It is estimated that one in five pregnancies end in miscarriage. Sadly, this number is likely to be higher as a large proportion of pregnancy losses are managed at home and go unreported (Tommy's, 2022). With such prevalence, I would expect this to be something that most readers have dealt with, regardless of clinical setting. It is also likely that you will know someone personally who has been through this experience—however, if you think you don't, is this truly the case or is it a reflection of the stories that have never been shared?
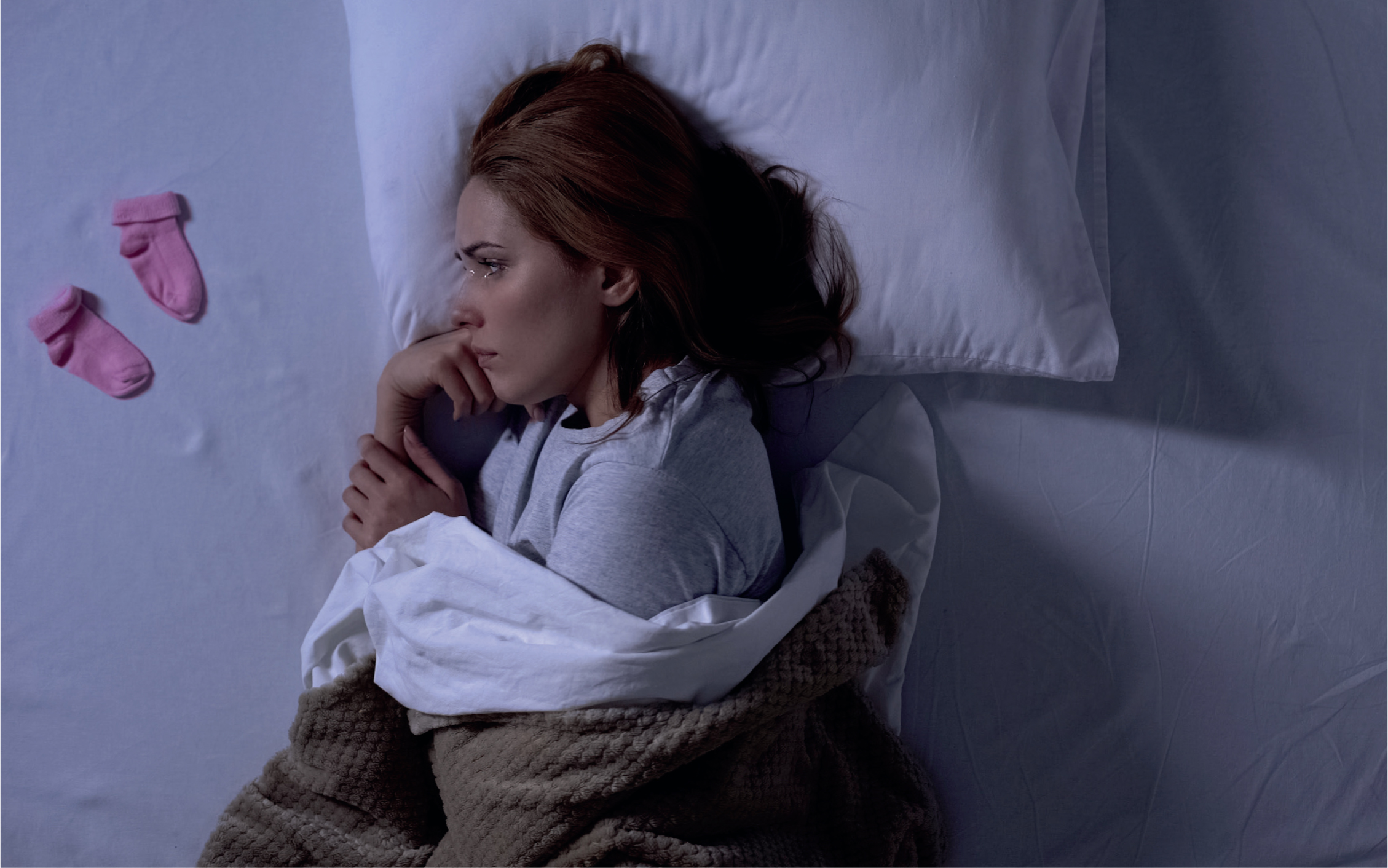
My name is Nikki and I am an Advanced Paramedic Practitioner in Urgent Care. I am the one in five women who has lost their baby. I want to break the taboo that surrounds talking about early pregnancy loss and share my story—as both a clinician who wants to educate for the benefit of patients, and as a mother who was never able to bring her baby home.
Following 3 years of infertility and one round of in vitro fertilisation (IVF), I was devastated to hear that a pregnancy I had so longed for was ‘not viable’ when no heartbeat was detected at our first scan. Although my loss was early, it was no less devastating. Without going through this experience, I could not have imagined how deeply affected by it I would be. I lost more than my baby; in that moment, I lost the future I had planned out, I lost my confidence, my identity, and my faith in those around me.
Taboo around early miscarriage
An early miscarriage is defined as a pregnancy loss in the first 12 weeks (Saying Goodbye, 2023) and this accounts for approximately 80% of miscarriages (NCT, 2023). It is because of this statistic that most pregnancy announcements are made after this time and there is a societal norm that early pregnancy is not spoken of. This creates an absence of conversation and a lack support when it is needed most—not only for women who may start to experience symptoms of pregnancy, and be required to alter their clinical roles if they work within our profession, but also for those whose pregnancy will sadly come to an end.
Sharing our loss
It is a very difficult conversation to announce the loss of a baby no one knew about. Many women feel they have to deal with their miscarriage in silence and carry on as normal while they privately grieve (Gurtin, 2020).
In my own workplace, I felt comfortable in talking about my journey through IVF and, as my management team and closest colleagues had an awareness of the treatment, I announced its success early on. I was ready to adapt my clinical duties as set out in policy and looked forward to the exciting journey I thought I had ahead. My openness meant that the people around me knew I was pregnant when I had to share that I no longer was, but it was this honesty that made me feel so foolish and naïve that I was under the illusion my pregnancy would result in a baby being born.
Types of pregnancy loss
There are different types of early pregnancy loss and non-viable pregnancy as shown in the Table 1.
| Threatened miscarriage | Vaginal bleeding or abdominal pain in a pregnancy that is deemed as viable on a scan |
| Incomplete miscarriage | Bleeding that has started but pregnancy tissue remains in the womb |
| Missed miscarriage | A pregnancy that has stopped developing but remains inside the womb, often with no symptoms to suggest the pregnancy has ended |
| Anembryonic pregnancy | Embryo development stops early and only an empty pregnancy sac is visible on the scan |
| Ectopic pregnancy | An embryo that implants and begins to grown outside of the uterus |
| Molar pregnancy | An egg that is incorrectly fertilised and placenta develops abnormally resulting in cyst formation |
| Chemical pregnancy | Loss before or around 5 weeks. Detected only by a pregnancy test as it is too early for anything to be visible on a scan. Often women will not have realised they were pregnant |
A miscarriage is also not an instant diagnosis, detecting the viability of a pregnancy can take weeks when ultrasound scans are carried out between 7 and 14 days apart to determine if a heartbeat can be detected of if an embryo has or has not grown (National Institute for Health and Care Excellence (NICE), 2019).
Managing miscarriage
Miscarriage management can be determined by choice or clinical need, and can take different forms (Table 2). As a clinician, I found becoming a patient during pregnancy loss very difficult. Particularly working in the ambulance service, paramedics may attend patients when they are at their worst during a miscarriage because the bleeding is too heavy or the pain is too much. Based on my experience in attending the patient group I now found myself in, I could not help but catastrophise my own situation and worry for events that thankfully did not occur. I was swept up by the kindness and compassion of the early pregnancy assessment unit (EPAU) and could not fault their treatment. For staff who experienced my presentation every day, they were sensitive, caring and took time to explain every procedure. I was saddened however that this experience was not reflected with my own general practitioner (GP).
| Expectant management | A women will wait for the miscarriage to commence naturally and on the resolution of pain and bleeding take a pregnancy test to ensure the pregnancy has ended |
| Medical management | Medication is taken to encourage the body to start the process of miscarriage |
| Surgical management | The embryo or baby and surrounding pregnancy tissue are removed under general anaesthetic |
Capacity to care
I had an extended amount of time off work. I could not imagine caring for others when I was hurting so much: the thought of being the person who someone else was turning to for help terrified me. How do I support someone else through their trauma when I cry every day after my own? When I went to my GP to obtain a sickness certificate, I was asked for proof of my loss ‘because I can't take your word for it!,’ said my GP. What I believe he meant was that he had not yet received my discharge papers and was unaware of my experience. However, he did not express his thoughts in this way or with any sensitivity. There was no exploration of how I was dealing with my grief or if my physical pain and symptoms had subsided. I felt ashamed and belittled. This experience shifted my core belief that if I needed help, there are trained professionals who care. I always treat my patients how I would want to be treated and, yet, when I was in need, I did not receive this care in return. In the months that followed, I continued to receive paperwork for the pregnancy I no longer had, and as my due date loomed, I received antenatal appointment notifications and a call from a midwife to arrange a visit. I felt guilty every time I had to explain I had miscarried 5 months previously, appreciating the busy work schedules of these professionals—however, I should not have felt this way.
Psychological impact of early pregnancy loss
The psychological impact of an early pregnancy loss is often something that is overlooked. A recent study has shown that 29% of women were experiencing symptoms of post-traumatic stress disorder (PTSD) 1 month after early pregnancy loss. In addition, 24% of women were experiencing anxiety and 11% had depression. At 9 months after loss, 18% (about 1 in 5) of the women continued to experience PTSD, 17% had anxiety, and 6% had depression (Farren et al, 2020). I was lucky enough to know how and where to access invaluable support through my ambulance trust; however, this is not often something afforded to the general public. In 2019, a survey of health commissioners across the UK demonstrated that in 86% of areas, there are no specialist therapies to support parents who have lost a pregnancy or whose baby has died (Babyloss-awareness, 2019). Before experiencing this myself, I would not have known where to direct patients or been aware of any available resources through which they could seek help.
Being the statistic
I write this article because one in five pregnancies end in miscarriage. I am a paramedic and I was that statistic. I know that my story is replicated among the patients you see and the colleagues you work alongside. If one person reads this and feels less alone, or reaches out to someone they know and feels able to share their story, then mine was worth sharing.
‘The privacy of baby loss should be a choice and not an instruction.’

