This 28-year-old lady was found unconscious by her mother. She had significant mental health issues. She had written a suicide note and an empty pack of antidepressants and a bottle of vodka were found by her side.
Her vital signs were as follows:
- Blood pressure: 130/78 mmHg
- Pulse: 55 beats per minute
- Respiratory rate: 16 breaths per minute
- She was apyrexial
- SpO2 on air: 92%.
A 12-lead ECG was recorded as shown in Figure 1. Note that the ECG interpretative software is suggesting a diagnosis of ‘Acute MI [myocardial infarction] with ST elevation—consider inferior injury or acute infarct’. Clearly, the clinical presentation is not suggestive of an acute cardiac event.
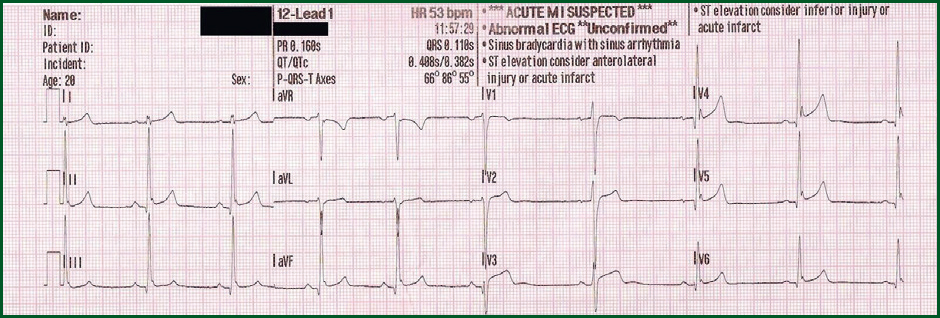
Interpretation of the ECG rhythm
- The heart rhythm is regular
- The heart rate is approximately 55 beats per minute
- The rhythm is sinus bradycardia.
There is ST segment elevation across a number of leads. However, in this case the changes are not as a consequence of acute myocardial infarction. Rather, this ECG suggests early repolarisation changes.
Early repolarisation is often referred to as ‘high take off’. It is usually a normal variant seen in fit young people, under the age of 50 years. It produces widespread ST segment elevation that may mimic pericarditis or acute MI. The ECG changes of early repolarisation generally disappear in middle age, and are rare in the elderly. It is possibly related to high sympathetic tone on the heart and can normalise with increased heart rates.
The main ECG changes seen in early repolarisation include:
- Elevated J Point often with notching (so-called ‘fish-hook’ appearance)
- Changes are predominantly in anterior chest leads V2–V5 but can occur elsewhere
- ST elevation is usually <2 mm in the precordial leads and <0.5 mm in the limb leads
- Absence of reciprocal changes or evolution / pathological Q waves.


