The novel coronavirus pandemic has affected healthcare on an unprecedented global scale. The first cases of SARS-CoV-2 infection (COVID-19) were discovered in the Wuhan area of China (World Health Organization (WHO), 2020a), and the virus spread rapidly across the world, with COVID-19 being declared a pandemic by the World Health Organisation on 11 March 2020 (WHO, 2020b).
The first known cases of COVID-19 in the UK were recorded on 31 January 2020 (UK Government, 2021a). This was followed by a rapid increase in the number of cases between February and March 2020 as the virus spread through the population.
A government-imposed national lockdown came into effect on 23 March 2020, with the population being advised to stay at home and go out for essential reasons only, including grocery shopping, and all non-essential retail was closed (Institute for Government, 2021). Widespread testing for COVID-19 was not initially available in the UK.
Similar lockdowns came into force across Europe and the United States, where governments implemented stay-at-home orders with widespread limitations on domestic and international travel (Baldi et al, 2020; Marijon et al, 2020; Chan et al, 2021; Sultanian et al, 2021).
A small number of studies across Europe and North America have reported significant increases in the rate of out-of-hospital cardiac arrest (OHCA), coupled with a decrease in return of spontaneous circulation (ROSC) and overall survival to discharge since the start of the pandemic (Marijon et al, 2020; Baldi et al, 2020; Sultanian et al, 2021; Chan et al, 2021).
The profile of OHCA has also been reported to be changing, characterised by younger patients, a decreased frequency of shockable rhythms and a longer time to starting cardiopulmonary resuscitation (CPR) (Chan et al, 2021). The London Ambulance Service NHS Trust reported similar changes in OHCA in the only UK study to date (Scquizzato et al, 2020; Fothergill et al, 2021).
This study will be the only known one that aims to report the incidence, characteristics and rates of ROSC at hospital from OHCA attended by an air ambulance (critical care) service during the COVID-19 pandemic.
Thames Valley Air Ambulance
Thames Valley Air Ambulance (TVAA) provides prehospital enhanced and critical care to patients in the counties of Buckinghamshire, Berkshire and Oxfordshire between 07:00 and 02:00, 365 days a year. TVAA assets include an Airbus H135-T3 helicopter and five Skoda Kodiaq critical care response vehicles.
A critical care paramedic (CCP) and dispatch assistant are located within the South Central Ambulance Service NHS Foundation Trust (SCAS) control room to interrogate emergency calls and dispatch critical care assets. Patients may be attended by a doctor/CCP or double CCP team. CCPs have enhanced skills including the use of point-of-care ultrasound and sedation, and are supported by a remote senior on-call clinical adviser. Responding to OHCA accounts for almost 30% of TVAA's workload (TVAA, 2021).
During the first wave of the COVID-19 pandemic in the UK (March–May 2020), TVAA was able to maintain a doctor/CCP response, while also supporting the wider NHS response by placing CCPs in the major trauma centre emergency department and developing a critical care transfer service.
A COVID-19 supplementary procedure was developed in April 2020 to guide the dispatch and the on-scene management of OHCA in the context of a global pandemic, with the aim of reducing the risk of transmission to staff (TVAA, 2020). A more targeted dispatch process was adopted to identify patients with good prognostic factors (Table 1) or where critical care management was required (TVAA, 2020).
| Witnessed cardiac arrest |
| Effective bystander cardiopulmonary resuscitation |
| Shockable rhythm |
| Return of spontaneous circulation |
| ETCO2 >1.6 kPa |
| Consideration of a low frailty score (<5)/good premorbid function |
ETCO2: end-tidal carbon dioxide
Further supplementary procedures were developed, including a COVID-19 infection prevention and control handbook. This detailed enhanced personal protective equipment (PPE) requirements for when managing patients during the pandemic, as outlined by Public Health England to protect both staff and patients from exposure to COVID-19 (UK Government, 2021b). Level 2 PPE included donning a disposable apron and fluid-repellent surgical mask for all patient contact, with level 3 PPE (FFP3 facemask, fluid-repellent overalls and eye protection) being required for any aerosol-generating procedures (AGPs) such as airway suctioning and intubation (NHS, 2021).
The initial management of OHCA changed nationally across all ambulance services, with a focus on chest compressions and defibrillation only by the first responders until staff were able to safely don level 3 PPE to carry out airway management. TVAA emphasised the use of a functional supraglottic airway, a heat and moisture exchange filter and a 30:2 chest compression to ventilation ratio (TVAA, 2020). Other interventions remained unchanged. The use of enhanced levels of PPE have been identified as increasing response time to OHCA, with the potential to delay definitive care and airway management and also impact communication between responders (Chan et al, 2021). The outcomes of such changes remain unclear.
Methods
A retrospective review of patient records completed by TVAA clinicians using the HEMSbase system (Medic One Systems) was undertaken. A predefined search function was used to identify OHCA cases in HEMSbase for 2 consecutive years covering a pre-pandemic (1 February 2019–31 January 2020) and a pandemic period (1 February 2020–31 January 2021).
A population, intervention, comparison and outcome (PICO) framework was used to answer the question: in adult, medical OHCA attended by TVAA (P), has the COVID-19 pandemic (I), compared to a pre-pandemic period (C), changed the incidence, characteristics and outcomes from OHCA (O)?
Inclusion and exclusion criteria
All medical OHCAs attended by TVAA clinicians were included in the initial analysis.
All cases of trauma (any cause, including drowning, hanging and deliberate self-harm), patients aged <18 years, those with a documented do not attempt resuscitation order or known terminal phase of illness and cases with missing data were excluded.
Cases where a TVAA asset was stood down en route or not dispatched were not included in the analysis.
Data analysis
Data extracted from HEMSbase were interrogated using a Microsoft Excel spreadsheet and SPSS statistical software (IBM, v.26). The primary outcome of this study was ROSC on arrival at hospital. Descriptive statistics were used to analyse patient characteristics, OHCA location, the rate of bystander witnessed and/or CPR and automated external defibrillator (AED) deployment, response time, aetiology and initial rhythm and critical care interventions. Pearson's chi-squared test was used to establish statistical significance in patient outcome and key characteristics between the groups.
Cases in the pandemic period were screened for any COVID-19 symptoms (new/continuous cough, fever or loss/change in taste or sense of smell) (NHS, 2021) or a suspected or confirmed diagnosis of COVID-19 documented in the patient notes or operational log text. These cases were grouped for a subset analysis.
Ethics and study approval
This study was approved by the TVAA research and clinical audit working group and medical directorate in March 2021. Ethical approval was not required for this service evaluation.
Results
Despite a small drop in the overall number of patients attended between the two periods (7.9% reduction in pandemic period), there was an increase in the number of OHCA cases attended during the pandemic (18.0% in 2019–2020 compared to 24.7% in 2020-2021) (Figure 1).
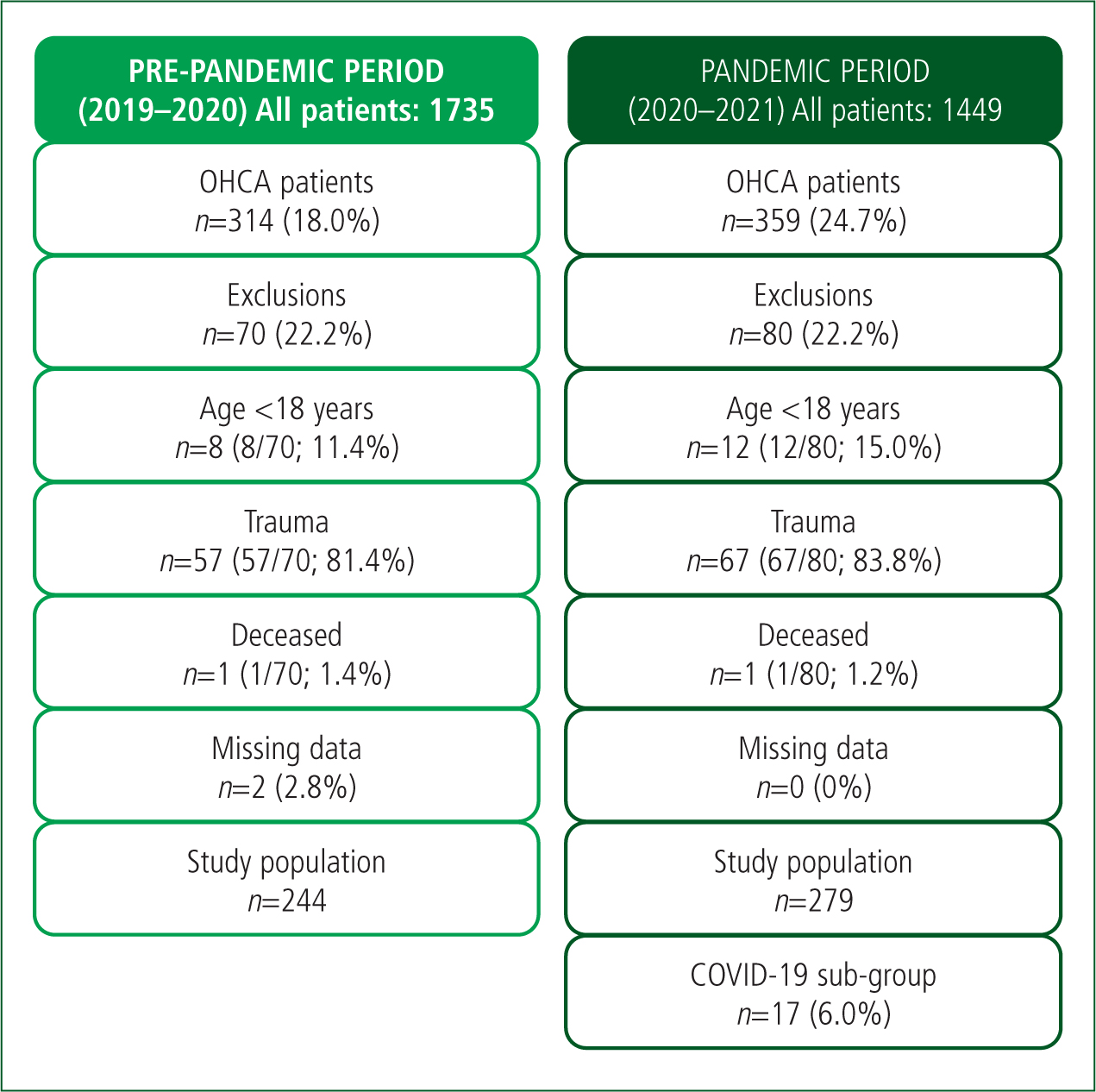
The prevalence of COVID-19, based on documented symptoms, in the pandemic period was 6.0% (n=17/279).
OHCA characteristics
Patients in the pandemic period, specifically those in the COVID-19 sub-group, were younger than those in the pre-pandemic period: median age 60 (IQR 51–71) in the pre-pandemic period; median age 58 (IQR 48–68) in the pandemic period; median age 52 (IQR 45–60) in the COVID-19 sub-group. There was a higher prevalence of male patients in both groups, increasing in the pandemic period (72.1% versus 78.1%; P=0.096). Baseline characteristics are described in detail in Table 2.
| 2019–20 | 2020–21 | P | Non-COVID-19 | COVID-19 | P | |
|---|---|---|---|---|---|---|
| n=244 | n=279 | n=262 (93.9%) | n=17 (6.0%) | |||
| Age (years) | ||||||
| Median (IQR) | 60 (51–71) | 58 (48–68) | 58 (48–68) | 52 (45–60) | ||
| Gender (n, %) | ||||||
| Male | 176 (72.1%) | 218 (78.1%) | 0.096 | 207 (79.0%) | 11 (64.7%) | <0.001 |
| Female | 68 (27.8%) | 60 (21.5%) | 54 (20.6%) | 6 (35.2%) | ||
| Transgender | 0 | 1 (0.3%) | 1 (0.3%) | 0 | ||
| Location (n, %) | ||||||
| Home | 154 (63.1%) | 195 (69.8%) | 0.101 | 181 (69.0%) | 14 (82.3%) | <0.001 |
| Public place | 13 (5.3%) | 10 (3.5%) | 0.274 | 63 (24.0%) | 2 (11.7%) | <0.001 |
| Work | 66 (27%) | 65 (23.2%) | 10 (3.8%) | 0 | ||
| Other | 11 (4.5%) | 9 (3.2%) | 8 (3.0%) | 1 (5.8%) | ||
| Bystander witnessed (n, %) | ||||||
| Witnessed OHCA | 146 (59.8%) | 171 (61.2%) | 0.734 | 115 (43.8%) | 16 (94.1%) | <0.001 |
| Bystander CPR | 169 (69.2%) | 194 (69.5%) | 180 (68.7%) | 14 (82.3%) | ||
| Bystander AED | 26 (10.6%) | 26 (9.3%) | 26 (9.9%) | 0 | ||
| Response time (mins) | ||||||
| Helicopter (median, IQR) | 00:20 (00:16–00:26) | 00:21 (00:16–00:25) | 00:20 (00:14–00:26) | 00:17 (00:14–00:20) | ||
| Car (median, IQR) | 00:21 (00:12–00:25) | 00:19 (00:12–00:27) | 00:20 (00:14–00:26) | 00:17 (00:12–00:22) | ||
| Response platform (n, %) | ||||||
| Helicopter | 72 (29.5%) | 103 (36.9%) | 97 (37.0%) | 6 (35.2%) | ||
| Critical care response car | 172 (70.4%) | 176 (63.0%) | 165 (62.9%) | 11 (64.7%) | ||
| Aetiology (n, %) | ||||||
| Presumed cardiac | 68 (27.8%) | 88 (31.5%) | 0.360 | 83 (31.6%) | 5 (29.4%) | 0.845 |
| Medical other (non-cardiac) | 176 (72.1%) | 191 (68.4%) | 179 (68.3%) | 12 (70.5%) | ||
| Initial rhythm (n, %) | ||||||
| VF/pVT | 83 (34.0%) | 119 (42.6%) | 0.043 | 114 (43.5%) | 5 (29.4%) | <0.001 |
| PEA | 44 (18.0%) | 51 (18.2%) | 47 (17.9%) | 4 (23.5%) | ||
| Asystole | 107 (43.8%) | 99 (35.4%) | 0.051 | 91 (34.7%) | 8 (47.0%) | <0.001 |
| Unknown | 71 (29%) | 88 (31.5%) | 10 (3.8%) | 0 | ||
| Critical care intervention (n, %) | ||||||
| No airway on arrival | 35 (14.3%) | 95 (34.0%) | 0.034 | 89 (33.9%) | 6 (35.2%) | <0.001 |
| Intubation (excluding PHEA) | 59 (24.1%) | 77 (27.5%) | <0.001 | 73 (27.8%) | 4 (23.5%) | 0.736 |
| PHEA | 31 (12.7%) | 32 (11.4%) | 30 (11.4%) | 2 (11.7%) | ||
| Sedation (+/- paralysis) | 19 (7.7%) | 16 (5.7%) | 16 (6.1%) | 0 | ||
| Ultrasound (echo) | 55 (22.5%) | 107 (38.3%) | 99 (37.7%) | 8 (47.0%) | ||
| Additional drugs | 15 (6.1%) | 29 (10.3%) | 27 (10.3%) | 2 (11.7%) | ||
| Outcome (n, %) | ||||||
| ROSC at hospital (all) | 92 (37.7%) | 87 (31.1%) | 0.117 | 83 (31.6%) | 4 (23.5%) | <0.001 |
| ROSC at hospital (Utstein) | 36 (39.1%) | 36 (41.3%) | <0.001 | 35 (13.3%) | 1 (5.8%) | <0.001 |
| Transported to ED in arrest | 43 (17.6%) | 37 (13.2%) | 35 (13.3%) | 2 (11.7%) | ||
| Transported to PPCI in arrest | 5 (2.0%) | 2 (0.71%) | 2 (0.7%) | 0 | ||
| Died at scene | 104 (42.6%) | 153 (54.8%) | <0.001 | 142 (54.1%) | 11 (64.7%) | <0.001 |
AED: automated external defibrillators; CPR: cardiopulmonary resuscitation; ED: emergency department; IQR: Interquartile range; OHCA: out-of-hospital cardiac arrest; PEA: pulseless electrical activity; PHEA: prehospital emergency anaesthesia; PPCI: primary percutaneous coronary intervention; ROSC: return of spontaneous circulation; VF/pVT: ventricular fibrillation/pulseless ventricular tachycardia
Bystander-witnessed OHCA
The rate of bystander-witnessed OHCA showed a slight increase between the pre-pandemic and pandemic periods (59.8% versus 61.2%; P=0.734).
However, bystander CPR provision remained largely similar between the two groups. The largest increase in bystander CPR was seen between the COVID-19 sub-group and the non-COVID sub-group.
These were coupled with an overall increase in OHCA occurring in the home environment and reduction in OHCA occurring at work or in a public place because of the lockdown restrictions.
Response time
The response times remained largely unchanged between the study periods on both aircraft and road platforms.
As expected, the number of incidents attended by helicopter increased because of a reduction in critical care car availability following paramedic redeployment during the initial lockdown (April to May 2020).
Initial rhythm and aetiology
The rate of shockable rhythms increased between the pre-pandemic and pandemic periods (34.0% versus 42.6%). Shockable rhythms were less common in the COVID-19 sub-group (29.4% compared to 43.5% in the non-COVID-19 sub-group). Presumed cardiac aetiology increased between the pre-pandemic (27.8%) and the pandemic period (31.5%).
Critical care intervention
There was an increase of 19.7% in no airway management, defined as no advanced airway (supraglottic or endotracheal tube) in the patient on arrival at scene of TVAA during the pandemic period.
The rate of intubation (excluding ROSC patients intubated as part of pre-hospital emergency anaesthesia (PHEA)) showed an unexpected increase between the two study periods (24.1% versus 27.5%; P<0.001). The rate of undertaking post-ROSC PHEA remained largely unchanged between the two periods.
Outcome
There was a reduction in overall ROSC on arrival at hospital (pre-pandemic period 37.7% versus pandemic period 31.1%; P=0.117) between the two study periods. The number of patients who were pronounced life extinct on scene saw a significant increase in the pandemic period (42.6% to 54.8%; P<0.001). Poorer outcomes were observed in patients with suspected or confirmed COVID-19 when compared to pre-pandemic times.
Discussion
This is the only known study to report and compare the incidence and ROSC at hospital from OHCA in a UK air ambulance setting before and during the pandemic. The general findings of this study are consistent with those of similar studies from Europe and North America (Baldi et al, 2020; Marijon et al, 2020; Scquizzato et al, 2020; Sultanian et al, 2021).
The primary outcome of this study was ROSC on arrival at hospital, which, as other studies show, decreased during the pandemic period and in those with suspected or confirmed COVID-19. This was coupled with a large increase in the termination of resuscitation at scene. The Resuscitation Council UK criteria for termination of resuscitation remained unchanged (TVAA, 2020; Bossaert et al, 2015).
The relationship between OHCA and the prevalence of COVID-19 in the general population was not examined in this study. During the first wave of the pandemic, widespread testing for COVID-19 was not available and the true incidence of the disease was unknown (UK Government, 2021a). The prevalence of COVID-19 symptoms among OHCA patients varies in this and other reported studies, ranging from 4.8% in Seattle (Chan et al, 2021) to 26% in Lombardy (Marijon et al, 2020) and 6.0% as seen in this study.
Several studies across Europe (Chan et al, 2021) report a general reduction in the presence of shockable rhythms and reduced number of presumed cardiac causes of OHCA. In contrast, this study found a significant increase in both shockable rhythm and presumed cardiac aetiology. However, the increase in shockable rhythms and cardiac aetiology was unlikely a result of COVID-19 and more likely a result of a more targeted approach to the dispatch of critical care assets to OHCA cases where the assumption of a more favourable outcome had been made.

Furthermore, if this study were to include all cases of OHCA from across the South Central ambulance area, it is likely that the results would be similar to those seen across Europe, where much larger case volumes have been reported.
TVAA response times remained largely unchanged and this study did not examine the ambulance service response to OHCA. The studies conducted in Europe and America found an increase in the overall ambulance response to OHCA, which was associated with a decrease in shockable rhythms (Baldi et al, 2020; Marijon et al, 2020; Chan et al, 2021; Sultanian et al, 2021). As a supplementary response to the ambulance service, TVAA was not commonly first on scene at OHCA incidents. It is feasible that the attending ambulance service colleagues providing basic and advanced life support before TVAA arrival, coupled with targeted dispatch, account for the increase in shockable rhythms.
As reported, a strict national lockdown was imposed by the UK Government (2020) on 23 March 2020. The impact of such restrictions on the wider health community and population remains under-reported. A study of acute hospital trusts in England found a 40% reduction in admissions for acute coronary syndromes in the first 3 months of 2020 (De Filippo et al, 2020; Mafham et al, 2020).
This supports the suggestions in other OHCA studies that the impact of such restrictions, coupled with fear of COVID-19 disease, led to a reduction in people seeking help for new and existing conditions (Sultanian et al, 2021). This could potentially account for the increase and presence of shockable rhythms in the pandemic period seen in this study.
COVID-19 is well documented as a respiratory disease (Esakandari et al, 2020) that can have several cardiovascular implications, including myocardial dysfunction, arrhythmia, heart failure and myocarditis (Samidurai and Das, 2020). These effects and the risk of complications of COVID-19 are dramatically higher in patients with pre-existing cardiovascular disease, which is itself a leading cause of mortality in the UK, particularly in men (Office for National Statistics, 2020).
The pathophysiology of the COVID-19 disease process may also account for an increased presence of shockable rhythms and presumed cardiac cause seen in this study. However, the data presented are insufficient to draw any accurate conclusions.
The increase in no initial airway management on arrival of TVAA was as expected, given the changes in guidance around starting resuscitation (TVAA, 2020), which advocated carrying out no aerosol-generating procedures until clinicians had donned appropriate levels of PPE (TVAA, 2020; UK Government, 2021b).
There was much controversy in the early stages of the pandemic surrounding compression-only CPR, especially given the nature of COVID-19 as a respiratory illness, with the potential to cause OHCA because of hypoxia (Esakandari et al, 2020). This could have influenced outcomes from OHCA, where delayed oxygenation and ventilation as part of advanced life support may be detrimental to the patient. However, it was not within the remit of this study to establish such links between cause and effect.
Despite the TVAA (2020) supplementary procedures for OHCA advocating the use of supraglottic devices, the rate of intubation (excluding PHEA) showed a significant increase (pre-pandemic period 24.1% versus pandemic period 27.5%; P<0.001). There was no obvious indication to explain such an increase and further exploratory work is required to better understand the possible reasons behind this.
Other critical care interventions examined in this study include the delivery of PHEA, sedation (and paralysis during a physician/paramedic response), ultrasound and additional drugs as outlined in the Resuscitation Council UK (2021) guidelines (calcium chloride, magnesium, sodium bicarbonate and vasoactive drugs for post-ROSC care). Large increases in the use of ultrasound and additional drugs were seen in the pandemic period.
As of January 2020, all critical care paramedics at TVAA had undergone initial training in point-of-care ultrasound and had begun to undertake supervised scans towards Royal College of Emergency Medicine (RCEM) sign-off (RCEM, 2010). This may account for the increase in the use of ultrasound seen in this study.
The exact indications for the use of additional drugs were not explored but may be as a result of more deranged and abnormal respiratory and cardiac presentations that have been associated with COVID-19 (Samidurai and Das, 2020).
Limitations
Outcome data beyond ROSC on arrival at hospital is not available to TVAA and limits this study in its ability to comment on the true outcomes of OHCA between pandemic and pre-pandemic times.
In comparison to other published data, this study has a smaller study population in both periods. Ambulance service data were not analysed as they include counties outside the TVAA's operational area and would not be fully representative of OHCA cases that TVAA could attend.
TVAA routinely records cases of ‘missed jobs’ where an asset was not able to attend or mutual aid attended. These data were not included within this study, and including these may have increased the study population.
Furthermore, ambulance service data on attendance at OHCA were not available for the 2021 study and were not reviewed as part of this study.
Conclusion
OHCA remains a leading cause of mortality across the globe. The findings of the present study highlight the impact of an unprecedented global pandemic on an air ambulance system and the implications for patient characteristics, outcomes from OHCA and changes in how air ambulance systems respond to such global health challenges.
Further exploration of the effects of COVID-19 is required, particularly surrounding OHCA care and its impact on systems and patients alike.

