This 58-year-old man lives in a remote and rural area and presents with central chest pain.
He normally keeps fit and well and has no pertinent medical history. He was out for his usual morning jog. He had run for several miles when he became acutely unwell. He had developed a heavy, pressing central chest pain that radiated into his jaws and down both arms. The pain was severe and he rated it as 9 out of 10. He vomited several times. He managed to return to his car and drove himself home. However, he continued to feel very unwell and called for an ambulance. He suspected he was having a heart attack.
His vital signs were as follows:
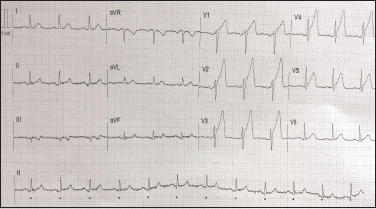
The 12-lead electrocardiogram (ECG) in Figure 1 was recorded.
Interpretation of the ECG rhythm
There is ST segment elevation of approximately 5mm across his chest leads V1–V5. There is no T wave inversion or pathological Q waves. This suggests a hyperacute anterior septal ST elevation myocardial infarction (STEMI).
Coronary angiography revealed an occluded proximal left anterior descending coronary artery. A single stent was inserted. He went on to make an uneventful recovery.


