LEARNING OUTCOMES
After completing this module, the paramedic will be able to:
Cardiovascular disease is a major cause of mortality worldwide, and is directly related to the development of acute coronary syndrome (ACS) and ST-elevation myocardial infarction (STEMI) (Jiang et al, 2015). Globally, cardiovascular diseases (CVDs) are the number one cause of death (World Health Organization, 2017). Within the 17.5 million individuals who die from CVDs, four out of five deaths are caused by heart attacks and strokes (World Health Organization, 2017). Approximately 30% of patients with ACS experience STEMI, which is associated with a 5–15% inhospital mortality rate (André et al, 2014; Vercellino, 2017: 2).
Platelet aggregation and subsequent formation of a thrombus are pertinent components of STEMI development, and this highlights the importance of pharmacological platelet inhibition in the treatment of this condition (Jiang et al, 2015; US Food and Drug Administration (USFDA), 2019).
At present, the optimal treatment for STEMI includes early administration of aspirin, glyceryl trinitrate (GTN), a P2Y12 antagonist (ticagrelor, prasugrel or clopidogrel) and an anticoagulant (such as unfractionated heparin or enoxaparin), which is complemented by primary percutaneous coronary intervention (PPCI) or tissue plasminogen activator (tPA) administration (Jiang et al, 2015; Chew et al, 2016; Sealy et al, 2020). Often these treatments are delivered through interdisciplinary partnerships between paramedics, physicians and interventional cardiologists (Khan et al, 2016; Johnson et al, 2015: 372–373).
| Clopidogrel |
|
| Indications |
|
| Contraindications |
|
| Mechanism of action |
|
| Route of administration |
|
| Dose (adult) | Average doses across global ambulance services |
| Adverse effects |
|
Sources: New South Wales Ambulance (2018); Queensland Ambulance Service (2018); St John Ambulance New Zealand (NZ) (2019); Wellington Free Ambulance (2019); MIMSOnline (2020)
Clopidogrel is the most common P2Y12 receptor antagonist administered for STEMI management; it prevents platelet degranulation and, therefore, inhibits platelet aggregation. It is a second-generation P2Y12 receptor antagonist that actively impedes the binding of adenosine diphosphate (ADP) to the platelets' surface receptors, preventing the subsequent activation of ADP-mediated glycoprotein IIb/IIIa (Johnson et al, 2015: 372; MIMSOnline, 2020). This prevents the inhibition of cyclic adenosine monophosphate driven calcium storage, increasing the upload of calcium into the platelet dense tubular system—a membrane system that plays a pivotal role in the modulation of platelet aggregation (Gerrard et al, 1978). This prevents platelet shape transformation and degranulation events that occur in blood clotting, and therefore inhibits platelet congregation and further formation of a thrombus in the patient with STEMI (Maynard, 2019).
Pharmacokinetically, the drug has a rapid absorption rate and can reach peak plasma within 45 minutes of dosing (USFDA, 2019). The half-life is approximately 6 hours (USFDA, 2019).
As a prodrug, clopidogrel is absorbed through the gastrointestinal system, metabolised by the liver and experiences the first pass effect. The activated metabolite (clop-AM) binds antagonistically to the platelet receptors, inhibiting platelet degranulation and aggregation for the remainder of the platelet's lifespan, which is approximately 5–10 days (Karaźniewicz-Łada et al, 2014; Jiang et al, 2015; USFDA, 2019).
Despite multiple studies and trials indicating its effectiveness, such as the CAPRIE (CAPRIE Steering Committee, 1996), CURE (Mehta et al, 2001), CLARITY (Sabatine et al, 2005), and COMMIT study (Bhala and Taggar, 2006), only a small number of statutory ambulance services internationally have incorporated clopidogrel into their STEMI management regimens (Dhillon, 2015: 52; MIMSOnline, 2020).
The purpose of this report is to examine peer-reviewed articles and clinical practice guidelines relating to prehospital clopidogrel administration, and explore whether this drug should be more widely used across international ambulance services.
Methods
A literature search of the EBSCOHost (Health) group of journal databases, PubMed, Scopus and the Cochrane Library was undertaken. The primary search terms used were clopidogrel, pre-hospital*, ST-elevation myocardial infarction and antiplatelet. Secondary searches included ticagrelor, thrombolysis and acute coronary syndromes. The filters assigned to each search were: full text; peer reviewed; and published between 2005 and 2020. Boolean operators were used to link keywords. Figure 1 shows the search method and results.
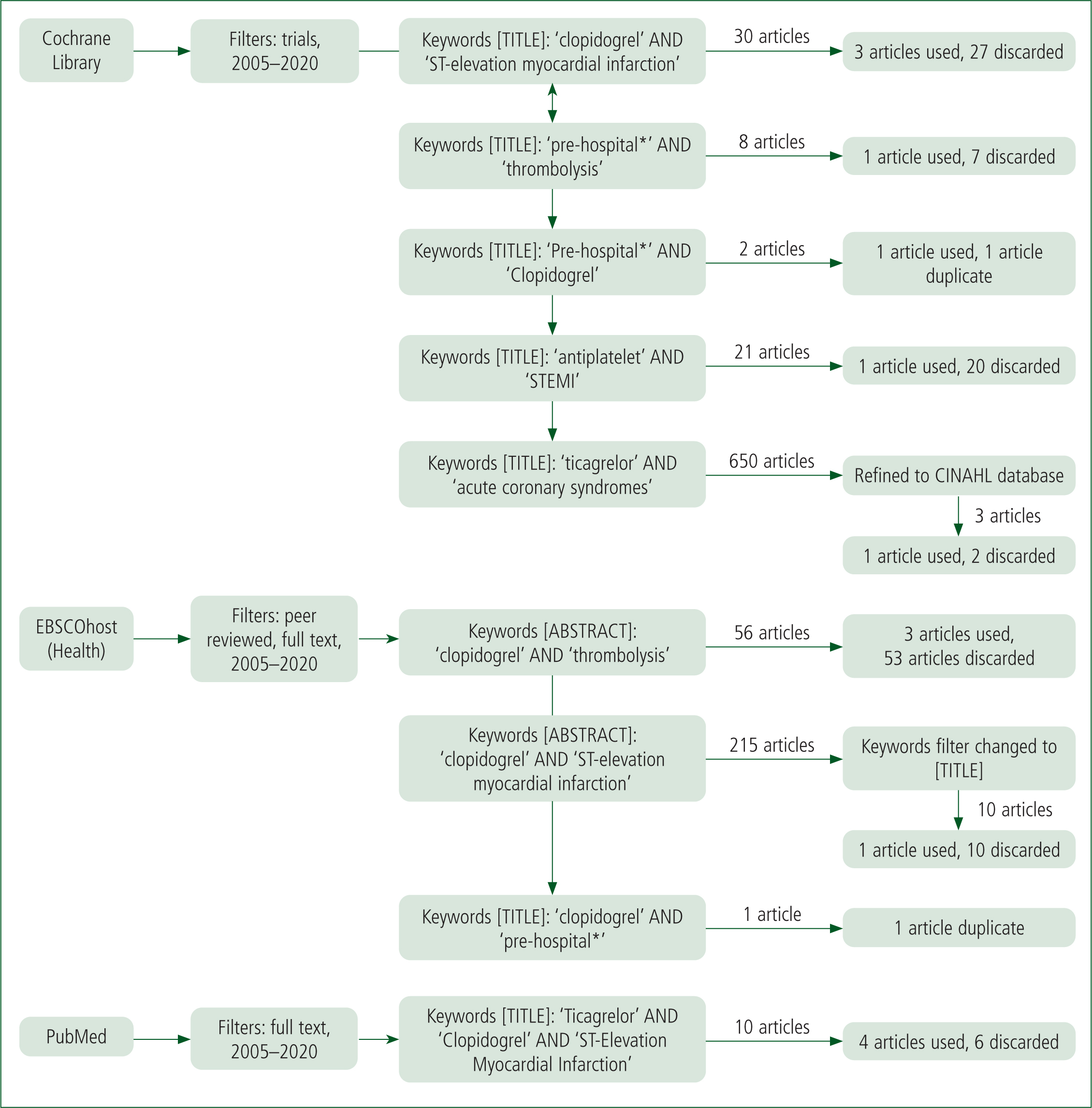
Duplicate articles were removed. Fourteen studies were retained.
Where available, clinical practice guidelines relevant to clopidogrel and thrombolysis were obtained from international ambulance jurisdictions. Of the 12 guidelines reviewed in this study, eight advocated clopidogrel use within their cardiac thrombolysis regimes (Table 2).
| International ambulance services | Clopidogrel use |
|---|---|
| New South Wales Ambulance | Yes |
| Queensland Ambulance Service | Yes |
| ACT Ambulance | No |
| Ambulance Tasmania | No |
| Ambulance Victoria | No |
| St John Northern Territory | Yes |
| St John Ambulance New Zealand | Yes |
| Wellington Free Ambulance | Yes |
| JRCALC (UK) | Yes |
| Alberta Health Services | Yes |
| British Columbia Health Services | No |
| Ireland | Yes |
Source: Ambulance Tasmania, 2012; St John Ambulance Northern Territory, 2013; Pre-Hospital Emergency Care Council (Ireland), 2014; Australian Capital Territory Ambulance, 2015; Association of Ambulance Chief Executives (UK), 2019; New South Wales Ambulance, 2020; St John Ambulance New Zealand, 2019; Wellington Free Ambulance, 2019; Ambulance Victoria, 2020; Queensland Ambulance Service, 2020; Alberta Health Service Emergency Medical Services, 2021; British Columbia Health Services, 2021
Reflective activity: scenario 1
As a double-crewed ambulance, you attend an 80-year-old female who is reporting central crushing chest pain that came on at rest only 25 minutes ago. You conduct your observations, finding that she is tachycardic, tachypnoeic, clammy and is having an anterolateral STEMI on the 12 lead ECG.
As part of her daily medication, she takes simvastatin, amlodipine, Aspirin, vitamins and a non-steroidal anti-inflammatory drug (NSAID). She discloses that her medical history consists of hypertension, atherosclerosis, hypercholesteremia, chronic liver disease and a stroke, but is unable to recall what type.
As part of your guidelines, you administer the STEMI care bundle and begin to consider what drugs to administer in preparation for the patient to undergo a PPCI at the local catheterisation lab which is 40 minutes away. Following your clinical practice guidelines, you prepare to administer clopidogrel but have some concerns in relation to the patient's past medical history and medication list.
Using the present article and your own research, discuss why liver failure and NSAID use can be a problem for clopidogrel administration.
Results
This review identified five factors most relevant to the safety and efficacy of prehospital clopidogrel administration for STEMI: therapeutic rationale, drug interactions, time of administration, absorption issues, and alternative P2Y12 therapies (ticagrelor and prasugrel). These will now be discussed sequentially.
Although bleeding tendency increases with clopidogrel use, particularly in conjunction with aspirin or fibrinolytics (Oldgren, 2010: 1454-1456), there appears to be no significant increase in bleeding risk when clopidogrel doses are elevated (Ducci et al, 2013) or when it is used 2–8 days before a PCI (Zeymer et al, 2007). Notwithstanding, patients who are concurrently receiving drugs which interfere with the clotting process must be monitored closely when clopidogrel is administered (MIMSOnline, 2021).
The efficacy of clopidogrel may be altered by other drugs which disrupt the way in which clopidogrel is metabolised. Clopidogrel is a prodrug, which means that after administration (in tablet form) the drug must undergo first pass metabolism to convert to its active metabolite form, clop-AM. Enzymes from the cytochrome P450 family are responsible for clopidogrel metabolism in the liver, including cytochrome P450 2C19 (CYP2C19) and cytochrome P450 3A4 (CYP3A4). Drugs such as some anti-fungals, proton pump inhibitors (used for gastric reflux) and steroidal agents may interfere with CYP2C19 and CYP3A4 enzymes—either by inducing or inhibiting these enzymes—which can compromise the therapeutic effects of clopidogrel (National Drug Agency, 2009: 19; Hasan et al, 2012; MIMSOnline, 2021).
With regards to 12-month mortality rates and bleeding risk, clopidogrel has been deemed safe (Mehran et al, 2011; Khan et al, 2016). Secondary admissions after a cardiac event where the drug was used in the prehospital setting were found to be common, potentially because of the delayed onset of biochemical effects (Ducci et al, 2013). On the other hand, when clopidogrel was given in hospital rather than administered by paramedics, mortality rates were higher after 1 year (Oldgren et al, 2010). The P2Y12 trials also demonstrated that clopidogrel was associated with a relative reduction in death, recurrent MI or stroke (OR 0.80; 95% CI [0.72–0.90]; P<0.001), and a relative increase in extensive bleeding (OR 1.38; 95% CI [1.13–1.67]) (Chew et al, 2016). Long-term use of clopidogrel was associated with a reduction in mortality, secondary MI occurrences and CVAs (Zeymer et al, 2007).
The timing of clopidogrel administration received attention within the literature. The paramedic ‘Clopidogrel to Improve Primary Percutaneous Coronary Intervention in Acute Myocardial Infarction (CIPAMI)’ study found that clopidogrel did not increase the patency of the vessel when the period between administration and PPCI was less than 1 hour (Ducci et al, 2013: 4814). However, bleeding tendency did increase (Oldgren et al, 2010: 1454–1456). Both of these factors may become an issue, particularly in urban areas where transport time is reduced; however, a 600 mg dose administered as soon as possible was found to have greater effects over longer time periods (Biscaglia et al, 2013: 192; Ducci et al, 2013: 4814). Several studies conclude that, because of this, clopidogrel needs to be administered early so as to reach the therapeutic range at the appropriate intervals for effective treatment (Zeymer et al, 2007; Biscaglia et al, 2013; Vercillino et al, 2017).
| Author | Article title | Result | Implication |
|---|---|---|---|
| Biscaglia et al, 2013 | Effects of pre-hospital clopidogrel administration on early and late residual platelet reactivity in ST-segment elevation myocardial infarction patients undergoing primary intervention |
|
Clopidogrel needs to be administered as soon as possible when on scene for maximum effect because of its long half-life |
| Ducci et al, 2013 | Comparison of pre-hospital 600 mg or 900 mg vs peri-interventional 300 mg clopidogrel in patients with ST-elevation myocardial infarction undergoing primary coronary angioplasty. The Load&Go randomized trial |
|
Clopidogrel needs a longer time to take effect, regardless of dose. This would be an issue in urban areas where transport time is shorter |
| Dhillon, 2015 | Ticagrelor: a review of its use in adults with acute coronary syndromes |
|
Clopidogrel relies on the hepatic P450 enzymes for metabolism, leading to delayed onset of action, genetic polymorphism and higher variations in individual responses. The irreversible binding to receptors causes rapid offset and drug interactions |
| Vercellino et al, 2017 | Ticagrelor versus clopidogrel in real-world patients with ST elevation myocardial infarction: 1 year results by propensity score analysis |
|
|
| Zeymer et al, 2007 | Efficacy and safety of clopidogrel 600 mg administered pre-hospitally to improve primary percutaneous coronary intervention in patients with acute myocardial infarction (CIPAMI): study rationale and design |
|
|
| Khan et al, 2016) | Pre-hospital thrombolysis in ST-segment elevation myocardial infarction: a regional Australian experience | Clopidogrel was found to be safe to administer in the prehospital environment | Clopidogrel has fewer adverse effects and a higher safety range when given prehospitally |
| Zeymer et al, 2015 | Influence of morphine on the effect of clopidogrel and prasugrel in patients with ST elevation myocardial infarction. Results of the ETAMI trial | Morphine adversely affects the antiplatelet inhibitory effects of clopidogrel | Morphine is often used in the treatment of ACS in ambulance protocols to treat associated pain |
| Bouman et al, 2010 | Predictive value of various platelet function tests on ST-segment resolution and clinical outcome in STEMI patients randomized to either dual or triple antiplatelet therapy: the OnTIME 2 platelet function substudy | The use of three different antiplatelets was more efficient than clopidogrel and aspirin alone | A combined antiplatelet treatment regimen has a more potent effect and is more beneficial in successful thrombolysis |
| Berwanger et al, 2018) | Ticagrelor vs clopidogrel after fibrinolytic therapy in patients with ST-elevation myocardial infarction: a randomized clinical trial |
|
Ticagrelor has a more predictable and consistent antiplatelet effect. Mortality rates are slightly lower with ticagrelor than clopidogrel but ticagrelor is associated with more adverse bleeding complications |
| Alfredsson et al, 2020 | Bleeding complications with clopidogrel or ticagrelor in ST-elevation myocardial infarction patients–a real life cohort study of two treatment strategies |
|
Use in patients aged >75 years was unknown |
| Charpentier et al, 2020 | Bleeding risk of ticagrelor compared to clopidogrel in intensive care unit patients with acute coronary syndrome: a propensity-score matching analysis | Co-administration of ticagrelor/aspirin was associated with a greater bleeding risk than clopidogrel/aspirin | Combined antiplatelet therapy is effective when the appropriate medications are used. Ticagrelor/ASA has more complications than clopidogrel/ASA |
| Harding et al, 2017 | Contemporary antiplatelet therapy in acute coronary syndromes: are there differences in outcomes and discontinuation between clopidogrel and ticagrelor? |
|
Ticagrelor lacks consistent evidence as a take-home drug in comparison to clopidogrel, and is also associated with increased bleeding events |
| Hee et al, 2019 | Real-world use of ticagrelor versus clopidogrel in percutaneous coronary intervention-treated ST-elevation myocardial infarction patients: a single-center registry study |
|
Clopidogrel has less effect on patients with a lower bleeding risk, but has a greater effect with other patients |
| Tang et al, 2016 | Assessment of ticagrelor versus clopidogrel treatment in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention | Ticagrelor significantly reduced the incidence of major adverse cardiovascular and cerebrovascular events and composite endpoints of non-fatal MI, stroke and cardiovascular death | There is no significant difference between ticagrelor or clopidogrel in relation to all-cause mortality, unplanned revascularisation, stent thrombosis, stroke, non-fatal MI or bleeding events |
The ‘Early Thienopyridine Treatment to Improve Primary PCI in Patients with Acute Myocardial Infarction’ (ETAMI) trial and ‘Administration of Ticagrelor in the Cath-Laboratory or in the Ambulance for New ST-Segment–Elevation Myocardial Infarction to Open the Coronary Artery’ (ATLANTIC) study revealed that the use of morphine also affects the bioavailability of clopidogrel, resulting in an even longer time to onset (Dhillon, 2015: 64; Zeymer et al, 2015; Vercellino et al, 2017: 8).
Both Farag et al's (2018) and Frampton et al's (2020) review articles corroborate the information found in the ETAMI trial and ATLANTIC study. These papers explain that the co-administration of morphine and oral P2Y12 platelet antagonists (i.e. clopidogrel) impairs the absorption rate and diminishes the onset and duration of the drug, subsequently weakening antiplatelet efficacy. This is because opioids have an inhibitory effect on gastric motility, which affects the absorption ability of the gastrointestinal system and decreases peak plasma levels of active metabolites within oral medications (Zeymer et al, 2015; Giannopoulos et al, 2016).
According to Hobl et al (2014), morphine diminishes the effects of a 600 mg dose of clopidogrel to a 300 mg dose, thereby increasing mortality. Similar concerns about concomitant opioid and P2Y12 use are reported by Ibrahim et al (2018) and McEvoy et al (2018). Further research is still required in this area.
Clopidogrel administered in conjunction with other therapy has been proved to be more effective than when given alone (Bouman et al, 2010; Alfredsson et al, 2020). The Clopidogrel as Adjunctive Reperfusion Therapy—Thrombolysis in Myocardial Infarction (CLARITY-TIMI) 28 substudy demonstrated that management of STEMI with clopidogrel, fibrinolysis and heparin leads to reduced ischaemic times and increased reperfusion (Zeymer, 2007: 267). The Clopidogrel as Adjunctive Reperfusion Therapy (CLARITY) study further emphasised that fibrinolysis was improved when clopidogrel was used (Zeymer, 2007: 266). The ExTRACT-TIMI-25 study demonstrated that combining clopidogrel with enoxaparin was also beneficial (Arntz, 2008: 301).
Ticagrelor and prasugrel are two other commonly used platelet antagonists. Ticagrelor is an adenosine diphosphate (ADP) antagonist that reversibly binds to P2Y12 receptors at an allosteric site (Hermanides et al, 2018). It is commonly used in broad-spectrum ACS patients presenting in an intermediate to high-risk category of STEMI or non-ST ACS (NSTEACS) (Chew et al, 2016).
Ticagrelor is known for its faster onset, its lower risk of additional ischaemic events, MI, CVA and mortality (OR 0.84; 95% CI [0.77–0.92]), and is more efficacious when used in conjunction with aspirin than with clopidogrel (Dhillon, 2015; Chew et al, 2016; Tang et al, 2016; Vercillino et al, 2017; Berwanger et al, 2018).
Compared with clopidogrel, Dhillon (2015) and Vercellino et al (2017) stated that ticagrelor was associated with lower bleeding risk, while Hee et al (2019) noted it was more efficient in patients with a pre-existing bleeding risk. However, Chew et al (2016) and Harding et al (2017) found the opposite to be the case (OR 1.25; 95% CI [1.03-1.53]).
Berwanger et al (2018) and Alfredsson et al (2020) discovered that minor bleeding and complications, in addition to higher thrombolysis in myocardial infarction (TIMI) scores, were more common with the administration of ticagrelor. However, fatal bleeding rates were comparable between the two (Berwanger et al, 2018; Alfredsson et al; 2020). In terms of bleeding risk related to co-administration, Charpentier et al (2020) found that bleeding risk was significantly higher as a result of the use of ticagrelor and aspirin compared with the use of clopidogrel and aspirin. Ticagrelor was also associated with higher discontinuation rates because of adverse events related to increased bleeding, dyspnoea, ventricular pauses/bradyarrhythmia, and inappropriate consumption/chronic overuse (Harding et al, 2017).
Prasugrel is another P2Y12 antagonist that is metabolised into its active form by cytochrome P450 enzymes in the liver (Chew et al, 2016). Prasugrel was found in the Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel—Thrombolysis in Myocardial Infarction to be more effective in decreasing the risk of additional ischaemic events, MI, CVA and mortality (9.9% versus 12.1%; P< 0.001) (Wiviott et al, 2007). Chew et al (2016) concurred with these findings (OR 0.81; 95% CI [73–0.91); however, they noted that prasugrel was associated with an increased risk of bleeding (OR 1.32; 95% CI [1.03–1.68]), particularly in patients receiving coronary artery bypass grafts (Chew et al, 2016). In patients aged over 75, with previous cerebrovascular disease, below the weight of 60kg and with a medical history of transient ischaemic attacks or strokes, prasugrel has been found to be harmful.
Prasugrel was associated with higher platelet inhibition than clopidogrel (Hermanides et al, 2018). It is particularly efficient when no previous P2Y12 antagonists have been administered, and when PCI is indicated (Chew et al, 2016).
Discussion
As various trials show, clopidogrel significantly reduces mortality without significantly increasing bleeding intensity. The use of clopidogrel in the prehospital environment, although reasonably safe, effective and easily administered, appears to be optimal when there are extended transport times to hospital (Ducci et al, 2013: 4814–4816).
Clopidogrel is more commonly used in conjunction with fibrinolysis and when ticagrelor and prasugrel are contraindicated (Nickson, 2019).
Although the therapeutic effects of clopidogrel are unlikely to be fully realised in the prehospital environment, this review notes that early administration of clopidogrel is beneficial in the treatment of STEMI. This is particularly the case where there are extended transport times to a primary PCI facility. Risks relating to bleeding tendency, and the potential effects of other common drugs on clopidogrel metabolism were noted. A further area of research may be to consider the topic of opioids and clopidogrel absorption, examining how this may relate to the care delivered in prehospital settings.
Reflective activity: scenario 2
You are a senior clinician that has been working with various teams within the JRCALC to audit and develop current clinical practice guidelines based on evidence-based practice. One day, you receive a query from an ambulance service in Canada about whether intravenous morphine should be administered as an analgesia to STEMI patients who are also receiving clopidogrel. Studies have shown evidence of morphine slowing a patient's gastric motility and therefore gastrointestinal absorption of clopidogrel.
Currently, where indicated, patients can receive both morphine and clopidogrel within the STEMI care guideline. Using the current article and your own research, provide your recommendation for or against the use of morphine in STEMI patients indicated for clopidogrel.
Conclusion
The purpose of this study was to examine peer-reviewed articles and clinical practice guidelines relating to prehospital clopidogrel administration, and explore whether this drug should be more widely used across international ambulance services.
Although the therapeutic effects of clopidogrel are unlikely to be fully realised in the prehospital environment, this review notes that early administration of clopidogrel is beneficial in the treatment of STEMI. This is particularly the case where there are extended transport times to a primary PCI facility. Risks relating to bleeding tendency, and the potential effects of other common drugs on clopidogrel metabolism were noted. A further area of research may be to consider the topic of opioids and clopidogrel absorption, examining how this may relate to the care delivered in prehospital settings.

