An 89-year-old lady has lived in a care home for the last 3 years. Up until then, she lived independently at home with daily input from her two daughters. She was diagnosed with dementia 5 years ago and her cognitive function deteriorated insidiously since then. She had made advance arrangements to go into care while she still had capacity to do so.
Her only other past medical history is of hypertension that is well controlled on medication, including a beta blocker.
Over the last few days, she has been feeling out of sorts. She has felt very lethargic and easily tired on minimal exertion. She has also developed shortness of breath, particularly when lying flat in her bed. Staff had noticed her to be more confused than usual.
Her vital signs were as follows:
There was no 12-lead electrocardiogram (ECG) machine in the care home. However, one of the senior nurses did have her own mobile ECG device to manage her atrial fibrillation. She recorded the ECG rhythm strip in Figure 1.
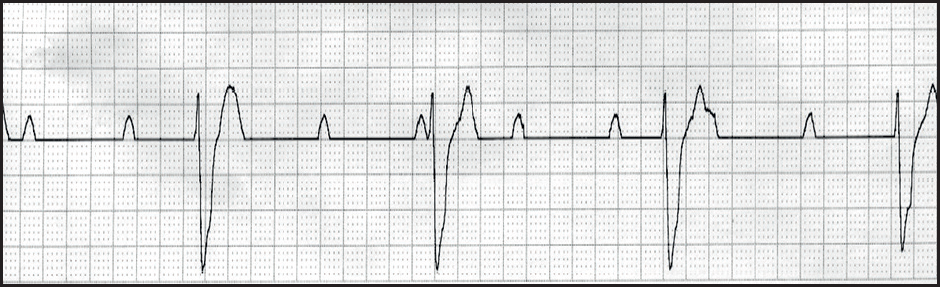
Interpretation of the ECG rhythm
In complete heart block, all atrial impulses are blocked at the atrioventricular (AV) node. Ventricular depolarisation may be maintained by an escape pacemaker. Nodal escape rhythms, originating above the bifurcation of the His bundle produce narrow QRS complexes, faster (>40 beats/minute) and reliable heart rates, and mild symptoms (for example, fatigue, postural light-headedness, effort intolerance). Ventricular escape rhythms, originating below the bifurcation produce wider QRS complexes, produce slower and unreliable heart rates, and more severe symptoms (such as presyncope, syncope, heart failure).
The lady was admitted to hospital and a permanent pacemaker was implanted the next day. She returned to the care home 24 hours later where she continues to do well.


