This 76-year-old man has presented with severe central chest pain. He lives alone, having been widowed 6 years ago. He was pottering around his garden when he developed an ache in his chest that escalated into a severe pain within minutes. He became overwhelmed by a sense of fear. The pain was present across the front of his chest and radiated into his jaws and both upper arms. He vomited several times. He was grey and cool to touch. A neighbour called for an emergency ambulance.
His vital signs were as follows:
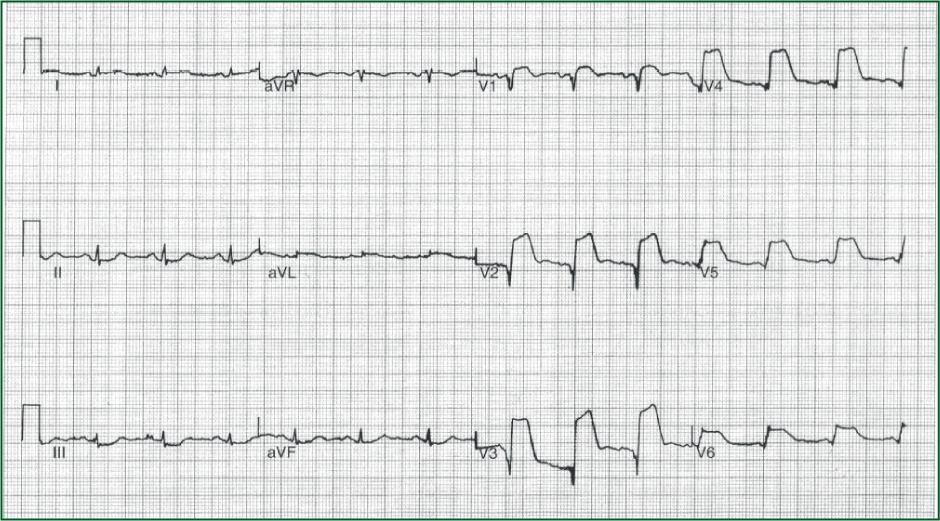
The 12-lead ECG in Figure 1 was recorded.
Interpretation of the ECG rhythm
There is ST segment elevation of up to 15 mm in V1–V6 suggestive of an extensive anterior lateral ST elevation myocardial infarction. There is ST segment depression in the inferior leads II, III and aVF.
The paramedics were preparing him for transfer to the catheterisation laboratory (cath lab) for primary percutaneous coronary intervention (PCI). He deteriorated further while they were preparing him for transfer and his pulse rate reduced to only 30 beats per minute. The ECG rhythm in Figure 2 was noted at this time.

Interpretation of the ECG rhythm
This is complete heart block (third-degree atrioventricular block) with a ventricular escape rhythm.
Complete heart block in the context of an anterior myocardial infarction is usually due to occlusion of the left anterior descending coronary artery resulting in septal necrosis and infarction of bundle branches. The complete heart block usually develops abruptly. The escape rhythm is unstable at <40–45 beats per minute. Consequently, there is often significant haemodynamic compromise and a grave outlook.
This man suffered a cardiac arrest before he could be transferred for primary PCI and unfortunately he could not be resuscitated.


