This 32-year-man presents with severe central chest pain. He has a long history of significant mental health issues and he smokes in excess of 60 cigarettes a day.
He has been experiencing intermittent chest pain for 2 days. However, this morning, it has become more severe. He describes it as being aching in nature and located across the front of his chest. He rates it as 9 out of 10 in intensity. His arms feel heavy. He is also pale and sweaty.
There is significant family history with both his father and older brother diagnosed with coronary heart disease at a young age.
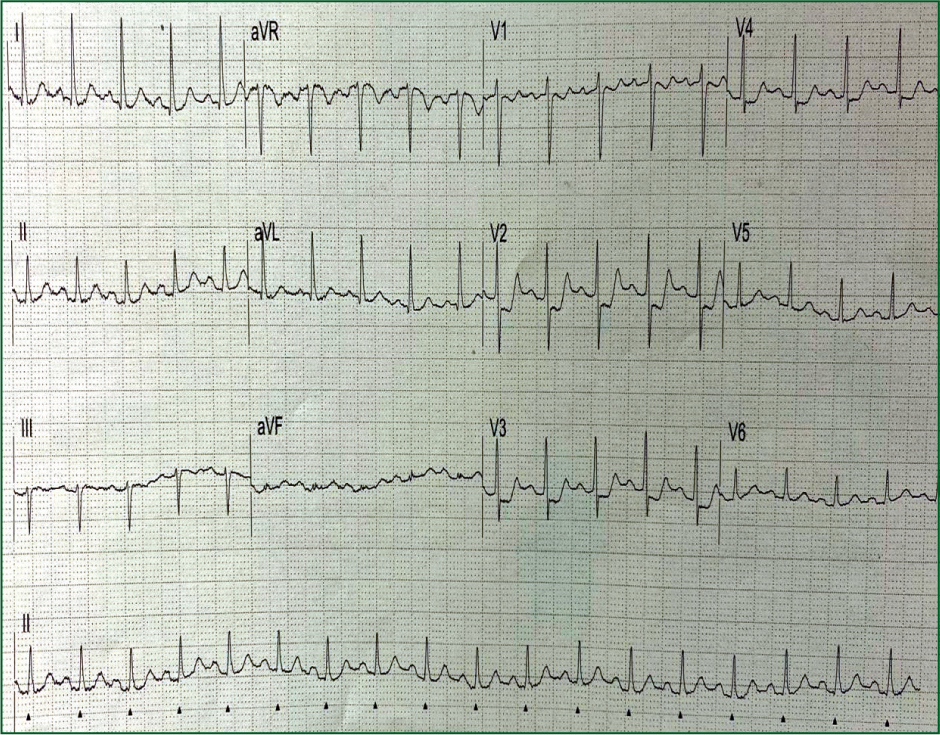
What does the ECG show?
Interpretation of the ECG rhythm
- The heart rhythm is regular and in sinus tachycardia
- The heart rate is approximately 105 beats per minute.
Interpretation of the 12-lead ECG
- The most striking abnormality is ST segment depression in leads V1–V4.
This man was triaged to the catheterisation laboratory (cath lab) for emergency primary percutaneous coronary intervention (PCI) with a likely diagnosis of acute posterior myocardial infarction (MI). He was found to have an occluded proximal circumflex coronary artery. A single drug-eluting stent was inserted.
An echocardiogram was recorded 48 hours later. It demonstrated akinesis of the posterior wall of the left ventricle. The ejection fraction was estimated at 45% (normal 50–60%)
Posterior myocardial Infarction
Around one in four patients with an acutely occluded coronary artery do not present with ST elevation. These acute ‘occlusive MI’ (OMI) patients do not meet the standard ST elevation criteria (mm) for primary PCI or coronary thrombolysis, however still need it.
A number of ECG patterns should be recognised as indicative of OMI:
- De Winters ECG
- Posterior MI
- Hyperacute T waves
- Aslanger's ECG.
Posterior MI is the most common ECG pattern of (OMI) without ST elevation, caused by circumflex or right coronary artery occlusion. It is often associated with inferolateral ST/T changes on the ECG. ST depression can be as low as 0.5 mm in V1–V3 and ST depression does not worsen towards V4–V6.


