This 94-year-old man lives in a care home. He has had multiple hospital admissions over the last 2 years for general frailty and urinary tract problems. He is known to have prostate cancer that is being medically managed and has a permanent urinary catheter in situ. He had recently been in hospital for treatment of a urinary tract infection (UTI).
This morning, he complained of being short of breath at rest. He is normally mobile using a walking frame but today, he is unable to walk. His oxygen saturation was 89% on air. His pulse was also noted to be irregular. The last time this was checked, he had a normal, regular pulse. The staff in the care home decided to call for an ambulance.
His vital signs were as follows:
- Blood pressure: 98/58 mmHg
- Pulse: 86 beats per minute, with a very irregular pulse noted
- Respiratory rate: 20 breaths per minute
- He was apyrexial
- SpO2 on air: 89%.
The 12-lead electrocardiogram (ECG) in Figure 1 was recorded:
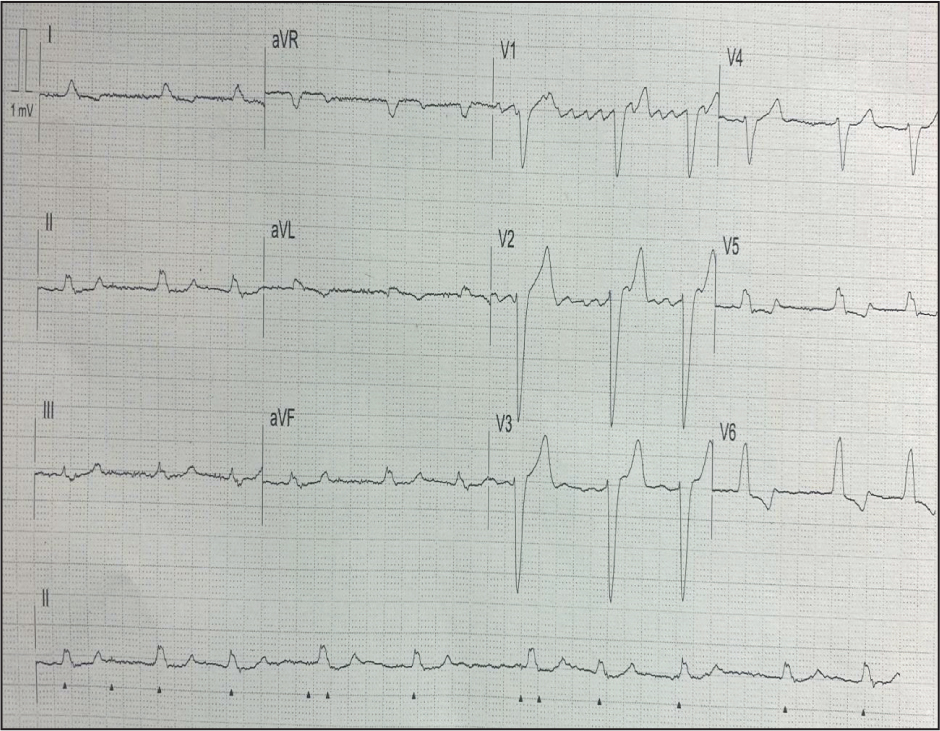
Interpretation of the ECG rhythm
- The heart rhythm is regular
- The heart rate is approximately 75 beats per minute
- The rhythm is very irregular
- The heart rate is approximately 80 beats per minute
- There are no identifiable P waves
- V1 in particular shows sawtooth flutter waves (hint: if you are struggling to see P waves on an ECG, have a look at V1 and V2 where atrial activity is often easier to see)
- The QRS complexes are >0.10 seconds in duration, i.e. wide
- There is a left bundle branch block (LBBB) configuration (RSR complexes in lead I, aVL, V5 and V6)
- The cardiac axis is normal (positive QRS complexes in leads I and aVF).
This ECG shows the patient to be in atrial flutter with a variable ventricular response and left bundle branch block configuration. His high sensitivity troponin was moderately elevated.
A final diagnosis of new onset atrial flutter and LBBB with subsequent heart failure was made.
LBBB causes an abnormal depolarisation. This also results in abnormal repolarisation, which causes a secondary ST/T wave abnormality. A primary ST/T wave abnormality would be caused by myocardial infarction. LBBB results in secondary ST/T wave abnormalities that can mimic ST segment elevation myocardial infarction (STEMI). In this case, there is appropriate ST segment and T wave discordance, i.e. in those leads with a positive QRS complex, the ST segment and T wave are deflected in the opposite direction and vice versa. This is an appropriate finding in LBBB and is a secondary ST/T wave abnormality, i.e. not ischaemia/infarction.


