The Scottish Government's strategic goals describe a new ethos for health in Scotland that sees people at the heart of a ‘mutual’ NHS (Scottish Government, 2007). ‘Delivering for Health’, an earlier report from the then Scottish Executive highlighted self-care support as a key priority, which is part of a wider framework aimed at improving health and well-being (Scottish Executive, 2005a).
The social and economic impact of ill health can be significant. The Scottish Association for Mental Health looked at the high costs of mental health problems. Their research showed that in 2005, these costs were equivalent to £8.6 billion, around 9% of Scotland's gross domestic product (Scottish Association for Mental Health, 2006).
Self-care is both an ethos and a set of techniques that health care professionals (HCPs) can employ to support people in their efforts to self-care better. There appears to be a growing enthusiasm for support of self-care among health boards and other organizations in Scotland. How has this come about? This article will describe what self-care is, its origins, whether the current literature provides an answer to the current enthusiasm for it, what is missing from the research and whether paramedics can effectively support the self-care agenda.
What is self-care?
Self-care can be described as:
‘whatpeople do to maintain their health, prevent illness, seek treatment or support, manage symptoms of illness and side effects of treatment, accomplish recovery and rehabilitation and manage the impact of chronic illness and disability on their lives and independence’ (Alliance for Self-Care Research, 2006).
Or:
the ‘actions people take for themselves, their children and their families to stay fit and maintain good physical and mental health’ (Department of Health (DH), 2005a).
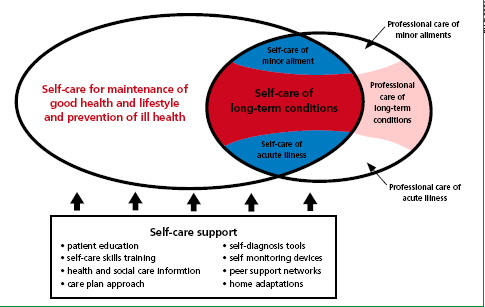
Figure 1 shows the links between self-care and professional care. Self-care includes managing minor aliments and minor injuries, but perhaps the greatest potential for self-care, is likely to be in the context of the management of long-term conditions (Scottish Executive, 2005b). This is an area where paramedic support for self-care is also likely to be of greatest benefit (in reducing hospitalizations and improving self-care awareness).
The origins of self-care
A key theory proposing a change from simply managing the biological illness to a more holistic approach was the ‘biopsychosocial model’ described by George Engel (Box 1). Engel (1977) suggested that to treat the person purely from the biological point of view was reductionist and that health professionals needed to treat patients more holistically. Later research by Albert Bandura (1995) found that successful self-regulatory change programmes had included the installation of beliefs about personal self-efficacy at every stage and that people who have a strong belief in their self-efficacy tend to regard a slip as a temporary setback. Bandura states that there are four elements to successful self-directed change: informational, development of self-regulatory skills, building a robust sense of efficacy, and enlisting and creating social supports.
Many NHS policy documents regarding self-care published in recent years suggest similar core elements (Wanless, 2002; Scottish Executive, 2003; DH, 2005a; Scottish Executive, 2005b; Scottish Executive, 2005c; Scottish Government, 2007; Scottish Government, 2010). This suggests that health and social policy makers are using grounded theory in their promotion of self-care support. Later work by Coulter (2007a; 2007b) concluded that building self-efficacy is a key element of building capacity to self-care.
The main drivers promoting self-care
Current literature suggests there are two key theoretical change models: the deficit model and the self-determination model. The deficit model suggests that the NHS is too expensive and we need to find more efficient ways of working. It also suggests that current care is not working, leading to unnecessarily high levels of GP, primary care and A&E attendances. This exacerbates the spiralling cost to the NHS. The self-determination model suggests that people are keen and ready to self-care, and that there is professional willingness and support to do so.
There is evidence supporting this (DH, 2005b). However, the deficit model seems to form the greater part of current Government and NHS policy (Scottish Executive, 2003; DH, 2005a; Scottish Executive, 2005b; Scottish Executive, 2005c; Scottish Government, 2007; Scottish Government, 2010). There are references to ‘efficient’ use of resources in most of these papers but they largely steer away from using terminology relating to financial cost such as ‘expensive’, mainly using this terminology to describe technologies or equipment.
This is perhaps so as not to lead to the conclusion that the main drivers behind changes in self-care support are financially driven. ‘Building a health service fit for the future’ (Scottish Executive, 2005b) is perhaps the clearest example of this general theme. This cites the financial burden to the NHS in Scotland as one of the main drivers for change, but follows the format described above in its careful use of terminology. For example, of the six instances of the word ‘expensive’, all but one relate to technology, laboratory equipment and in-patient diagnostic tests, the other to describe rural and remote factors.
Almost all of its eighteen uses of the word ‘efficient’ (or it's derivative) relate to processes, capacity, people, avoiding waste, referral systems, facilities, time-management and in-bed stays in hospital. Remote and rural factors are significant in Scotland. One fifth of the Scottish population live in a rural area (Scottish Executive, 2005b), and has greater need in terms of transport, access to services and information. Time spent in transportation to hospital and in attending patients in their homes can be significant. This can affect the ability of these key service providers to attend other patients.
Barriers to improving self-care skills
Living in deprived areas, employment, education, race, gender, sexuality, language barriers and age are all barriers to accessing self-care services and resources (DH, 2005a; Scottish Government, 2007, Alliance Scotland, 2008) and as such, are barriers to improving self-care skills. Access needs to be improved so that disadvantaged groups can access these services and improve their health literacy. Improving health literacy is a challenge and there are differing opinions as to how far health literacy can be promoted. The Expert Patients Programme's (EPP) main aim is to:
‘Establish the principle of individual self-management and self-care as a recognized public health measure’ (EPP, 2008)’
It delivers free courses for those with a recognized long-term condition. Despite being shown to be cost-effective, there are limitations to the EPP. Richardson et al (2008) found that people who lived in deprived areas showed less appeal for the programme. This is a challenge as this is one of the key groups the Scottish Government hopes to target with self-care support resources.
Why should we support it?
The current evidence supporting self-care greatly outweighs evidence to the contrary. This is clearly visible in the DH white paper ‘Research Evidence on the Effectiveness of Self-Care Support: Work in Progress’ (DH, 2007). This paper lists current research findings. It clearly shows research evidence demonstrating benefits vastly out-numbering those which do not. Perhaps more importantly, patients want it (Tompkins and Collins, 2006), and are keen to do more (DH, 2005b)—this fits with the Scottish Government's key strategic goals of putting patients at the heart of everything they do (Scottish Government, 2007). Consideration needs to be given to effectiveness and there is evidence which suggests that improvements in self-care skills are less likely the longer someone has had a condition (Astin et al, 2002), so support strategies need to take this into account.
Delivering support for long-term conditions is a strategic priority for the NHS (DH, 2005a). This is supported by Tompkins and Collins (2008) who suggest that ‘we need to fundamentally change the way we manage and support people with long-term conditions; we need to find another way to manage the demand’.
What is missing?
Children and young people are little mentioned in the current literature. Although a small percentage of the total patient numbers in the NHS, children are an important group—after all, they are our future adult population. Can NHS partnerships enhance self-care education in schools? Can community and school nursing teams deliver more healthy-eating, oral care and healthy lifestyle education? The current emphasis appears to be aimed at primary care teams in scheduled services. How are unscheduled care services and scheduled service providers going to ensure that they are supporting self-care strategies with the same ethos? Unscheduled carers see their patients for only short periods of time, and usually for episodic care. So there is a clear opportunity to research a ‘joined-up approach’ for both groups.
Little is mentioned in the current literature regarding how best to monitor the quality of the holistic elements of care plans. For example: could Quality Improvement Scotland have a role in auditing the quality of the holistic and empowering elements of care plans?
What are the implications for practice?
There is evidence to suggest that patients feel that their emotional and psychological needs are not met in encounters with health professionals, rather they mainly get this from family members or friends (Chambers et al, 2006). For practitioners involved in the care of patients, there is a clear need to embrace the principles of self-care. This means becoming a more holistic practitioner, being aware of the principles of the biopsychosocial model and putting these into practice.
Practitioners need to use empowerment and shared decision-making as much as possible and being aware of the benefits of goal-setting and cognitive behavioural therapy. Managers need to allow time and resources to provide training and support for self-care, with protected time for learning, exploring areas of possible funding and building partnerships with social support networks (Chambers et al, 2006).
Can paramedics support the self-care agenda?
Scotland has approximately two million people living with long-term conditions (Long Term Conditions Alliance Scotland (LTCAS), 2008). In 2005, around 3% of those over 65, who had a long-term condition, accounted for 35% of emergency and unplanned admissions (National Primary Care Research and Development Centre, 2006).
One long-term condition identified as a key challenge is chronic obstructive pulmonary disease (COPD). The most recent UK JRCALC guidelines describe COPD as ‘a chronic progressive disorder characterized by airway obstruction that does not change markedly over several months’ (JRCLAC, 2006). The World Health Organisation (WHO) (2001) has identified COPD as the fourth most common cause of death worldwide. Audit Scotland (2007) state that during the period 1997/8-2005/6 the inpatient and day case admission rates for COPD has increased by 25%, while rates for some other long-term conditions have fallen. This is significant as the report identifies that (if prevalence rates remain the same), the number of people with COPD will rise by 33% between 2007 and 2027. It therefore seems prudent to use COPD as an example of how paramedics can deliver support for self-care.
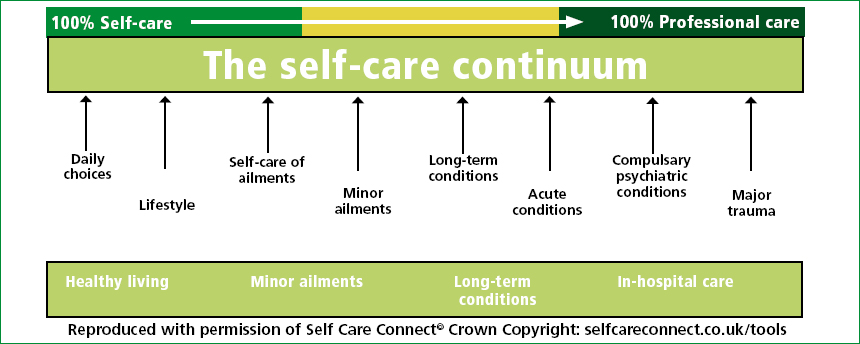
Paramedics generally meet individuals who have acute health needs (to the right of the health care continuum shown in Figure 2). This presents challenges around supporting self-care skills in terms of time and unfamiliarity with the patient. Even with these challenges, paramedics can help individuals develop self-care skills.
Paramedic recognition of patients requiring hospital admission has been called into question (Schmidt et al, 2000Hauswald, 2002; Silvestri et al, 2002). However, this evidence must be questioned when it comes to assessing whether today's UK paramedics are able to carry out assessment of patients safely.
A more recent, high quality study has concluded that paramedics with additional training can safely assess the need for hospital admission (Mason et al, 2008). The following is an example of how prehospital providers with additional skills can embrace the ethos of self-care support, encourage shared decision-making, improve self-efficacy and in turn improve general health and reduce hospital admissions.
An example
David is 58-years-old and lives alone since his wife died three years ago. He suffers from COPD, anxiety disorder and ischaemic heart disease. He lives in a first floor flat, does not take much to do with his neighbours and sees little of his son after a dispute with him after his wife's death. He now cannot do the things he enjoyed before such as gardening and socializing. He has refused re-housing a number of times, claiming that he would lose his independence. He has one care provider each evening to help him prepare a meal. He has refused further care as again he feels this would undermine his independence.
David uses home oxygen via nasal prongs delivered by a condenser. He calls 999 regularly because of breathlessness. He knows the ambulance crews by name and feels they provide him with reassurance and someone to talk to.
On the day in question, he called for an ambulance twice. When the crew arrived on the second occasion, he was feeding his budgerigar. The paramedic adopted the 5A's approach (assess, advise, agree, assist and arrange) which is endorsed by the WHO (2005) as a technique which can enhance holistic care. The paramedic's assessment had already started. He asked David if he would like to take a seat and asked what had been bothering him. David stated that he was worried that he was having an exacerbation of his COPD. The paramedic asked if anything else was bothering him and how this was making him feel. During his responses, the paramedic saw that David was anxious, but was speaking in long sentences.
‘Practitioners need to use empowerment and shared decision-making as much as possible and be aware of the benefits of goal-setting and cognitive behavioural therapy’
The paramedic asked him if he would agree to be examined. He found that David's heart rate, respiratory rate, lung sounds, tidal volume, oxygen saturation levels, temperature, skin colour, blood pressure and ECG were all within the expected range for him. During the assessment, he asked about David's family, neighbours and friends, how he felt about his adherence to medications and his use of oxygen.
David said that the oxygen tubing was too short as every time he goes into hospital the paramedics allow him to take a length of the tubing with him. This is because he prefers nasal prong delivery of oxygen. The shortened tube length means he has to take it off to get to his bathroom and kitchen. He said that he does stick to his medication regime most of the time. He is worried about what his neighbours think about the state of his garden and he wanted to get to the newsagent to get a paper to do the crossword he does every Saturday.
After describing what he has found during the physical exam, the paramedic offered David advice on medication use and in controlling breathing. He engaged him in an exercise in controlled breathing and kept the pulse oximeter on David's finger.
This assisted David to gain self-regulation skills by positive association with the improving oxygen saturation reading. He gave David some lengths of oxygen tubing to keep at home; this makes him feel less anxious. He offered to go the newsagent and return with his paper after the consultation had finished (I can hear ambulance service managers having a sharp intake of breath here- but read on, and then decide if this was a crucial part of an approach which led to the outcomes we all want to see). They discussed and agreed two action plans. One was designed to help David identify symptoms of anxiety and breathlessness and how to differentiate between the two. The other, a goal-setting strategy aimed at eventually allowing him to tend to a small section of his garden.
With David's agreement, he arranged for David's downstairs neighbour to get his paper for him the following Saturday. Also with David's agreement, he offered to speak with a contact he has in the local Social Services team with a view to arranging a visit from them to see how they might be able to assist further. He wrote a brief summary of the encounter with David in his care plan so as other service providers can see what had been discussed.
Afterwards, the paramedic liaised with social services and they arranged to visit David a few days later. The paramedic learnt that David has now accepted an enhanced care package. His neighbour now gets his newspaper each Saturday and cleans up David's garden. They have developed a good friendship and his neighbour checks on him regularly. He has had reduced hospital admissions and has not called an ambulance in two months. The paramedic carried out a reflective account of his encounter with David. He action planned for encounters with similar patients.
Managing the risk
‘There is no ideal risk assessment method or framework’ (Calder, 2002), but it is important to manage the risks associated with leaving people at home after calling for help from health care services. In these circumstances, risk management is really on risk reduction.
Paramedics can ensure the risks are reduced by ensuring their decision- making is sound and defensible, ensuring all decisions are recorded accurately, ensuring that the patient has no concerns about calling for help again, providing those contact details (telephone numbers etc.) to the patient and family members and ensuring that the patient recognizes what symptoms should alert them to call again. Agencies can ensure risks are reduced by ensuring that paramedics involved in these situations are properly trained and that this training is reinforced through regular updates, by regular audit of these patient encounters and by introducing a follow-up system where the patient is seen the next day, either by the same provider or by another care agency.
Conclusion
Support for self-care is gaining widespread support, not just in Government and the NHS in Scotland, but also among patients, patient groups, carers and support groups. The theoretical models underpinning support for self-care are grounded in widely accepted behavioural, social science, health and social care research. The evidence-base to support self-care is extensive despite occasional evidence questioning the success of self-care support strategies for some conditions and patient groups. This includes evidence of significant financial benefits. There are challenges around delivering a ‘joined-up’ approach, particularly with regard to time, resources and training.
Training should be directly linked to the knowledge and skills framework. This would ensure manager ‘buy-in’ and support. Currently, paramedic care is predominantly guideline driven and focuses on the current symptoms or complaint. A paternalistic approach is necessary in some cases, but practice for many other consultations can develop to embrace the principles of the biopsychosocial model.
Paramedics can use easy-to-learn tools such as the 5As approach to enhance shared decision-making and improve the holistic content of their consultations. It is vital that the good work in supporting self-care by scheduled services is not undermined by unscheduled care providers working from a differing ethos. Self-care awareness training must include unscheduled care providers. If changes in practice do not occur then parts of the NHS in Scotland are likely to continue to treat patients on an episodic basis and waste valuable resources.
