are very rare after 15 years of age, due to skeletal maturity, and occur more commonly in males than females (Beals, 1976; Lins et al, 1999).
The most common mechanism of injury is landing on an outstretched hand as the child extends his/her arms to protect against a fall. This typically results in hyperextension of the elbow; allowing the olecranon to act as a fulcrum, causing an extension-type fracture in the supracondylar region, where the distal fragment is displaced and angulated posteriorly (John et al, 1996; Wu et al, 2002; Mangwani et al, 2006). This pattern of injury is seen in 98% of cases of all supracondylar fractures, while the flexion pattern is seen in 2% of patients.
Neurological injury occurs in approximately 15% of displaced supracondylar fractures, with the anterior interosseous branch of the median nerve being most at risk (Culp et al, 1990). Injuries to the radial and/ or ulnar nerve have also been reported with up to 15% incidence. Vascular injuries involving the brachial artery may also occur in up to 15% of displaced fractures (Gosens and Bongers, 2003; Robb, 2009). Forearm compartment syndrome, resulting in Volkmann's ischaemic contracture (permanent flexion contracture of the fingers, hand and wrist) occurs in less than 1% of cases.
Elbow stiffness and non-union following supracondylar fractures are rare in children (Rockwood et al, 2006). However, malunion and bone growth abnormality can occur, leading to progressive deformities. Cubitus varus or ‘gunstock deformity’, in which the elbow is bent with the forearm pointing towards the midline of the body, is the most common deformity. In a series of 206 patients with supracondylar humeral fractures, aged between 1.5 to 14 years, the incidence of cubitus varus deformities varied from 1.9% in those treated with pin fixation, to 7.9% after cast immobilization (Pirone et al, 1988).
The key to prevention is to achieve and maintain anatomical reduction (Rockwood et al, 2006). Although cubitus varus is essentially benign, corrective osteotomies are offered to those with cosmetic concern (Lins et al, 1999).
Accurate prehospital assessment and treatment of suspected supracondylar fractures influence hospital management and therefore patient outcomes. This article aims to refine assessment techniques for the neurovascular status in suspected supracondylar fracture; review analgesic options en route to hospital; and evaluate various splinting methods within the constraints of the prehospital setting.
Methods and results
A literature search was performed using PubMed and CINAHL Plus®. Key words searched included: ‘paediatrics’, ‘supracondylar fracture’, ‘humeral fracture’, ‘elbow fracture’, ‘compartment syndrome’, ‘cubitus varus deformity’, ‘Volkmann ischaemic contracture’, ‘intranasal fentanyl’, ‘inhaled methoxyflurane’, ‘entonox’, ‘air splint’, ‘pneumatic splint’, ‘inflatable splint’, ‘SAM splint’, ‘plaster of Paris backslab’, and ‘fiberglass slab’. The resulting articles provided background for further manual literature searches. Eighty-five articles were reviewed, and 34 of these are referenced.
Websites for the American Academy of Orthopaedic Surgeons (AAOS), the American Academy of Pediatrics (AAP), and the Paramedics Australasia (PA) were searched for consensus guidelines or policy statements regarding prehospital management of paediatric orthopaedic trauma; no records were found.
The literature on the clinical assessment and treatment of paediatric supracondylar fractures is largely based on case reports and anecdotal evidence. Several retrospective studies have been instrumental in appraising the efficacy of different analgesics in the paediatric emergency setting. A small number of human experimental studies have evaluated the use of inflatable splints in general.
Clinical assessment
Inspection—‘look’
The anterior and posterior aspect of the arm should be carefully inspected for any open wound, marked swelling about the elbow or bruising over the antero-medial aspect of the forearm, which may indicate brachial artery injury.
Any signs of a severely displaced fracture and/or neurovascular injury should be sought, and their presence indicates the need for urgent orthopaedic intervention. These include:
Palpation—‘feel’
Both hands should be palpated simultaneously for temperature and presence of a radial pulse. If the radial pulse is weak or absent, vascularity of the hand should be thoroughly assessed. If available, a handheld Doppler ultrasound may be used to detect an audible radial pulse if it is not physically palpable. The fingertips should be tested for distal perfusion using capillary refill, noting any delay.
A pulse oximeter with a paediatric probe can be used on the affected hand to further evaluate collateral circulation. A poor waveform or low oxygen saturation may indicate poor collateral arterial supply after a ruptured or entrapped brachial artery. If this is the case, the receiving hospital's surgical team should be alerted to the arrival of the patient and be prepared to explore and repair or reconstruct the brachial artery, after reducing and pinning the fracture.
‘Any signs of a severely displaced fracture and/or neurovascular injury should be sought, and their presence indicates the need for urgent orthopaedic intervention’
Neurological assessment—‘move’
Testing for specific peripheral nerve injuries should be performed by examining active movements of the fingers without disturbing the forearm and elbow to minimize pain and increase accuracy. The normal limb should be briefly examined first to ensure the child's understanding and compliance with the movements required. The screening tests (Figure 1) are:
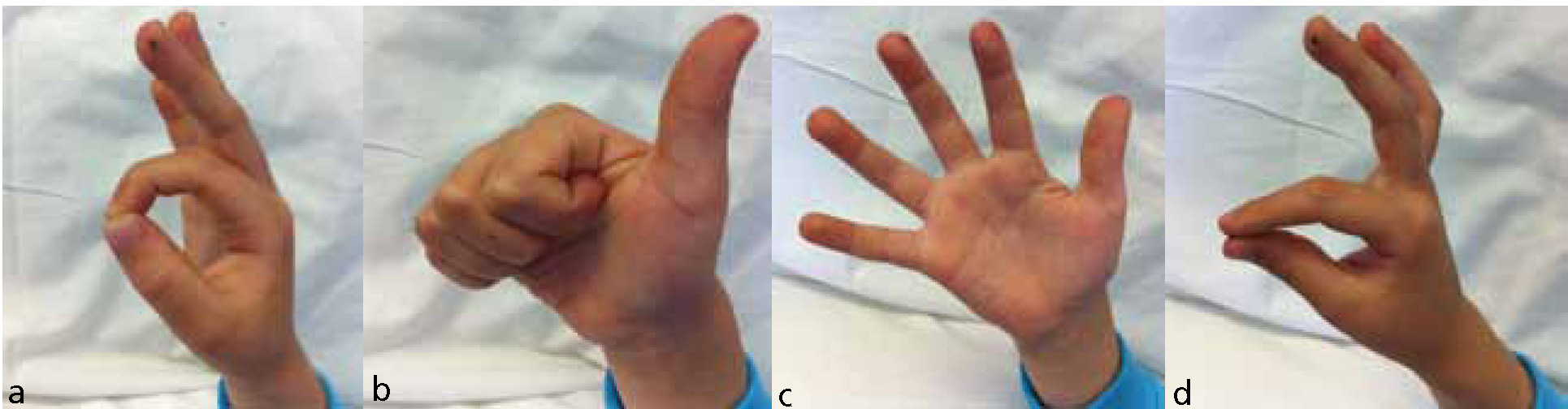
Particular attention should be paid to ensure the child is able to flex the distal inter-phalangeal joint of the index finger and thumb when doing the ‘okay sign’. The inability to do so is indicative of anterior interosseous nerve dysfunction. The presence of abnormalities of any of these active movements should be clearly documented and reported to the emergency department (ED) staff.
Sensation should be grossly examined using light touch. Each of the main nerves in the arm should be tested:
The child should be asked if there is any difference in sensation in any of these areas compared to the unaffected limb.
Finally, when the diagnosis is not made obvious by gross deformity and swelling, gentle palpation for tenderness is useful for ascertaining the exact location of the injury. However, where there is an obviously displaced fracture, palpation for tenderness is contraindicated as this will cause unnecessary pain.
Analgesia
Ideally, children with suspected supracondylar fractures should be given parenteral analgesia, rather than oral analgesia, in view of the possibility for urgent surgical intervention requiring general anaesthesia. Available options include intramuscular or intravenous morphine, inhalational methoxyflurane and intranasal fentanyl.
Morphine
Morphine is a potent narcotic agent which has been in use since the 19th century. It is administered through various routes and has a relatively short half life. Parenteral morphine provides safe and effective analgesia in children, both in emergency department and prehospital settings (Borland et al, 2007; Bendall et al, 2011). Contraindications to morphine include known hypersensitivity to opioids, acute or severe bronchial asthma or other obstructive or restrictive airway disease, renal impairment, heart failure, and head injury with severe central nervous system depression (MIMS online, 2011). Important side-effects include respiratory depression and hypotension, which are dose-related.
Avoiding the intramuscular route
In general, the intramuscular route is avoided in children because of the pain caused by the injection, delayed drug absorption with variable bioavailability, and inability to titrate the dosage of the drug (Fleisher and Ludwig, 2010). On the other hand, the intravenous route allows titration of the drug. However, it is often difficult to secure immediate intravenous access in children. Moreover, in Victoria (Australia), only specially trained paramedics such as mobile intensive care ambulance (MICA) paramedics are accredited to perform intravenous cannulation in children.
Methoxyflurane
Methoxyflurane first entered the market in 1962 as penthrane inhalation liquid, 99.9% (Abbott Laboratories, USA). However, due to its association with ‘serious, irreversible, and even fatal nephrotoxicity and hepatotoxicity in humans’, its approval by Federal Drug Administration (FDA) was withdrawn and its sale discontinued in 2005 in the US (FDA, 2005).
In Australia, inhaled methoxyflurane (e.g. penthrox inhalation, Medical Developments International Ltd, Springvale, Australia) is still widely used in the prehospital setting and is preferred by many paramedics. It is administered via a tubular, lightweight, handheld inhaler, whereby 3 ml of methoxyflurane is poured onto an internal wick, from which the child inhales. Typically, the inhaler dispenses vapour concentrations ranging from 0.2-0.7%. A maximum of 6 ml/day is recommended by the manufacturer. It is contraindicated in those with pre-existing renal impairment or renal failure, heart failure, respiratory depression and head injury or loss of consciousness (Medical Developments International, 2011). It should be used with caution in those with known liver damage or diabetes, and under treatment with enzyme-inducing drugs such as barbiturates.
Common adverse effects of methoxyflurane include nausea, vomiting, dizziness, headache, cough and retrograde amnesia. Onset of analgesia is expected to occur within 3-4 minutes of constant inhalation at a normal respiratory rate and tidal volume.
Intranasal fentanyl
The efficacy of inhalational analgesics depends on established coordination between perception of pain and the conscious decision to inhale with effective inspiratory effort—which may not be the most appropriate method of administration in young children who are distressed, crying and non-compliant.
The use of intranasal fentanyl in children with trauma is gaining popularity among health professionals. The recommended strength of intranasal fentanyl solution is 100 mcg/2 ml, which is drawn up into the syringe at doses between 0.75 mg/kg and 1.5 mcg/kg. With the patient sitting up at 45 degrees or with the head to one side, it is administered via a mucosal atomizing device (e.g. MAD300, LMA North America, Inc. San Diego, USA), dividing the dose between nostrils. It is contraindicated in those with known hypersensitivity to fentanyl, altered conscious state, bilateral occluded nasal passage and epistaxis (Royal Childrens Hospital (RCH) Clinical Practice Guidelines (CPG), 2011). Onset of analgesia occurs within 4-5 minutes of administration.
Intranasal fentanyl and intravenous morphine have been shown to be superior to inhaled methoxyflurane in relieving pain. A recent retrospective comparative study conducted in New South Wales, Australia, evaluated the effectiveness of intravenous morphine, intranasal fentanyl, and inhaled methoxyflurane in 3312 paediatric patients aged between 5 and 15 years with moderate to severe pain (76% of subjects with trauma), in the prehospital setting. ‘Effective analgesia’, defined as a reduction in pain score of ≥30% using the 11-point verbal numerical rating score (VNRS-11) was achieved in the majority of patients. However, intranasal fentanyl and intravenous morphine were shown to be more effective than inhaled methoxyflurane (87.5, 89.5, and 78.3% for morphine, fentanyl, and methoxyflurane, respectively). There was no statistical difference between intranasal fentanyl and intravenous morphine (OR 1.22; 95% CI 0.74-2.01) (Bendall et al, 2011).
The use of intranasal fentanyl in children appears to be safe as demonstrated in several small studies. A prospective study of 46 children aged 1-3 years presenting to ED with moderate to severe pain as a result of trauma (fracture in 39%), demonstrated that intranasal fentanyl, administered at 1.5 mcg/kg, was effective, safe and well-tolerated (Cole et al, 2009). Another observational study found that intranasal fentanyl administered at a median dose of 1.5 mcg/kg to forty-five children aged 3-12 years with fractures in ED, achieved early and significant reduction in pain without affecting vital signs and oxygen saturations (Borland et al, 2002).
Intranasal fentanyl is also shown to be as effective as intravenous morphine (at 0.1 mg/kg) with no serious adverse events when delivered at a dose of 1.7 mcg/kg in children aged 7-15 years with acute fracture (Borland et al, 2007).
A higher single dose of intranasal fentanyl at 2 mcg/kg (maximum 100 mcg) provided safe and satisfactory analgesic coverage up to 30 minutes in children aged 3-18 years with orthopaedic trauma (Saunders et al, 2010).
Given its efficacy, safety and ease of administration, intranasal fentanyl may be considered the ideal choice of analgesia in the prehospital setting for children with suspected supracondylar fracture, especially those in moderate to severe pain and non-compliant with inhalational methoxyflurane. The recommended initial dose is 1.5 mcg/kg. A second dose (0.751.5 mcg/kg) may be administered 10 minutes after the first dose as required.
‘Intranasal fentanyl and intravenous morphine have been shown to be superior to inhaled methoxyflurane in relieving pain’
Entonox
Entonox (containing 50% nitrous oxide and 50% oxygen) has been widely used by paramedics in the UK (not in Australia) as a method of analgesia in the prehospital setting since 1969. Its advantages are that it provides good analgesia, while being relatively safe. As is the case with inhaled methoxyflurane, compliance in the paediatric population relies on a child being cooperative. There have been no studies directly comparing the effectiveness of intranasal fentanyl and nitrous oxide for analgesia in significant trauma, such as supracondylar fractures, in the prehospital setting.
Immobilization
Immobilization of the affected limb serves both to limit further damage to the neurovascular structures at risk in a fracture, and also to alleviate pain. It may prevent conversion of a closed fracture to an open fracture by stabilizing fractured bone fragments. In paediatric supracondylar fractures, the affected limb should be splinted in a position that is comfortable for the patient, while avoiding flexion beyond 40 degrees (Omid et al, 2008) to limit swelling and deformity, and risks to other structures of the arm.
The different modes of splinting currently available to the paramedics include air-splints or inflatable splints, wooden splints and SAM (structural aluminium malleable) splints (e.g. SAM® Splint; SAM Medical Products, USA). Each method of splinting has its advantages and disadvantages.
Inflatable-splints are widely used by paramedics mainly as they are easy to apply and are radiolucent. The first described use of inflatable splints was recorded in 1944 (Curry, 1944). Since then, a number of human studies have demonstrated potential harm in using inflatable splints when applied to both upper and lower limbs for a prolonged period of time or when applied too tightly (Ashton, 1966; Sloan and Dove, 1984; Christensen et al, 1986).
The maximum safe pressure stated by some manufacturers is 30-40 mmHg. However, this pressure has been shown to be deleterious to the limb, due to direct transmission of pressure to the deeper tissues including arteries and osteofascial compartment, resulting in reduced blood flow and tissue perfusion (Ashton, 1966; Christensen et al, 1986). This phenomenon can take effect within one to two minutes of application (Ashton, 1966), and may be worsened by elevating the limb above the level of the heart, which is often done in an attempt to minimize associated swelling (Ashton, 1966; Christensen et al, 1986).
Some studies recommend the safest maximum splinting pressure of 15 mmHg (Christensen et al, 1986) while pressures below 10 mmHg have been shown to provide ineffective splinting (Sloan and Dove, 1984). Although it would be difficult to achieve pressures between such a narrow range (10-15 mmHg), since the majority of inflatable splints do not have pressure gauges or blow-off valves.
‘Immobilization of the affected limb serves both to limit further damage to the neurovascular structures at risk in a fracture and also to aleviate pain’
In addition, the methods used by paramedics to estimate the splinting pressures, are namely:
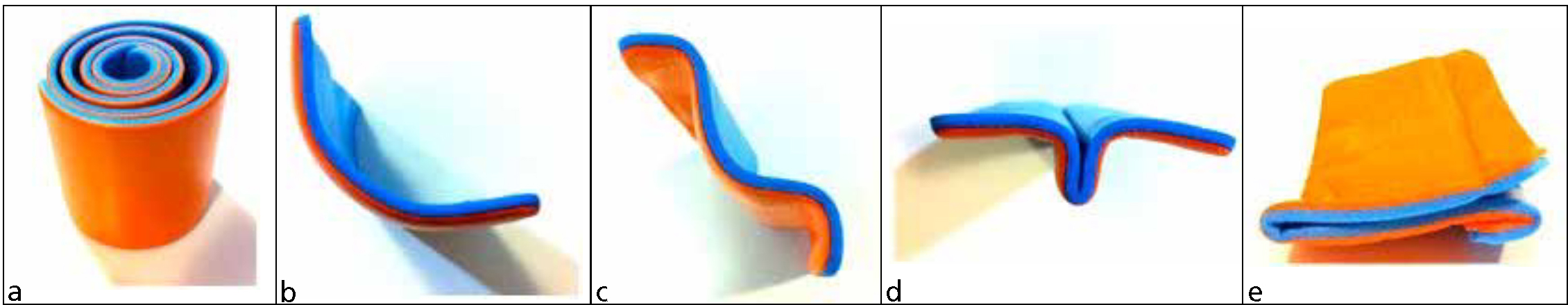
An alternative method of immobilization is the SAM splint which was invented in 1985 by Dr Sam Scheinberg, an orthopaedic surgeon. It is made with a thin core of aluminium alloy, sandwiched between two layers of closed-cell foam. The SAM splint is extremely light, flexible, waterproof, relatively radiolucent, easily mouldable, removable, and reusable. It is unaffected by extreme temperatures, humidity or altitudes, and is easily stored and portable. For these reasons, it would appear that the SAM splint is preferable to the inflatable splint. It should be noted that, at the time of publication, Ambulance Victoria is phasing out the use of inflatable splints.
Fibreglass and plaster of Paris are generally used for the longer term stabilization of a fracture. Plaster of Paris is cumbersome to prepare in the prehospital setting as it requires a bucket of water and takes a long time (minutes) to set. Fibreglass slabs (e.g. Dynacast Prelude, Smith and Nephew, England) are light, relatively radiolucent, and simple and can be applied quickly by the paramedics. Once set, it attains considerable strength hence stability. Although there have been no studies into the efficacy of using a fibreglass slab for immobilization in the prehospital setting, the authors feel that it is a viable option. Disadvantages of the fibreglass slab include high cost, susceptibility to spoilage in extreme weather conditions (e.g. high humidity, intense sunlight), and limited shelf life while in storage.
Hospital management
Definitive treatment of supracondylar fractures depends on the direction and amount of displacement of the fracture, as per the Gartland radiographic classification.
Gartland type I fractures are described as undisplaced or minimally displaced, with the anterior humeral line still passing through the ossified capitellum. Gartland type II fractures are partially displaced, with posterior angulation and hinged posterior cortex. Gartland type III fractures have complete displacement of the distal humeral fragment with no cortical contact Flynn, 2011).
Overall goals of definitive treatment are to obtain anatomical reduction and to maintain reduction until union.
Gartland type I fractures are generally treated non-operatively with immobilization, with the elbow flexed at 90° and forearm in the neutral position. This is typically achieved in a collar and cuff or above-elbow posterior slab, with an arm sling for 3-4 weeks. A randomized controlled trial (Oakley et al, 2009) showed immobilization in an above-elbow posterior fibreglass slab was superior to collar and cuff, achieving faster return of function (2.0 days vs 7.0 days, P=0.01).
Gartland type II fractures require closed reduction, preferably under general anaesthesia in the operating theatre with the use of an image intensifier, so that the alignment of the fracture can be ascertained in real-time while in theatre ensuring that the child has to undergo only one general anaesthetic (Simanovsky et al, 2007). At times, wire fixation may be necessary. If theatre is not readily available, manipulation can be performed in ED with intravenous sedation and analgesia.
The management of Gartland type III fractures continues to evolve with emerging evidence. Treatment options include closed reduction with immobilization with plaster slabs or K-wire fixation, open reduction and internal fixation with K-wires, and straight arm traction, depending on the degree of associated swelling, neurovascular deficit and time of presentation.
Currently, no consensus exists for the management of the pink pulseless hand associated with supracondylar humeral fractures (Allen et al, 2010). Some may opt to closely monitor the neurovascular status of the affected limb over the next 48 hours, while others may choose a more aggressive approach with early exploration of the brachial artery if the pulse does not return after reduction.
However, if left untreated, vascular injuries associated with supracondylar fractures may be complicated by the emergence of compartment syndromes, with subsequent ischaemia of the forearm and hand musculature, giving rise to Volkmann ischaemic contracture.
Prognosis
Supracondylar humeral fractures in children have a high rate of good functional outcomes. Two retrospective studies have reviewed return of range of motion of the elbow post-injury with similar impressive results. In one study, after closed reduction and percutaneous pinning of displaced supracondylar fracture, the average return of range of motion was 86% at 3 months and 94% at 6 months (Zionts et al, 2009). In another study, a return of range of motion of 90% was recorded at 6-7 weeks after removal of cast/wires from the elbow (Wang et al, 2009).
Conclusion
Supracondylar humeral fractures are one of the more common paediatric fractures. The principal goals of prehospital management of paediatric supracondylar fractures are rapid neurovascular assessment, administration of adequate and effective analgesia, and stabilization of the affected extremity with appropriate splinting. Prompt and accurate assessment, especially when there is neurovascular compromise, is important to facilitate prompt ED diagnosis and ultimately orthopaedic intervention, where required, to ensure good outcomes.
