Crisis Resource Management (CRM) had its humble beginnings in the training of airline pilots in the 1960's (Howard et al, 1992). Teamwork and effective communication were subsequently identified as essential principles of CRM in the clinical context (Gaba, 2001). These components were then adapted and adopted into the training of many medical practitioners (Holzman et al, 2005). These principles therefore intend to encourage teamwork, situation awareness, and effective communication through empowering people to speak up in an emergency scenario. The aim of CRM is to ultimately improve patient safety and prevent at risk situations or events.
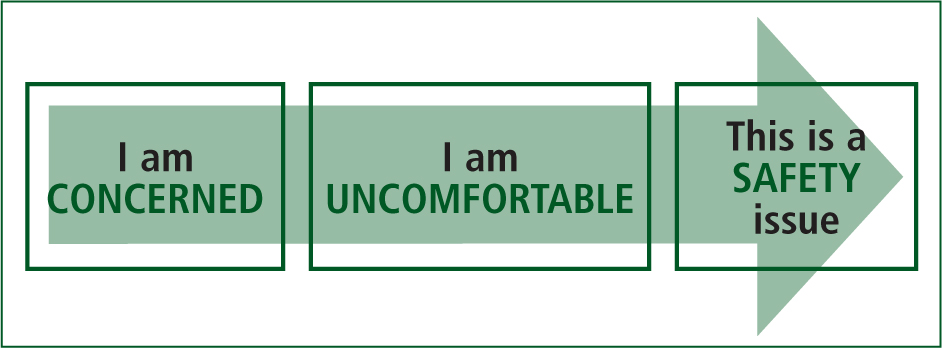
Researchers in pre-hospital emergency medical care have identified teamwork and effective communication as essential components in the delivery of high quality and safe patient care (Leonard et al, 2004). Moreover, the team leaders have been identified as an important link in fostering a positive teamwork environment. These leaders are encouraged to inspire the emergency medical care (EMC) practitioner to speak up. Being vociferous in such situations and giving productive input will translate to providing effective care to the patient. EMC practitioners are also advocates of patient safety and are therefore encouraged to follow the “Concerned, Uncomfortable, Safety” (CUS) principle and two-challenge rule (Hunt et al, 2007). These principles, if utilised correctly, minimise patient risks and maximise patient benefits.
This report explores the emergency medical service (EMS) environment in which EMC is performed in the State of Qatar. Furthermore, the importance of working as a unified team in the context of CRM in pre-hospital care is highlighted.
Background about the State of Qatar
The population of Qatar is in excess of 2.42 million (76.2% male versus 23.8% female) (MDPS, 2016). Almost 90% of the country's population comprises expatriate workers. The country's most populous migrant workforces include: Indians, Nepalis, Filipinos, Egyptians, Bangladeshis, Sri Lankans, and Pakistanis (Goodman, 2015).
Healthcare in Qatar
The Ministry of Public Health regulates healthcare in Qatar. The country maintains high healthcare standards (Goodman, 2015), and its investment in healthcare has increased over the years. In 2014, Qatar invested $4.7 billion in healthcare (Hussin et al, 2015). This expenditure is very significant in relation to the population size; however, the country's healthcare system is being hampered by high rates of obesity, diabetes, and genetic disorders. Sixteen percent of the adult population were diagnosed with diabetes in 2013 (Walker, 2014). The top 10 causes of death in Qatar in 2012 were: ischaemic heart disease (14.7%), diabetes mellitus (8.9%), road injury (7.6%), stroke (4.4%), self-harm (3.5%), falls (2.8%), trachea/bronchus/lung cancer (2.6%), kidney diseases (2.4%), endocrine/blood/immune disorders (2.2%), and colon and rectum cancers (2.0%) (WHO, 2013).
Hamad Medical Corporation (HMC) is the main government healthcare provider in Qatar. HMC operates eight hospitals (HMC, 2016). In addition, there are also 21 government funded Primary Healthcare Centres and three main private hospitals in the country. HMC also operates an ambulance service and a mobile doctor service (HMC, 2016). These healthcare resources are strained. There were 170,000 emergency calls and 1,600,000 adult and paediatric emergency visits nationally in 2014 for a population of around 2.2 million inhabitants (HMC, 2015).
Pre-hospital emergency medical care in Qatar
The provision of pre-hospital EMC in Qatar is provided by the national Ambulance Service (HMCAS). EMS operations are labour intensive, the world over. HMCAS depends on the professional preparedness of its culturally diverse EMC practitioners. HMCAS operates a hub and spoke model with a tiered response approach. This involves ambulances with a crew of two paramedics (AP), rapid response vehicles with a critical care paramedic (CCP) and an ambulance paramedic, and supervisors credentialed at the AP level of clinical practice.
CCPs employed by HMCAS (n=100) have been recruited from various countries including: South Africa, Australia, New Zealand, Canada, and the United States of America (USA). These practitioners have received diversified training in various systems in their home countries. They are commonly trained to provide the highest level of care in the pre-hospital environment. They are knowledgeable and skilled in performing various invasive and non-invasive procedures as highlighted in the organisation's Clinical Practice Guidelines (CPG) (HMCAS, 2016).
In the local emergency environment, the CCP works with other practitioners from various linguistic and cultural backgrounds. The APs (n=1331) at HMCAS are recruited primarily from Tunisia, India, Philippines, Jordan, Morocco, Egypt, Great Britain, and the USA (Figure 1). Within the State of Qatar, the CCP and AP function in numerous roles including; clinical operations, aeromedical, management, education, and specialised medical services. Qatar's multinational population adds to the diversity of EMC practice in the country. In addition, structures within HMCAS are hierarchical. These factors may create an environment which is not conducive to effective communication and may inherently suppress free expression of speech in the emergency situation and in the day-to-day working practices.

Practitioners are the most salient port of call in pre-hospital emergencies. These practitioners are expected to possess excellent judgement to allow them to function optimally and independently in unstructured and constantly changing environments. Furthermore, these practitioners are equipped with the knowledge, skills, and experience to be able to make sound clinical decisions in haste.
Patient safety is a vital component of professional practice (Fanning, 2013) for practitioners. It is impacted upon by various factors in the pre-hospital environment at HMCAS including clinical decision making by practitioners, adverse events and medication errors, communication within the organisation, emergency driving during patient transportation, safety around aircraft operations, inter-facility transportation of patients, extreme weather conditions, and rapid sequence induction of the critical patient. Essential familiarisation and adherence to the 15 CRM principles identified by Rall et al. (2005) has been identified to enhance patient safety (Table 1).
| Decision making | Teamwork and resource management |
|---|---|
| Know the environment | Call for help early |
| Anticipate and plan | Exercise leadership and fellowship |
| Use all available information | Distribute the workload |
| Prevent and manage fixation errors | Mobilise all available resources |
| Cross check | Communicate effectively |
| Use cognitive aids | Use good teamwork |
| Re-evaluate repeatedly | |
| Allocate attention wisely | |
| Set priorities dynamically |
The impact of teamwork and effective communication in pre-hospital EMC
Very little research has been done on CRM in the pre-hospital setting. Most research in the CRM field has been conducted in other medical areas, mainly anaesthesia (Howard et al,1992; Gaba et al, 2001).
Communication between practitioners, in a situation where time is critical and decisions need to be made, is of great importance. It is one of the major processes of group dynamics. Mediated by a team leader, if required, communication in a team aims to encourage and empower each member to speak up if and when there is a concern to be raised (Howard, 1992), or feedback needs to be provided to one or more team members to improve patient care. Feedback needs to be timely, considerate, and specific (Ramani and Krackov, 2012) to promote the highest standards of patient care possible. Practitioners should really be “watching each other's back” (Cross monitoring) (Ferguson, 2008).
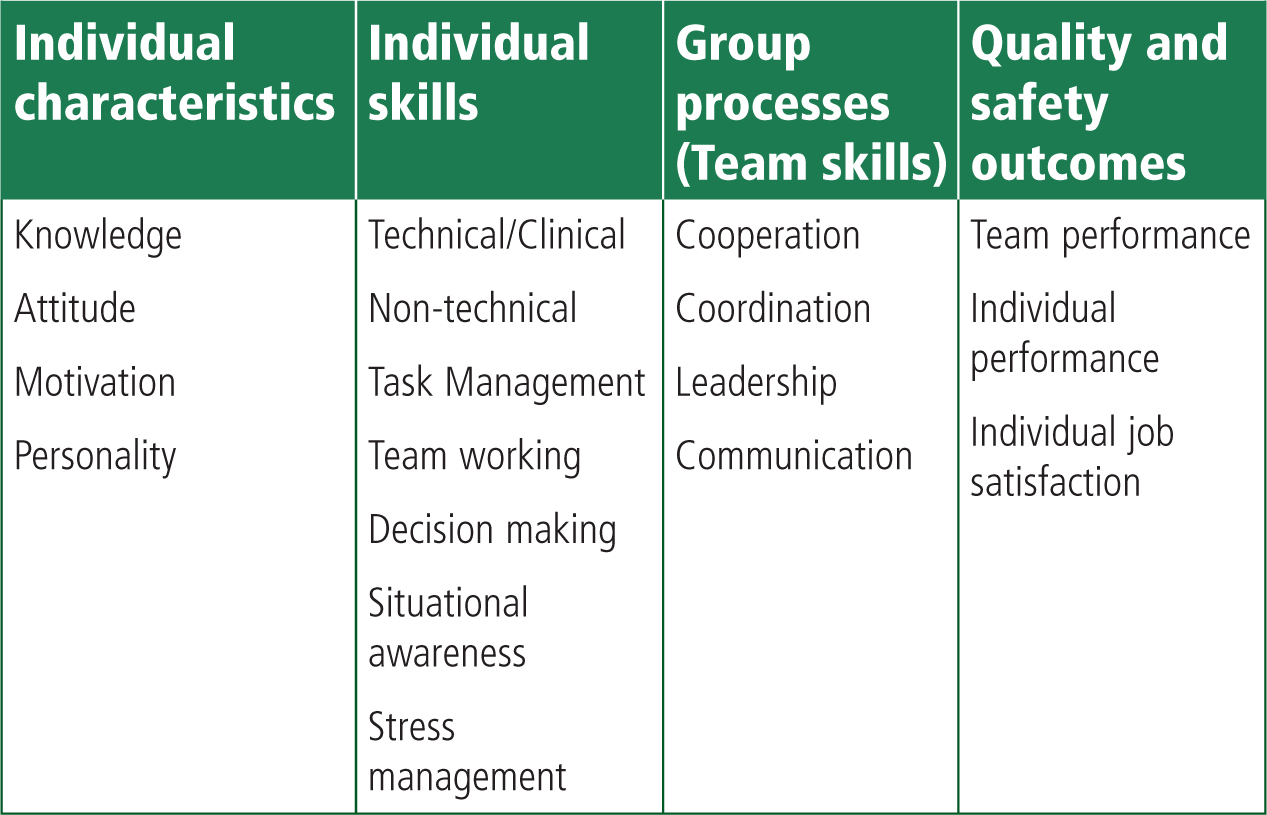
CRM training was introduced into HMCAS to overcome patient safety compromises. The tenets of teamwork training included the individual's characteristics, individual skills, group processes and quality and safety outcomes (Figure 2.). Initially it was included as part of the orientation programme of all newly recruited practitioners. Improvements stemmed the inclusion of CRM in specialised continuing professional development (CPD) educational courses (Alinier et al, 2014). This implementation aimed to standardise team dynamics and promote good communication and teamwork among staff of differing seniority levels and cultural backgrounds. At HMCAS, implementation relies primarily on the tools presented in the TeamSTEPPS training package, which is part of the mutual support team competencies (Henriksen et al, 2008). To that effect patient safety is dependent on the skills, knowledge, vigilance, and judgement of all trained EMC practitioners (Murray et al, 2000) in a wide range of direct and indirect patient care aspects.
Certain communication tools including CUS and the two-challenge rule are appropriate for early identification of patient safety risks in the pre-hospital setting. The CUS principle can be identified as an informal “verbal warning” to the EMC team about the issue and its magnitude in the case of a first occurrence (Hunt et al, 2007). It is predicated on a three-step technique. The first step includes the EMC practitioner stating their concern. In the second step the EMC practitioner identifies why they are uncomfortable about the issue. The final step identifies the safety issue if the course of action is not altered. In this third step, the EMC practitioner identifies why they highlighted the safety issue and what different action is required to remedy the breech in safety (Figure 3). If used to raise a concern previously identified and not resolved, it may have to be formally escalated for mediation by involving line managers. It then falls out of its primary “mutual support” usage among colleagues or the provision of feedback, and the primary concern is the wellbeing of patients.
The hierarchical pre-hospital EMC setting may be a deterrent to effective communication in Qatar. EMC practitioners may not be forthcoming with their concerns to the detriment of patient safety. Managers should therefore be encouraged to create an environment whereby practitioners can speak up, irrespective of culture or nationality, as opposed to feeling suppressed by the presence of more senior or experienced colleagues. These practitioners must be able to openly raise the “red flag” with their concerns regarding patient safety. The two-challenge rule helps identify patient risks and allows junior practitioners to challenge decisions taken by their senior counterparts (Pian-Smith et al, 2008).
The two-challenge rule was therefore designed to be invoked when the team leaders' decisions become questionable and is not agreed upon by the rest of the team members. These team members are encouraged to “stop the line” when a safety breach involving the patient and or practitioners is discovered. Members are informed to be assertive in a respectful manner to the senior practitioners. When the first assertive statement is ignored, the team member should raise their assertiveness once more. This should stimulate the senior practitioner to acknowledge the challenge and rethink their pathway of patient care, minimising the risk. Failure by the senior practitioner to acknowledge the patient safety concern must be immediately escalated through the management chain of command (Pian-Smith et al, 2008).
Incorporating the CUS principle and two-challenge rule into the realm of EMS practice is challenged by team dynamics and ingrained cultural norms. Getting different people to work together in unison to meet the organisation's goals may create challenges to management structures. These goals may sometimes be misinterpreted or conflict with the practitioners' personal goals. It is therefore imperative that the right EMC practitioners are employed and that they are further tuned to operate in harmony. Regular training programmes must be offered to these practitioners to overcome barriers that promote poor teamwork. As endorsed through our training programmes, EMC practitioners must be encouraged to call for help early, exercise leadership and followership, distribute the workload, mobilise all available resources, communicate effectively, and use good teamwork (Table 1 and 2).
| Team structure | Relates to team size, membership, leadership, composition, diversity, identification of goal, and distribution of tasks. |
| Leadership | Ability to coordinate the activities of team members by ensuring team actions are communicated, understood, that changes in goal prioritisation are dynamically shared, and that team members have the necessary resources and guidance. |
| Situation monitoring | Process of actively scanning and assessing situational elements to gain information, understanding or maintaining awareness to support the team function progressing toward its goal. |
| Mutual support | Ability to anticipate and support other team members' needs through accurate knowledge about their responsibilities and workload, and the provision of feedback. |
| Communication | Process by which information is clearly and accurately exchanged among team members, according to pre-set standards and processes. |
EMC practitioners are affected by barriers related to the individual, the team, and the environment in which they function. The individual's ability to work safely is potentially affected by fatigue, sleep deprivation, anger, stress, ill health, inexperience, lack of knowledge, and fear of reprimand. Team dynamics such as role confusion, authority, and ineffective communication skills labour the process of effective teamwork. In addition, environmental factors add to teamwork pressure. Equipment failure, noise, interruptions, unfamiliar places all contribute to poor teamwork. (Reznek, 2003; Hicks et al, 2008).
The involvement of all team members during an emergency situation is essential to minimising patient safety risks and optimising their outcomes. The teamwork principles must be promoted (Table 2). Education and training in CRM using simulations will improve team dynamics. During the simulations, team members must be encouraged to speak and contribute meaningfully towards the patient's treatment. Clearly identified roles and responsibilities of each team member will create an environment which is conducive to quality patient care. CRM training should be a continuous process commencing during employee orientation. CRM training must then be conducted regularly with all role players in different settings in the form of CPD. This will ensure that participants overcome individual, team, and environment pressures in a controlled setting (Alinier and Newton, 2013).
CRM must involve the training of individuals to function in teams whereby non-technical skills such as: collaboration, communication, task management, teamwork, and leadership are taught and are accompanied by practice and feedback encouraging reflection on the part of the practitioners.
Although much work has gone into CRM over the past two decades, more work still has to be completed (Gaba, 2010). Various dynamics exist in articulating an appropriate CRM model for EMC. Repeated regular training will facilitate effective teamwork and help minimise risks in patient care (Jankouskas et al, 2007). Logarajah and Alinier (2014) proposed an acronym (ABCDE approach) to help recall the CRM principles and to increase patient safety.
Conclusion
This article explored CRM in relation to empowering people to speak up in the context of a Middle Eastern ambulance service with a highly heterogeneous workforce. Researchers in this field encourage teamwork and effective communication as a means to bridge cultural and communication barriers. In order to overcome these barriers and encourage EMC practitioners to “speak up” during clinical practice, the researchers recommend that the CRM principles are enforced regularly. Training on the CUS, two-challenge rule, and other TeamSTEPP principles must be entrenched in all EMC learning programmes. Furthermore, these principles must be reinforced through continuous professional development activities. Evaluation and monitoring systems must be instituted to identify at risk situations and prevent patient safety breaches.
Training on the principles of CRM and teamwork are expected to improve compliance and patient safety. HMCAS is well underway of inculcating CRM principles into its EMC practitioners. They are well incorporated as part of the EMC's orientation programme and specialised CPD courses; however, CRM training should be conducted more regularly with all role players, including supervisors, in different settings, and using scenarios that help create specific situations calling for the application of the communication tools and teamwork principles. We now aim to monitor changes in attitudes and organisational culture over time, and how it impacts on case reviews and patient outcome.

