The identification and treatment of acute coronary syndrome (ACS) is a priority for Australian paramedics. ACS refers to a group of conditions that affect coronary blood flow and includes unstable angina and acute myocardial infarction (MI), which is diagnosed as either ST-elevation MI (STEMI) or non-ST-elevation MI (NSTEMI) (Bhatt et al, 2022). The acquisition and interpretation of a 12-lead ECG is considered the gold standard for early identification and management of ACS in the prehospital setting (Prihatiningsih and Hutton 2018). This is associated with significant reduction in time to definitive treatment without adversely increasing prehospital scene times (Mobrad 2020; Alrumayh et al, 2022). Where STEMI is misdiagnosed, mortality increases from 2% to 25.9% (Dee et al, 2022).
Recent advances in ECG interpretation have led to the finding that up to 28% of NSTEMIs present with a complete coronary occlusion and may be detected on an ECG (McLaren et al, 2022).
Because accurate interpretation has a profound impact on patient care and outcome, recent literature suggests that investigations into paramedic ECG interpretation are warranted (Funder et al, 2022).
Although local guidelines and protocols may vary between Australian jurisdictional ambulance services, these organisations employ two pathways for the management of STEMI. Where transport times to hospitals with percutaneous coronary intervention (PCI) capabilities are >60 minutes, the pathway is prehospital thrombolysis (Khan et al, 2020). If the transport time is <60 minutes, the second pathway is that patients are to be directly conveyed to a PCI centre (Khan et al, 2020).
These pathways are primarily activated and achieved through decision-support software algorithms to identify a STEMI, with the ECG then transmitted to a physician for confirmation (Faour et al, 2022). There are limitations to software support as these algorithms have a false negative rate of 1–7% for STEMI and may not identify an NSTEMI (Bosson et al, 2017; Faour et al, 2022). However, some paramedic specialists are authorised to perform prehospital thrombolysis and PCI referral through autonomous decision-making without software recognition or physician confirmation of a STEMI (Doan et al, 2020). A specialist is a paramedic who has reached a higher clinical level through additional education and training within a jurisdictional ambulance service; they are known as intensive care or critical care paramedics.
These intervention strategies are essential to ensuring improved patient outcome (Khan et al, 2020). This occurs through a reduction in morbidity and mortality for patients experiencing an acute MI through the resolution of the coronary obstruction (Faour et al, 2022). Where these strategies fail, patients may experience permanent cardiac injury (Alrumayh et al, 2022; Liao et al, 2022). In addition to this, where the PCI centre is inappropriately activated, there is a significant financial and fatigue burden on the hospital system (Shoaib et al, 2022).
Following an extension to the paramedic scope of practice in 2016, all paramedics have the capability to identify a STEMI (Alrawashdeh et al, 2020; Doan et al, 2020; Funder et al, 2020). Before this, STEMI identification was performed by specialist paramedics only (Alrawashdeh et al, 2020; Doan et al, 2020).
Although specialist autonomous decision-making pathways exist and paramedics are not discouraged from transmitting ECGs that do not meet STEMI criteria, no recent literature has explored Australian paramedic ECG interpretation (Funder et al, 2020).
With increases in the paramedic scope of practice in Australia and higher education requirements, it is pertinent to investigate and determine whether Australian paramedics can accurately perform ischaemic ECG interpretation. This may ultimately prevent potential adverse outcomes that could otherwise have been mitigated through ECG recognition.
Aims
The aim of this study was to investigate and assess Australian paramedic accuracy in ECG interpretation related to ischaemic ECG changes, specifically STEMI, NSTEMI and STEMI mimics.
The study investigated: whether there were there any differences within the data regarding educational background and paramedic clinical levels; and how collected data compared with existing international literature.
Methods
Study design and enrolment
The research involved a cross-sectional cohort study of Australian paramedics registered with the Australian Health Practitioner Regulation Agency (AHPRA) and working for an Australian jurisdictional ambulance service. Ethical approval was gained from Charles Sturt University (CSU) (H23749), with all procedures performed in compliance with the protocol as well as with institutional and committee guidelines.
Participants were recruited through voluntary response sampling, with the study advertised on Australian paramedic Facebook page Paramedic Good Karma Network. Consent was obtained at the start of the survey. The survey was distributed via online tool SurveyMonkey and was accessible between 18 July 2023 and 2 August 2023. It included questions on educational background, experience and practising clinical level. Participants were required to interpret 12 12-lead ECGs. They were given the choice of four options to select from:
The ECGs selected included three cases of STEMI (inferior, lateral and anterior), three mimics (left ventricular hypertrophy (LVH), left bundle branch block (LBBB) and pericarditis), two normal sinus rhythms (NSR) and four NSTEMI cases (DeWinter T-wave, aVR elevation, posterior acute MI and Smith-Modified Sgarbossa positive (paced) ECG). The LBBB presented was classed as a STEMI mimic as it did not meet occlusion MI criteria and no history was provided. Similarly, while a paced ECG is considered a STEMI mimic, as the ECG meets Smith-Modified Sgarbossa criteria, the correct response for this survey was NSTEMI. The ECGs were classed based on the STEMI versus NSTEMI paradigm. As the NSTEMI ECGs technically did not meet STEMI criteria, they were classed as NSTEMI to fit within the paradigm used in this survey. This paradigm is familiar to Australian paramedics and is reflected within the clinical practice guidelines of jurisdictional services.
Subjects and sample size
The last report issued by the (Australian) Department of Health (2019) showed that there were 15 115 employed paramedics working as clinicians for a jurisdictional service in Australia. Using this number, for a confidence index of 95% and margin of error of 5%, the SurveyMonkey sample size calculator recommended 375 respondents. Three hundred and ninety-seven paramedics were anonymously and voluntarily recruited. Participants had to be AHPRA registered Australian paramedics working for an Australian jurisdictional ambulance service. They were asked to provide their highest level of education, with 39 reporting a diploma or vocational pathway, 284 having a bachelor's degree and 74 holding a postgraduate qualification. Of these participants, 337 were paramedics and 60 were paramedic specialists. Details regarding sex, age, ethnicity or employer were not collected.
Data analysis
The data were downloaded from SurveyMonkey and uploaded into an Excel spreadsheet.
Responses from the entire sample on educational background and clinical level were descriptively analysed. The data were calculated and presented into simple counts and displayed as percentages. Online tools were used to assess the sensitivity, specificity and accuracy for each cohort. A comparative-descriptive analysis was performed to establish whether the results for Australian paramedics correlated with the findings from international studies.
Search criteria were carried out using CSU's servers and National Center for Biotechnology Information (NCBI) and criteria applied using the synonyms and keywords ‘paramedic’, ‘ECG’, ‘interpretation’, ‘recognition’, ‘diagnosis’, ‘Australia(n)’, ‘electrocardiogram’, ‘STEMI’, ‘myocardial infarction’, ‘New South Wales’, ‘Victoria’, ‘Queensland’, ‘South Australia’, ‘Western Australia’, ‘Tasmania’ and ‘ambulance’, and were limited to peer-reviewed English language sources. For international literature, keywords excluded the nouns pertaining to Australia.
Results
The survey revealed that paramedics commonly have difficulty differentiating between STEMI and STEMI mimics. This was most evident when misdiagnosing a mimic as a STEMI (Table 1). ECGs that were ischaemic but did not meet STEMI criteria were conversely misdiagnosed as a STEMI mimic (Table 1).
| Electrocardiogram | Percentage correct | Most misdiagnosed as |
|---|---|---|
| Inferior STEMI | 98.49% | STEMI mimic: 1.26% |
| NSR (1) | 91.94% | STEMI mimic: 4.53% |
| Anterior STEMI | 89.67% | STEMI mimic: 9.32% |
| NSR (2) | 86.90% | STEMI mimic: 5.29% |
| Lateral STEMI | 83.12% | STEMI mimic: 12.88% |
| LBBB | 72.54% | STEMI: 19.75% |
| aVR elevation | 62.47% | STEMI: 19.14% |
| Posterior AMI | 51.39% | STEMI: 22.47% |
| LVH | 49.12% | STEMI: 33.50% |
| DeWinter T-wave | 44.33% | STEMI mimic: 37.12% |
| Pericarditis | 23.67% | STEMI: 42.13% |
| Smith-Modified Sgarbossa positive (paced) ECG | 2.77% | STEMI mimic: 73.80% |
AMI: acute myocardial infarction; ECG: electrocardiogram; LBBB: left bundle branch block; LVH: left ventricular hypertrophy; NSR: normal sinus rhythm; STEMI: ST-elevated myocardial infarction
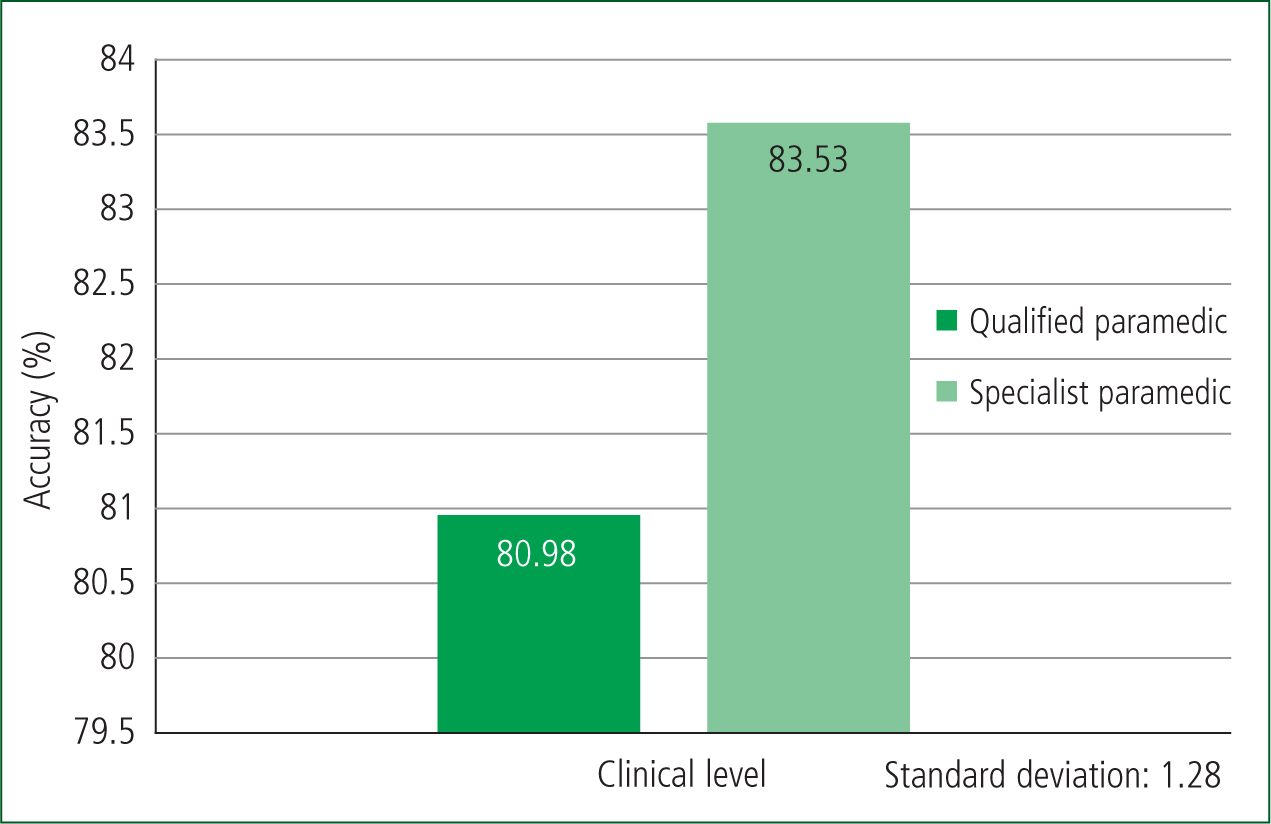
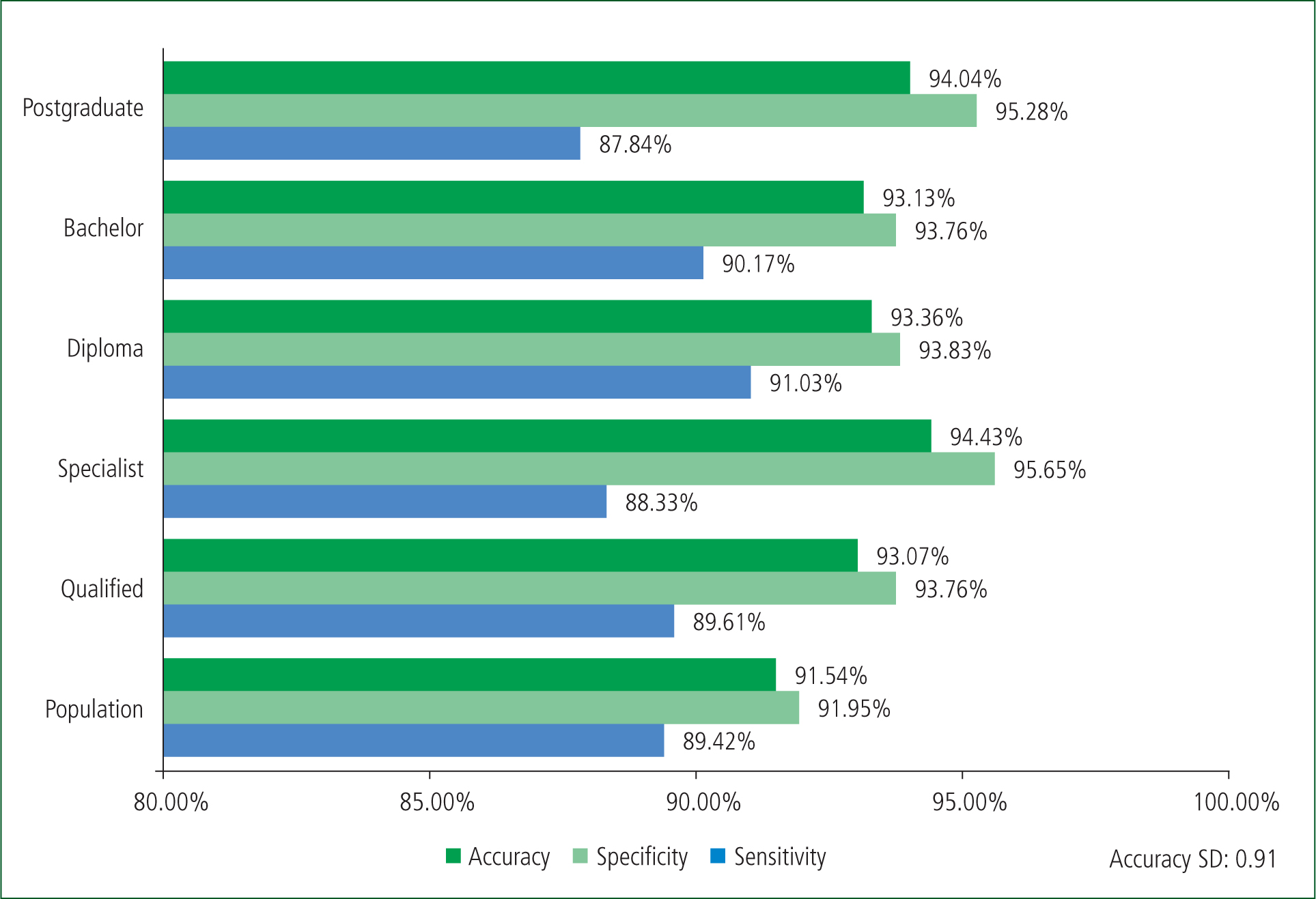
A clear trend for accuracy is noticeable within the results. Specialist paramedics scored higher than their qualified counterparts in all fields with a higher mean accuracy (Figure 1).
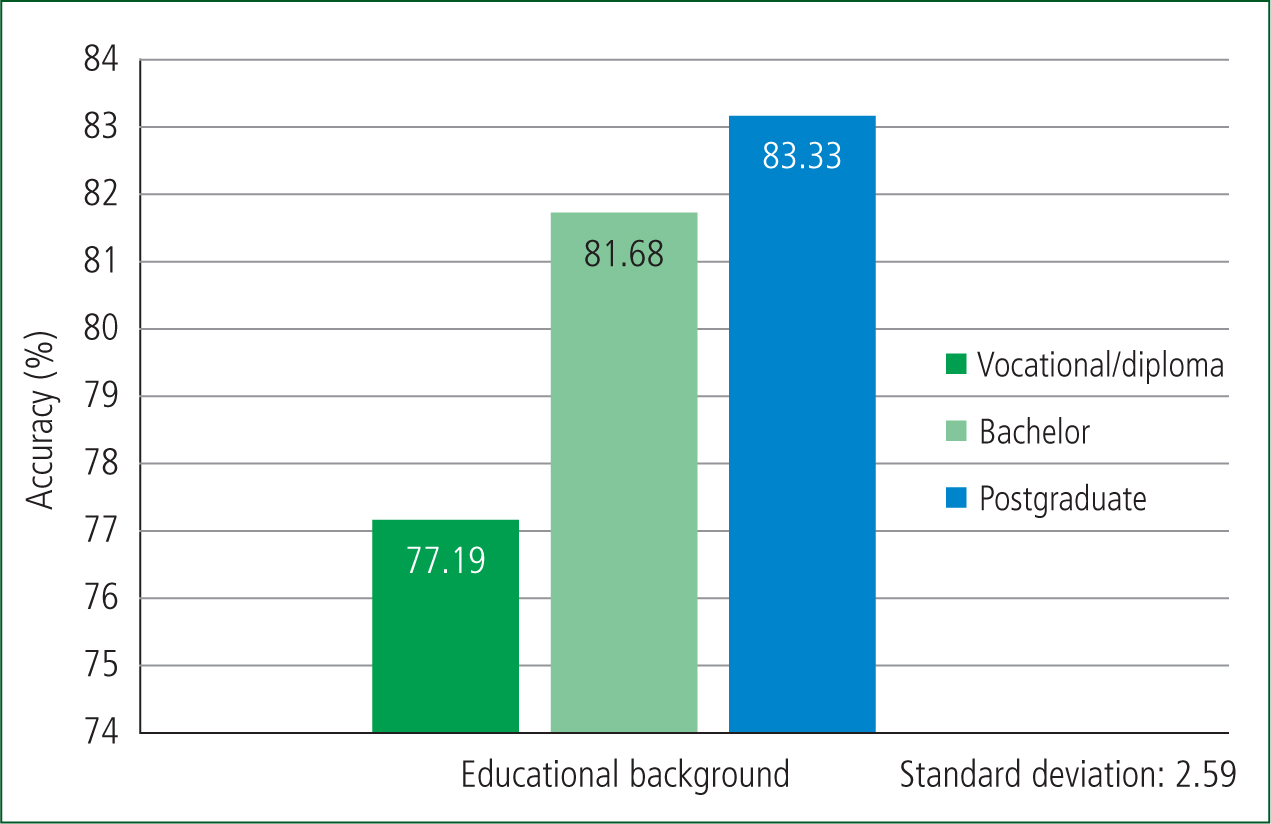
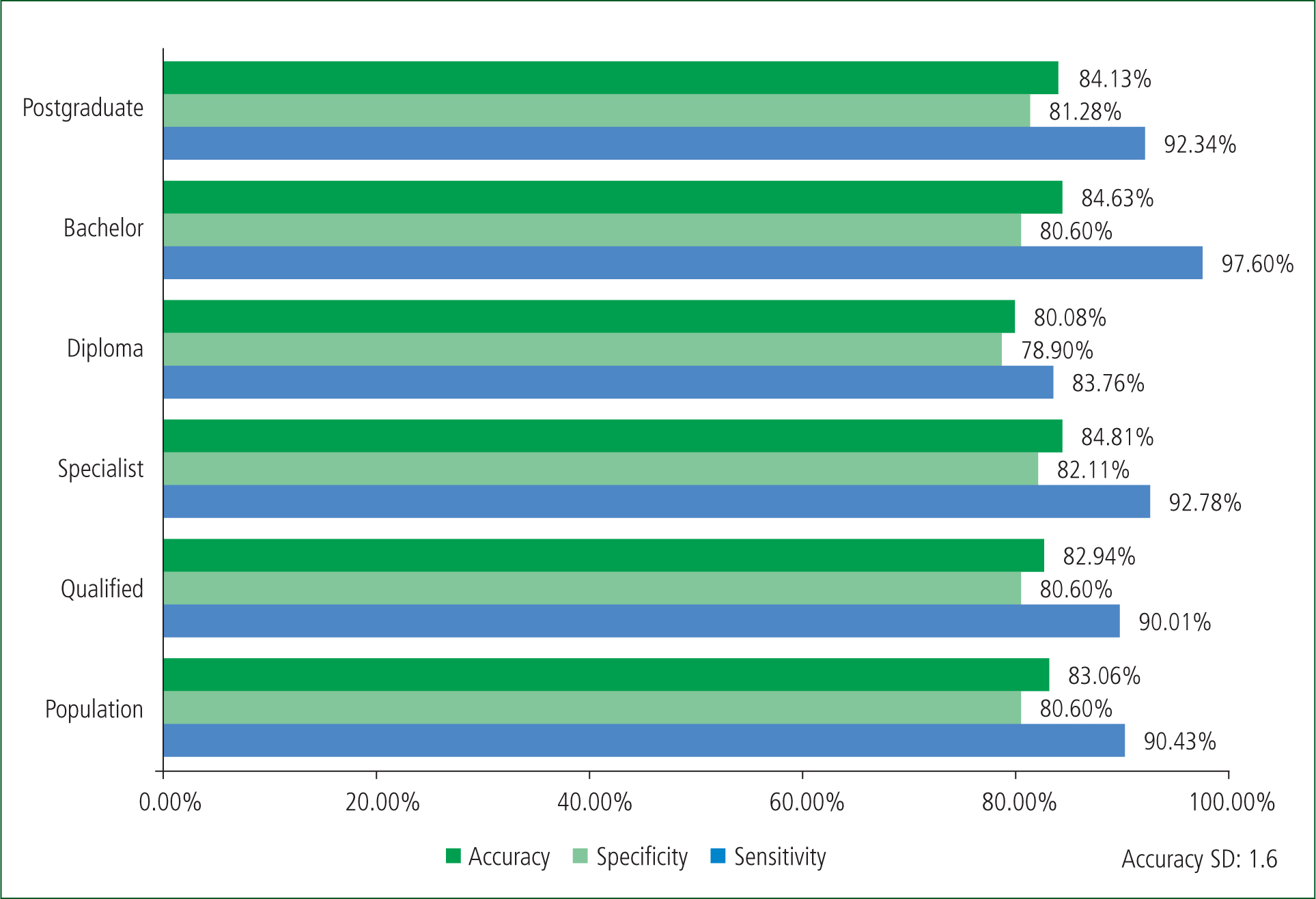
Similarly, higher levels of education were associated with higher accuracy scores, with the greatest difference between the diploma and postgraduate cohorts (Figure 2). Postgraduate paramedics overall were more accurate than those with bachelor's degrees; however, bachelor's qualified paramedics were 0.5 more percentage points accurate than postgraduate for STEMI identification (Figure 3).
Discussion
Paramedic interpretation
The mean correct response of 63% (Table 2) contrasts with a similar study conducted by Pilbery et al (2016), where 80% of English and Welsh paramedic participants were correct in their ECG interpretation. However, the results of this current study had a significant outlier, with 97.23% of participants incorrectly diagnosing the Smith-Modified Sgarbossa positive (paced) ECG (Table 1). Conversely, no outliers were declared in the study conducted by Pilbery et al (2016).
| Mean | 7.56/12 (63%) |
| Median | 8 (66%) |
| Range | 3–12 |
| Standard deviation (SD) | 1.69 |
A review of the literature found no studies that compared different paramedic clinical levels. Literature is contentious, with mixed conclusions regarding whether or not there are discernible patterns such as educational background or experience and how these may influence paramedic ability to accurately interpret ECGs (Sharp, 2017; Zègre-Hemsey et al, 2020; Alrumayh et al, 2022).
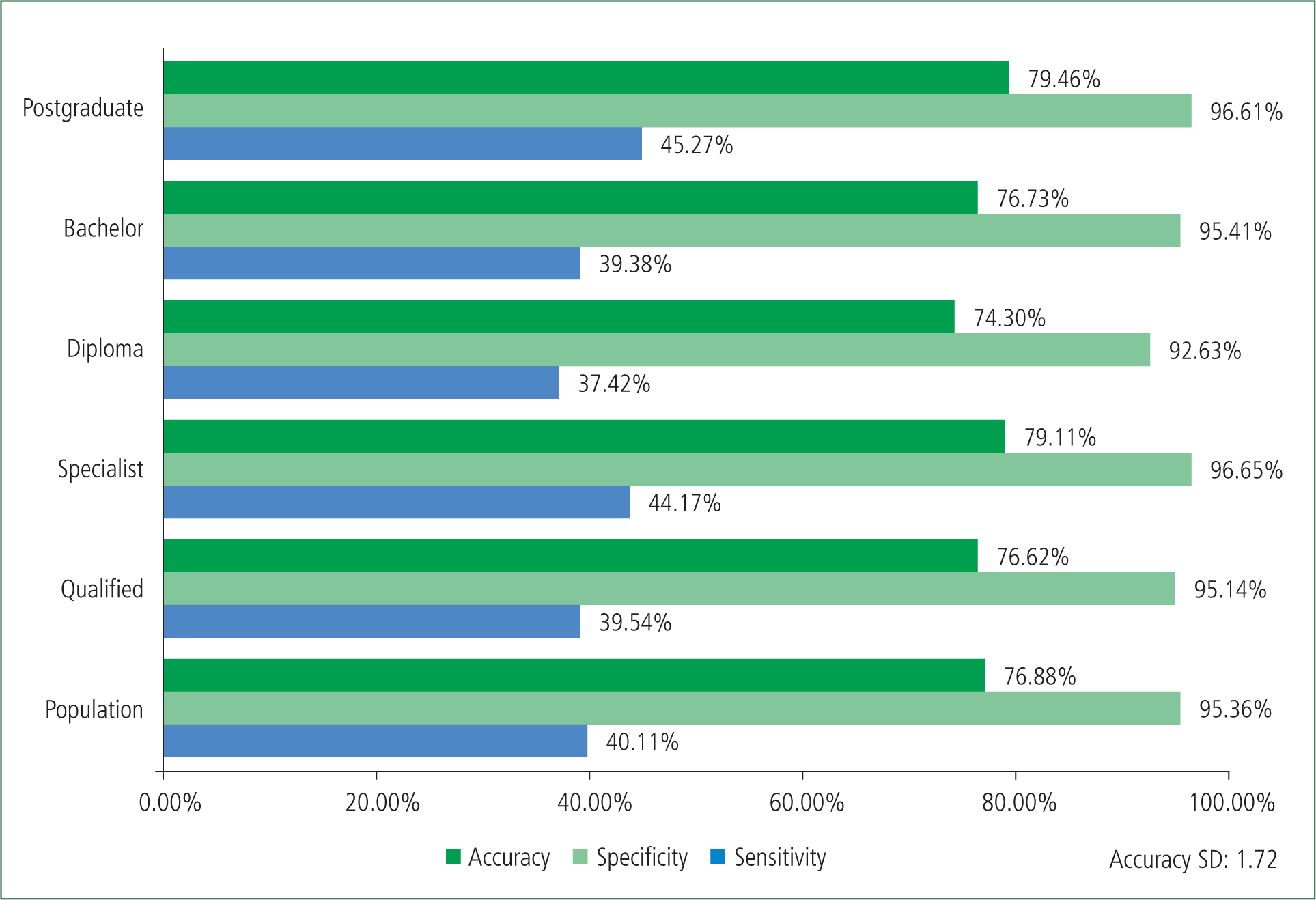
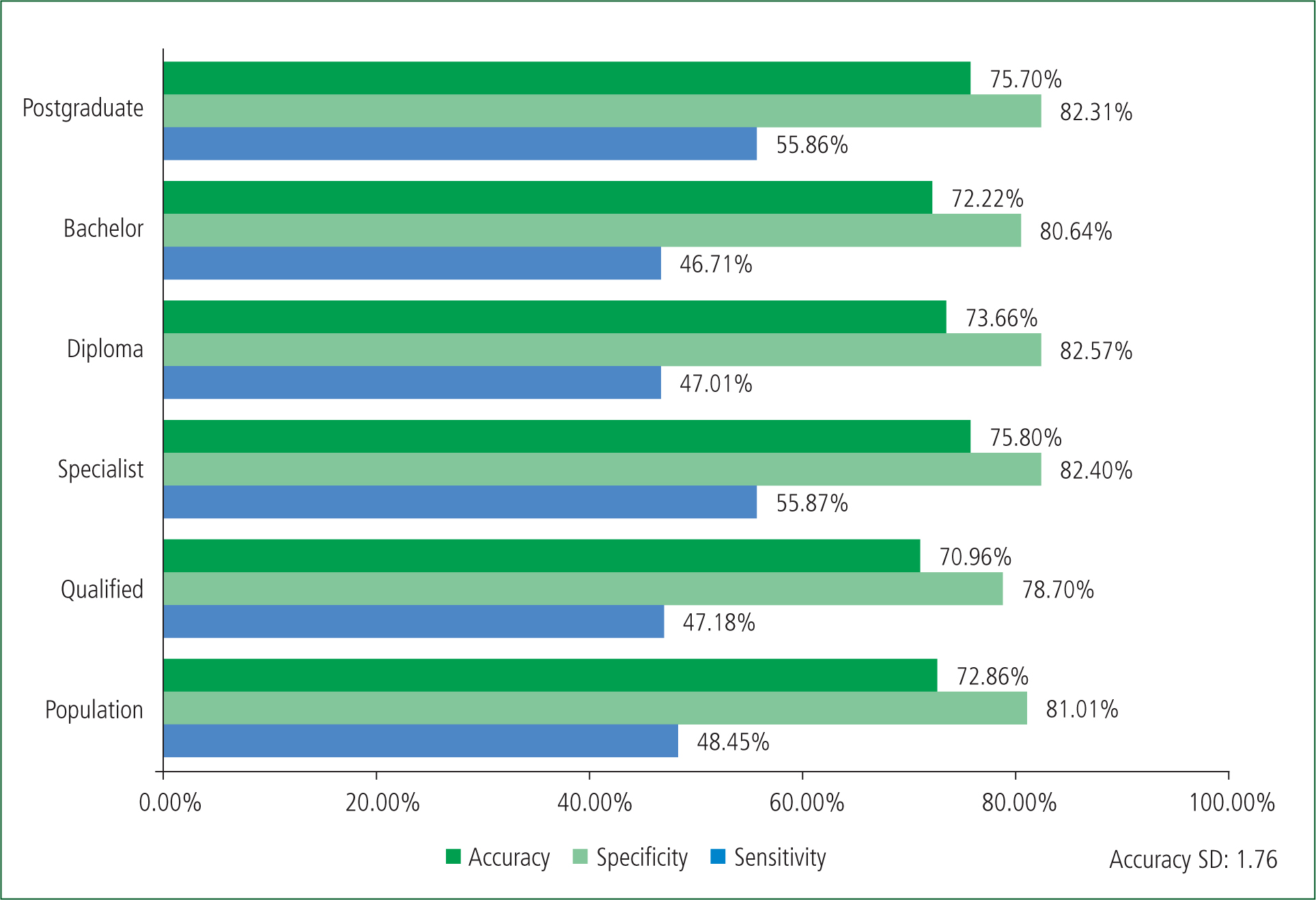
The results from this study suggest there is a correlation between higher education and an increase in accuracy of NSTEMI interpretation (Figure 4). Similar conclusions have been made in other studies assessing paramedic interpretation of ECGs (Prihatiningsih and Hutton, 2018; Mobrad 2020).
Normal sinus rhythm
There is limited evidence for paramedic interpretation of NSR as the literature traditionally focuses on STEMI identification.
However, a study conducted in Saudi Arabia investigated paramedic ability to interpret STEMI against STEMI mimics and NSRs (Alrumayh et al, 2022). The study found that the two NSRs presented were answered correctly by 72.3% and 47.9% of participants respectively (Alrumayh et al, 2022). The most common misdiagnoses were STEMI at 4.6% and right bundle branch block at 12.7% (Alrumayh et al, 2022).
This is in stark contrast to the results in this study (Table 1 and Figure 5), with paramedics correctly identifying NSR (1) and NSR (2) at 91.94% and 86.90% with high accuracy. The commonest misdiagnosis for the two was STEMI mimic (Table 1).
ST-elevation myocardial infarction
These results contrast significantly with a previous Australian study conducted in 2009, where the authors concluded that specialist Victorian paramedics could identify a STEMI 58% of the time (Hutchison et al, 2009). This result was concluded from all ECGs transmitted to Victorian hospitals that were positively identified as meeting STEMI criteria (Hutchison et al, 2009). Likely contributing to skewed figures is the fact that paramedics were not discouraged from transmitting suspicious ECGs not meeting STEMI criteria (Hutchison et al, 2009).
Software recognition plays a significant role in the diagnosis of a STEMI. While dependent on the software or machine used, the sensitivity for STEMI identification ranges between 35% and 96% and is 90–100% specific (Pilbery et al, 2016; Bosson et al, 2017; Coffey et al, 2018; Hillinger et al, 2019). Despite this apparent significant range, the majority of these sources report both sensitivity and specificity are both >90%. False negatives for software identification of STEMI may range from 1% to 7%, though these figures may be under-reported (Bosson et al, 2017; Coffey et al, 2018; Faour et al, 2022). As shown in Table 3, this correlates with the false negative rate found in this study of 2.8%. Of note, the high sensitivity and specificity for software interpretation were found or reported in studies performed in hospitals, where ECGs are generally of better quality than those performed prehospitally (Faour et al, 2022; Pilbery et al, 2016). This is significant as a leading cause of prehospital software misinterpretation is artefact (Bosson et al, 2017).
| Diagnosis | False positives | False negatives |
|---|---|---|
| STEMI | 19.4% (adjusted 11.6%) | 2.8% |
STEMI: ST-elevation myocardial infarction
Adjustment made to the false positive total to exclude non-STEMI diagnosis and include only non-ischaemic electrocardiograms (ECGs)
The data collected in this survey reflect results found in other international studies. North American and European studies have concluded that paramedics could identify STEMI ECGs with a high sensitivity and specificity. The results of these studies had ranges of 80–97% sensitivity and 85.4–97% specificity (Prihatiningsih and Hutton 2018; Zègre-Hemsey et al, 2020; Sibley et al, 2021).
A recent systemic review highlighted that paramedics could identify a STEMI between 58% and 99% of the time, with a mean of 83%, a stark contrast to the 90.43% sensitivity shown in Figure 3 (Funder et al, 2020). Of note, a New Zealand (NZ) study concluded that the NZ St John Ambulance Service had a STEMI identification rate of 50.7% (Liao et al, 2022). This research found that patients whose STEMI was missed had a three times greater mortality rate than those correctly diagnosed (Liao et al, 2022).
For STEMI sensitivity, Australian paramedics perform similarly to their North American and European counterparts, with comparable results to those reported by software interpretation. However, as shown in Figure 3, the population specificity for STEMI interpretation of 80.60% was lower than the reported international lower range of 85.4% (Alrumayh et al, 2022). The closest Australian demographics to this range were the bachelor qualified cohort at 84.63% and postgraduate cohort at 84.13% (Figure 3).
Non-ST-elevated myocardial infarction
The four ECGs classified as NSTEMI were selected as they reflect a cohort of high-risk patients likely to require urgent reperfusion and are known to be misdiagnosed prehospitally (Hillinger et al, 2019; Palladino et al, 2021; Faour et al, 2022). With advances in ECG interpretation and increasing awareness of occlusion MI criteria, there is a growing recognition of NSTEMI patients requiring urgent cardiac services for total coronary occlusions (McLaren et al, 2022).
This has coincided with a Dutch ambulance service modifying its cardiac protocol to enable paramedics to transport suspected NSTEMI patients to a PCI-capable hospital (Anroedh et al, 2018). This resulted from a recognition that software is limited for NSTEMI interpretation as it poorly identifies ST depression, abnormalities in the ST/T ratio and T-wave morphology (Bosson et al, 2017; Anroedh et al, 2018; Faour et al, 2022). Software is therefore less likely to identify an NSTEMI, which is linked with delayed activation of the receiving PCI centre and subsequent adverse outcomes (Faour et al, 2022; McLaren et al, 2022)
The results highlighted that paramedics' accuracy for NSTEMI interpretation varies. The most correctly identified NSTEMI at 62.47% was aVR elevation, with misdiagnosis of STEMI at 19.14% and overall ischaemic recognition of 81.61% (Table 1).
Similarly, posterior acute MI was correctly identified at 51.39% with a misdiagnosis of STEMI at 22.47% and an overall ischaemic recognition of 73.86% (Table 1). It is difficult to determine whether this was owing to the later rhythm being defined as a STEMI equivalent (Hillinger et al, 2019). For consistency in the ECGs, the posterior leads were not supplied for this ECG and therefore the definition is acknowledged as being broad. However, as Table 1 shows, DeWinter T-waves, another defined STEMI equivalent, were most frequently misdiagnosed as a STEMI mimic (Hillinger et al, 2019).
The Smith-Modified Sgarbossa criteria (ST/T ratio >25% and/or concordant ST elevation >1 mm and/or concordant ST depression >1 mm in V1–V3) may be used to determine the presence of an acute MI within a LBBB or paced rhythm (Faour et al, 2022; McLaren et al, 2022). At 2.77%, the Smith Modified Sgarbossa positive (paced) ECG was the least correctly identified ECG (Table 1).
Participants correctly identified NSTEMI with varying results. However, they recorded a specificity of 95.36%—the highest result for specificity in all results (Figure 4).
ST-elevation myocardial infarction mimic
A paucity of literature exists regarding paramedics' ability to interpret STEMI mimics. However, a body of literature describes common ECGs that are linked with misdiagnosis and false positives for STEMI.
Leading causes for false positives in the prehospital environment are STEMI mimics, in particular pericarditis, LBBB and LVH (Alrumayh et al, 2022; Bosson et al, 2017; Faour et al, 2022). Of note, pericarditis is frequently mentioned within the literature as a common cause for inappropriate PCI centre activations (Shoaib et al, 2022). This is reflected in the results, with 23.67% correctly identifying pericarditis; however, 42.13% misdiagnosed this as a STEMI (Table 1). Similarly, LVH and LBBB were also misdiagnosed as STEMI at 33.50% and 19.75% respectively (Table 1).
Additionally, an outlier emerged with paramedics identifying paced rhythm as positive for Smith Modified Sgarbossa, primarily as a STEMI mimic. While the most correctly recognised STEMI mimic was LBBB at 72.54%, the paced rhythm was also identified as a STEMI mimic by 73.80% of respondents (Table 1). This raises further questions regarding interpretation of STEMI mimics, STEMI and knowledge surrounding Smith-Modified Sgarbossa criteria.
The false positive rate for STEMI within this study was 19.4% (Table 3). However, included in this rate of 19.4% is the NSTEMI diagnosis that may require PCI centre activation. The adjusted value for this to account for only STEMI mimics is 11.6% (Table 3).
Closely linked with software interpretation is a high PCI centre cancellation rate of 41–65% (Zègre-Hemsey et al, 2020; Faour et al, 2022). Conversely, prehospital false positive rates in Perth, Australia, that led to a PCI centre activation are as low as 2.75% (Shoaib et al, 2022).
The qualified paramedics identified STEMI mimics with the least accuracy in this sample, a finding that correlates with existing literature (Bosson et al, 2017; Alrumayh et al, 2022; Faour et al, 2022) (Figure 6).
Recommendations
Further research is required to explore difficult-to-interpret ECGs and determine discrepancies between sensitivity and specificity. Institutions may consider further and targeted education for Australian paramedics to increase interpretation accuracy.
In line with the findings by Anroedh et al (2018) and because of the high specificity, Australian paramedic services may wish to consider exploring the implementation of a modified protocol to transport suspected NSTEMI patients to PCI-capable hospitals.
Limitations
The participants were not supervised, and their reported demographics could not to be verified. As services were not identifiable, actual results may differ between them because of potential variations between service-specific protocols, guidelines and scopes of practice.
Similarly, results show the performance of this sample size only and larger recruitment would give greater insight.
The survey was designed using the STEMI versus NSTEMI paradigm which has known limitations.
As data collection was limited to a multiple-choice diagnosis, it could not allow for deeper analysis.
There is a potential for ECG misinterpretation as no patient history was provided within the survey.
Additionally, confusion surrounding terminology may have existed and impacted on results.
Future research may consider the involvement of ambulance services, consider options for written analysis and include occlusion MI criteria.
Conclusion
Within this sample, higher clinical level and higher levels of education correlated with greater accuracy in interpreting ECG.
Consistent with international paramedic interpretation of STEMI, Australian paramedic identification results are similar and exceed existing evidence for NSR.
The findings of this study correlate with current literature that concludes that paramedics have difficulty in interpreting STEMI mimics. Despite a low sensitivity for NSTEMI identification, paramedics had a high specificity.

