Initially, thrombolysis was administered in hospital to patients presenting with acute ST-elevation myocardial infarction (STEMI). (GISSI, 1986; ISIS—2, 1988). This treatment dissolves the thrombus and thereby restores perfusion to the ischaemic myocardium.
In order to administer this treatment as quickly as possible, targets were set to achieve optimal ‘call-to-needle’ times (the time from the patient making the call for help to the time when thrombolysis was administered) and ‘door to needle’ times (the time from when the patient arrived at the hospital to the time when thrombolysis was administered). A lot of work was carried out to ensure that the patient was transported to hospital as quickly as possible and also to ensure that a slick system was in place within the hospital for the timely administration of intravenous thrombolytic therapy. The principle that ‘time means muscle’ was established—i.e, the quicker thrombolysis was given, the more left ventricular muscle was saved (GISSI, 1986; ISIS—2, 1988).
Delays to treatment
One ongoing delay to the administration of treatment to patients with acute STEMI is the delay between the onset of symptoms for a patient and the time when they call for help. This is often substantial. Patients often ignore their symptoms for a considerable period of time before calling for help, or assume that they are simply due to indigestion until they finally accept that they could represent something more serious.
The best way to reduce the time interval from symptom onset to the call for help is by educating patients and the general public. There have been various campaigns to encourage individuals to seek help if they develop symptoms suggestive of acute myocardial ischaemia. Often, patients who have experienced an acute STEMI will call for help at an earlier stage if they have a recurrent event some months or years later. Ongoing education is required to try and keep the time from symptom onset to the call for help as reasonable as possible.
Prehospital thrombolysis
In order to try and reduce the ‘call-to-needle’ times, prehospital thrombolysis was introduced (Weston et al, 1994; Khan et al, 2009). The patient is assessed on site by the paramedic team and an electrocardiogram (ECG) is recorded. The resting ECG is usually transmitted to a centre for further evaluation. A decision is then reached between the paramedic crew and the centre as to whether thrombolysis should be administered on site—i.e prehospital. Once thrombolysis has been given, the patient is then transported to hospital for ongoing care. This system of prehospital thrombolysis proved to be extremely effective and led to a marked reduction in the ‘call-to-needle’ times (Khan et al, 2009). This service has been particularly effective in the geographically remote areas where the transfer times from the patients home to hospital are long.
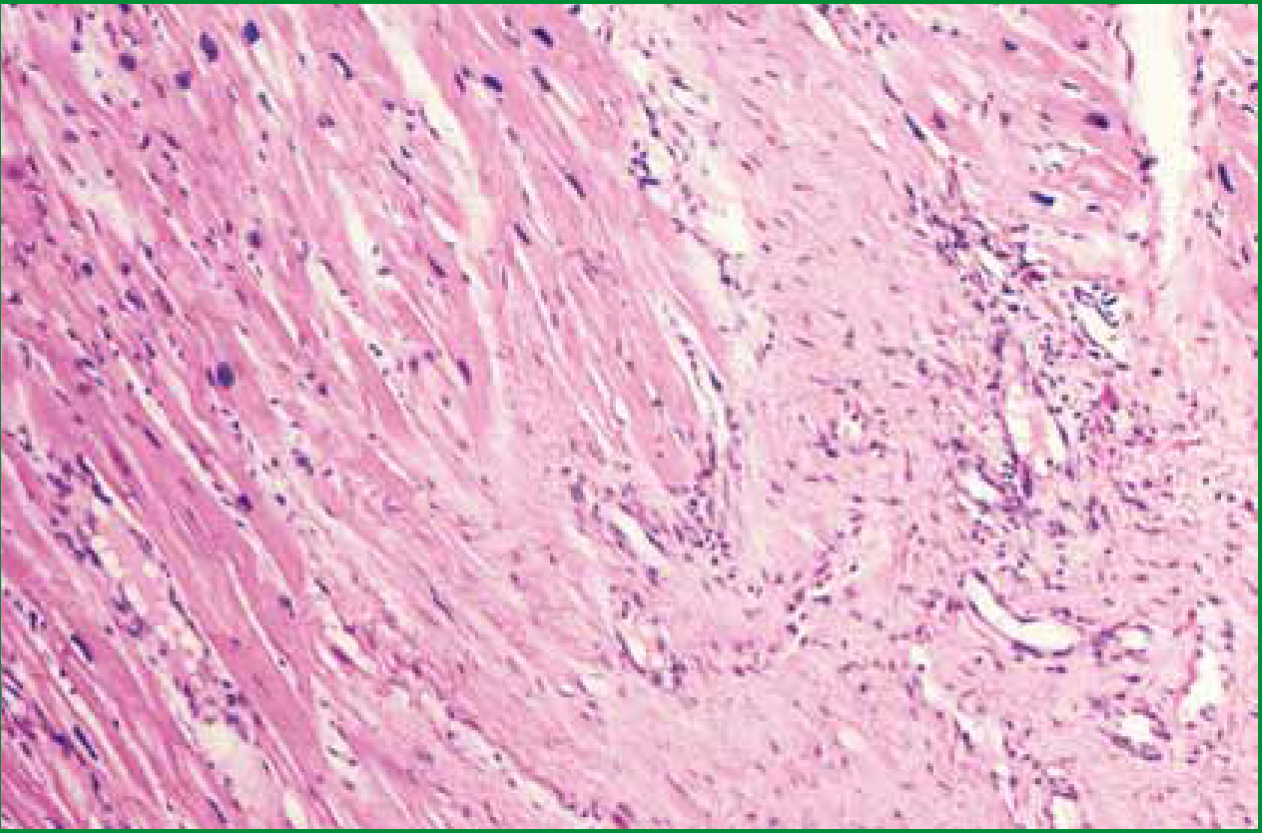
Although thrombolysis is an effective treatment for patients presenting with acute STEMI, both in terms of reducing mortality and preserving myocardial function, there are potential difficulties. Thrombolysis usually ‘dissolves’ the thrombus, restoring blood flow in the infarct-related artery, but it fails to open the vessel in a significant proportion of patients. In addition, in some patients, thrombolysis is successful in opening the blocked artery, but the vessel then re-occludes, usually associated with the recurrence of chest pain and changes on the ECG.
‘Ongoing education is required to try and keep the time from symptom onset to the call for help as reasonable as possible’
Finally, thrombolysis does not deal with the underlying stenosis in the coronary artery caused by the atheromatous plaque. This may result in ongoing symptoms of angina in the weeks following the acute event. There is also a small risk of bleeding associated with thrombolysis, which can be particularly serious if it results in cerebral haemorrhage. For this reason, thrombolysis is containdicated in some patients presenting with acute STEMI—for example, those who have recently undergone major surgery, those who have recently had gastrointestinal bleeding, and those with uncontrolled hypertension.
Primary percutaneous coronary intervention
In recent years, primary percutaneous coronary intervention (PCI) has been used more widely to treat patients with acute STEMI (Zijlstra et al, 1999; Keeley et al, 2003). This has the potential advantage of opening the infarct-related artery in a higher proportion of patients, dealing with underlying coronary artery plaque, and carrying a lower risk of major haemorrhagic complications.
During a primary PCI procedure, the occlusion in the infarct-related artery is crossed with a fine guide wire. A thrombectomy device is then usually advanced over the guide wire to the point of occlusion, enabling the thrombus to be aspirated. This device is then removed and the balloon/stent catheter is advanced over the guide wire enabling the stent to be deployed at the site of the occlusion.
With primary PCI, the same time pressures apply as with thrombolysis. It is important to transfer the patient to the heart attack centre either from their home or from the emergency department as swiftly as possible. It is then vital to take the patient to the catheter laboratory at the heart attack centre and restore flow in the infarct-related artery as quickly as possible—the ‘door-to-balloon’ time. Since many professional groups are involved in the care of a patient presenting with acute STEMI for treatment by primary PCI, to run such a service on a 24 hours/day and 7 days/week basis uses a considerable amount of resources (Zijlstra et al, 1999; Keeley et al, 2003).
There are ongoing studies comparing primary PCI with prehospital thrombolysis and PCI within the next 24 hours. In the second group of patients, PCI can be carried out between the hours of 9 am to 5 pm and in those who fail to reperfuse immediately after the thrombolysis, on the basis of the ECG changes failing to resolve, emergency PCI can be undertaken. The ongoing studies will compare the two groups in terms of clinical-effectiveness as well as cost-effectiveness.
Patient assessment
Patients usually enter the primary PCI service by one of the two routes. Some patients present themselves to an emergency department, while others call the emergency services to the scene, which usually is the patient's home. The patient must be assessed clinically and an ECG recorded. Following this, a decision needs to be made whether or not to transfer the patient to the nearest heart attack centre.
The clinical assessment involves the site and character of the chest discomfort. This is typically ‘crushing’ or ‘squeezing’ or ‘tightening’ and occurs across the front of the chest. It may be associated with breathlessness, sweating and nausea/vomiting. It is also important to establish any coexisting medical problems, since this may have an impact on their subsequent PCI procedure (for example, renal failure or peripheral vascular disease).
The time of onset of the symptoms is important to determine. The patient's heart rate, heart rhythm and blood pressure should be recorded. The ECG should be evaluated for the presence of ST segment evaluation, which is required for the diagnosis of STEMI.
If the patient has a good history of chest pain and has ST segment elevation on the ECG, he/she should be transferred immediately to the nearest heart attack centre. In patients where the history is not clear (for example no chest pain/or the ECG does not show ST segment elevation), it is usually more appropriate to take the patient to the nearest emergency department for more detailed assessment. Patients who have left bundle branch block can present a challenging problem. It is often not possible to determine whether the ECG changes are new or are longstanding.
The patient's history becomes even more important in this situation—is it suggestive of an acute myocardial infarction? If there is a suspicion of an acute infarction, it is usually most appropriate to transfer the patient to the nearest heart attack centre for further evaluation. It is important to administer adequate analgesia before the patient is transferred to hospital.
When the patient arrives at the heart attack centre, the clinical history may be further refined. It is important to consider other possible diagnoses, since these may require a different management strategy. Acute pericarditis usually presents with chest pain and ST segment evaluation on the ECG (Troughton et al, 2004). The chest pain is typically worse with inspiration and has a positional component (in that it is worse when lying flat).
In practice, it is still often necessary to take these patients to the catheter laboratory and perform a coronary angiogram in order to exclude acute coronary artery occlusion. Another diagnosis to consider is acute dissection of the thoracic aorta. These patients usually have a history of hypertension and their chest pain is typically ‘tearing’ in character and starts in the back between the scapulae (shoulder blades). If the dissection involves the ostium of one of the coronary arteries, the ECG will show the ST segment elevation seen in acute myocardial infarction.
If there is significant concern regarding the possibility of acute aortic dissection, it is usually best to carry out an emergency CT scan rather than proceeding with coronary angiography. If the CT scan confirms acute aortic dissection, the patient is usually referred for emergency cardiac surgery. If aortic dissection is excluded on the scan, the patient can then be taken to the catheter laboratory for coronary angiography.
The procedure
Once the infarct-related artery has been identified on the coronary angiogram, it is crossed with a guide wire, the thrombus is aspirated using a thrombectomy device, and the stent is deployed. In some patients, typically with an acute inferior STEMI, there may be profound bradycardia or evidence of atrio-ventricular block. In these cases, a temporary pacing lead can be advanced to the right ventricle via the femoral vein at the time of the cardiac catheter procedure. Some patients presenting with a STEMI have severe hypotension or cardiogenic shock.
In this situation, an intra-aortic balloon pump can be positioned to augment/support the circulation prior to the PCI being performed. If the patient has severe pulmonary oedema that does not respond to intravenous diuretics, they may require intubation and ventilation. Once a decision has been made to transfer the patient to a heart attack centre on the basis of his/her clinical assessment and ECG, anti-platelet therapy should be administered immediately. This is usually a combination of aspirin and clopidogrel.
‘Although thrombolysis is easy to administer, it is contraindicated in a significant proportion of patients presenting with acute STEMI’
A newer agent, prasugrel, can be used if the patient is intolerant of or allergic to clopidogrel. It may also be used instead of clopidogrel if the patient arrives in the catheter laboratory without receiving anti-platelet therapy, since it has a quicker onset of action than clopidogrel. During the PCI procedure, if there is a lot of intra-luminal thrombus present which cannot be aspirated using the thrombectomy device, a glycoprotein IIb/ IIIa inhibitor may be given intravenously. These agents, however, are expensive and carry an increased risk of bleeding.
Post procedure care
Following the emergency PCI procedure, the patient is transferred to a high-dependency unit. If they require mechanical ventilation, they will need to be admitted to an intensive care unit. The patients are subsequently transferred to a general cardiology ward for mobilization. Typically, the patients are discharged home after spending approximately 3 days in hospital. Cardiac rehabilitation forms an important part of the management of patients presenting with acute STEMI (Thompson et al, 2006). It has both an educational component and an exercise component.
The rehabilitation programme starts before the patient is discharged from hospital. A variety of medication is administered to patients presenting with acute STEMI. They are usually given aspirin for life and clopidogrel is typically given for 12 months following their stent procedure. A statin is also given life-long, which will reduce the cholesterol level and also reduce the risk of rupture of any residual coronary artery plaques (Thompson et al, 2006).
The statins produce ‘plaque-stabilization’ and thereby reduce the risk of acute coronary events in the future. The other drugs which are routinely administered following acute STEMI are the P-blockers and the angiotensin-converting enzyme (ACE) inhibitors (Thompson et al, 2006).
Conclusion
It is clear that the management of patients presenting with acute STEMI has changed in recent years. Although thrombolysis is easy to administer, it is contraindicated in a significant proportion of patients presenting with acute STEMI. In some patients, thrombolysis fails to open the occluded artery while in others the vessel can re-occlude. In addition, it does not deal with the underlying stenosis in the infarct-related artery.
Primary PCI is now being used more widely in patients presenting with acute STEMI. It is more effective than thrombolysis in opening the occluded artery and it treats the underlying stenosis in the vessel. Primary PCI is associated with fewer haemorrhagic complications than thrombolysis and may also reduce mortality in patients presenting with acute STEMI. Since a primary PCI service is more complex to deliver than a prehospital thrombolysis service, it uses more resources.
The findings of cost-effectiveness studies comparing the two treatments, which are currently ongoing, are awaited with interest. These include the STREAM study, which is a multicentre multinational trial (Armstrong et al, 2010). Patients with STEMI are randomized to either primary PCI or to prehospital thrombolysis and PCI within the next 6-24 hours, and mandated rescue PCI for those patients who fail to reperfuse on their 90 minute ECG. The trial compares the two treatment strategies from both the clinical-effectiveness and the cost-effectiveness viewpoint (Armstrong et al, 2010).
