This 77-year-old man has presented with chest pain. He lives at home with his wife. He generally keeps well and manages to walk around 10 000 steps each day, mainly walking his beloved dog.
This morning, he was walking his dog on the local beach. It was a particularly cold and windy day and he felt a little short of breath when walking against the cold wind. Having walked for about 20 minutes, he developed an ache in his chest. It quickly developed into a heavy chest pain that was of such intensity that he dropped to his knees. The pain was tight in nature and radiated to his jaws. A passerby attended to him and he requested that she call an emergency ambulance as he felt sure that he was having a heart attack.
An ambulance arrived and he was transported to his local community hospital. En route to hospital, he suffered a cardiac arrest and was successfully defibrillated once with return of spontaneous circulation (ROSC).
His vital signs were as follows:
- Blood pressure: 139/88 mmHg
- Pulse: 60 beats per minute
- Respiratory rate: 16 breaths per minute
- He was apyrexial
- SPO2 on air: 95%.
Interpretation of the ECG rhythm
A 12-lead ECG was recorded (Figure 1).
- The heart rhythm is regular
- The heart rate is approximately 60 beats per minute
- The rhythm is sinus rhythm.
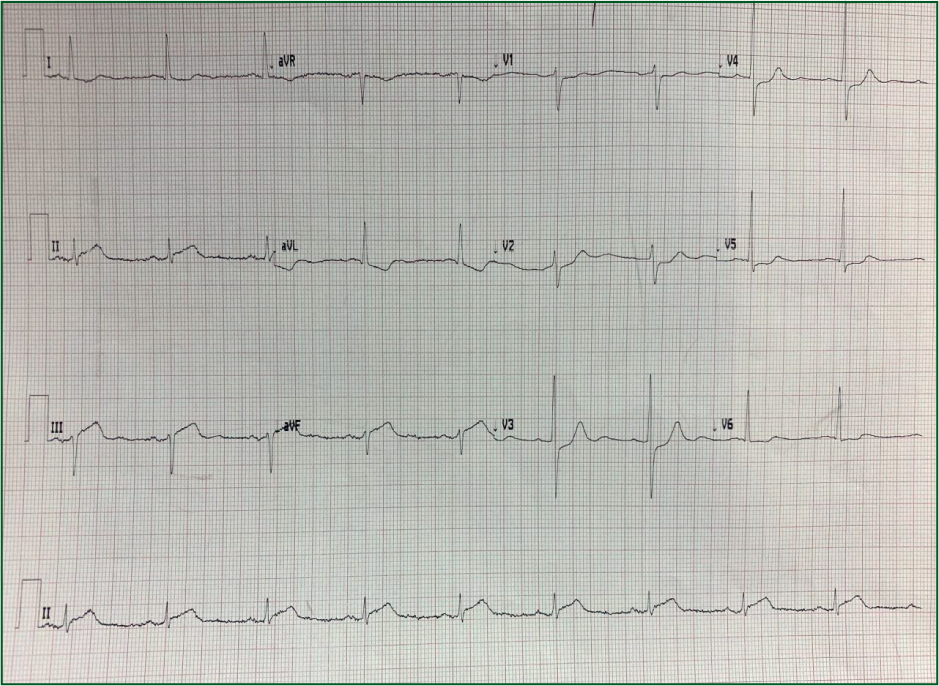
There is ST segment elevation in leads II, III and aVF, suggestive of an inferior ST elevation myocardial infarction (STEMI). There is no T wave inversion or pathological Q waves, which suggests a hyperacute appearance. This is in keeping with his early presentation.
There is ST segment depression across the chest leads, more obvious in V1–V3. This suggests involvement of the posterior wall of the left ventricle.
Inferoposterior myocardial infarction is generally seen in patients with an occlusion of the right coronary artery (RCA)
He was transferred to the nearest hospital capable of delivering percutaenous coronary intervention (PCI). Coronary angiography revealed a total occlusion of his proximal RCA. A single stent was inserted. He had an echocardiogram recorded 48 hours later. It demonstrated mild left ventricular impairment with akinesis of the inferior wall of the left ventricle.
He was discharged 3 days later on the following:
- Dual antiplatelet therapy (Asprin and ticagrelor)
- Beta blocker (bisoprolol)
- Statin (atorvostatin)
- ACE inhibitor (rampril).
He was reviewed by a cardiac rehabilitation specialist nurse 2 months later. He is doing well and has returned to his previous physical activity level.


