This 70-year-old man has presented to his GP with shortness of breath and chest tightness on exertion.
He lives at home with his wife. He no longer works, having retired as a Quantity Surveyor 5 years ago. He generally keeps well and travels extensively, regularly visiting his son who lives in Los Angeles, and a daughter in Western Australia.
He was investigated for exertional chest pain 7 years ago. A resting 12-lead electrocardiogram (ECG) and exercise tolerance test (ETT) were both reported as normal. He lost around two stones in weight through dieting and increasing his level of physical activity, and has felt well since.
Over the last few months, he has been aware that his exercise capacity has declined. When out walking, he now regularly stops to ‘catch his breath’ before continuing after several minutes of rest.
His vital signs were as follows:
Blood pressure: 169/98 mmHg
Pulse: 100 beats per minute with a very irregular pulse
Respiratory rate: 16 breaths per minute
He was apyrexial.
SPO2 on air: 98%
The 12-lead ECG in Figure 1 was recorded.
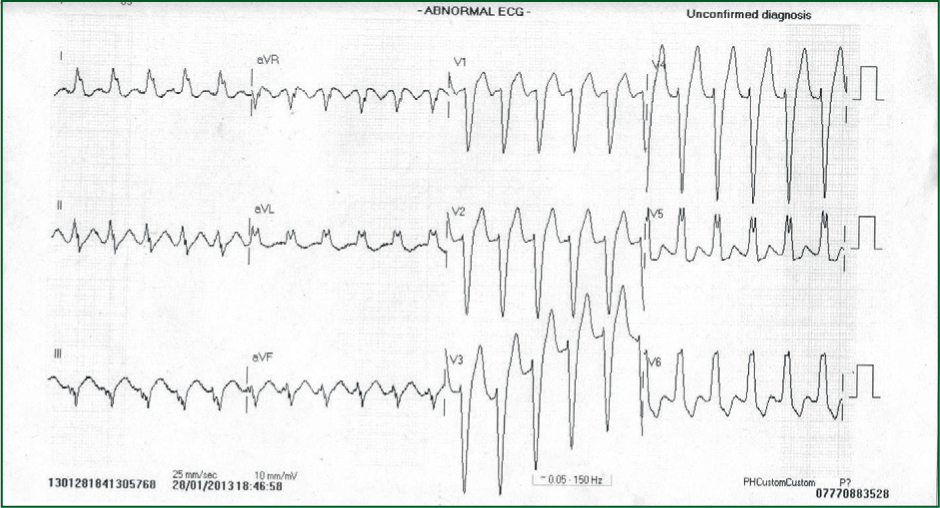
Interpretation of the ECG rhythm
- Heart rhythm is regular
- Heart rate is approximately 100 beats per minute
- The rhythm is sinus rhythm.
The most striking abnormality is the prolonged QRS duration. The QRS duration should be up to 100 milliseconds; whereas in this example, it is considerably prolonged, resulting in a wide QRS complex. There is a characteristic ‘M’ shaped QRS complex (an RSR morphology) in the lateral leads V5, V6, I and aVL. These ECG appearances are consistent with left bundle branch block (LBBB).
LBBB results in abnormal and delayed ventricular depolarisation, and consequently abnormal ventricular repolarisation. In LBBB, for the most part, both the ST segment and the T-wave are deflected in the opposite direction of the QRS deflection. This is called appropriate ST segment and T-wave discordance. This is an appropriate finding in LBBB and is a secondary ST/T-wave abnormality, i.e. the changes are not due to myocardial ischaemia/infarction.


