Medical simulation has been a key component in healthcare education for many years but it is seen by many as purely the use of mannequins in pressurized situations to test the competency and skills of practitioners in a safe yet ‘realistic’ environment. Nevertheless, the authors of this article question whether educators are using the technology to its fullest potential, as 2011 brings with it many new challenges (Fritz and Gray, 2008).
We believe that the use of simulation in prehospital education is concerned with not only how educators educate but more importantly, how learners learn. New models are being investigated—both active, for teaching purposes; and interactive, for practice purposes, allowing errors to be made with reactions to those simulated errors.
Many traditionally trained health personnel can relate to the days of formative and summative assessments when assessors put them through one-off pass/fail opportunities to demonstrate full competency, seen by some as the process of learning a robotic pattern and repeating it on demand in a simulated environment.
The authors suggest that the use of simulation in many healthcare settings is assessment focused, with the implication that the crucial process elements of learning may be lost. In prehospital and emergency care education, a heavy emphasis on skills acquisition and testing may serve only to perpetuate the problem. This article hopes to illustrate the potential benefits to the learning experience that simulation can bring when the focus is changed to process, rather than outcome.
Literature review
There is compelling evidence to demonstrate the educational and contextual benefits of simulation in healthcare settings (Okuda, 2008; McGaghie, 2010). This is especially evident in the training of surgeons in developing minimal access and endoscopic techniques (Flanagan et al, 2008; Larsen et al, 2009). Further evidence has been generated out of necessity, particularly within the nursing profession where opportunities for clinical placements have become drastically reduced (Henrichs and Rule, 2002; Bremner, 2006).
Indeed, a circular from the Nursing and Midwifery Council (NMC) in 2007 advised higher education institutions (HEIs) that alternative clinical placement hours could be acquired via simulated practice to a maximum of 300 hours (out of 2300) over the three-year period of pre-registration training to be a registered nurse. This could mean that students, who would normally learn the art and science of their profession on wards and departments, could now potentially learn in a simulated environment at the university.
In these contexts, simulation may be incorporated within other modes of learning which have been demonstrated to contribute positively towards ‘learning by doing’ and problem solving (Medley and Horne, 2005). However, if simulation is used in a reductionist assessment-driven way, valuable additional elements of a clinical learning experience may be lost, given the notion that simulation often involves something which must be passed before being allowed to progress to a situation in the real world.
This belief of passing or meeting the requirement of an assessment pervades many aspects of prehospital care; advanced life support (ALS) being a good example. Frequently, the use of other scenario-based simulation activities within educational programmes has some form of assessment as a focus, such as the objective structured clinical examination (or OSCE).
This assessment-driven focus may influence the learner's perception of simulation as a learning opportunity. This can subsequently generate anxiety for learners who feel that the experience will be one of fault finding as opposed to improving and developing capability and capacity. This philosophy seems to associate very closely with a ‘quality control’ model, which seeks to find fault, as opposed to a ‘quality assurance’ model whose emphasis is on continuous improvement and developments.
Simply put, although simulation is encouraged and supported by professional bodies such as the Health Professions Council (HPC), the authors have discovered that anecdotally there is little evidence of its use within curricula; aside from formative assessments or at the end of plenary sessions; to assess if theory can be put into practice whereas it could be used more fully, allowing standards for clinical competence to be safely met (Boker et al, 2008).
‘There is compelling evidence to demonstrate the educational and contextual benefits of simulation in healthcare settings’
Lessons from aviation
Simulation in its most prestigious and arguably most expensive sense is best illustrated in civil and military aviation specialities, which have used it for many years (Hamman, 2004). The fight simulators used by airlines offer highly representative environments (high-fidelity simulation) allowing for an exceptionally high levels of realism. This creates boundless educational and situational opportunities.
It is common knowledge that fight crew are required to spend a designated period of time in the simulator each year, in order that they may rehearse or practice an unusual or very unlikely situation on board the aircraft such as system failures and engine fires. Thankfully, these incidents are extremely rare; however, this is not the case in health care.
Medical emergencies such as myocardial infarction, stroke, collapse, respiratory difficulty and cardiac arrest are frequent if not common occurrences in prehospital and emergency care. There seems to be little need therefore, to rehearse how one may react to any one of these situations as the clinician is exposed to them so frequently. As in the aviation setting, there are procedures and protocols to be followed in the event of an unplanned situation. Emergency medicine and prehospital care have similar protocols and procedures to follow, and it is often these protocols and best practice guidelines that we rigorously test in a simulation activity or environment.
The obvious elements overlooked by taking this approach include decision-making, team work, and communication between staff, supportive collegial interventions and a dialogue with clinical colleagues. Interestingly, it is these elements from aviation which we seemed not to have learned so well. However, the notion of translating lessons from aviation into healthcare has come under recent criticism with the suggestion that when faced with a problem, the pilot does not have to diagnose the systems on board as the aircraft will display the problem and how it should be dealt with. This of course, combined with checklists and drills, does not translate into prehospital care (Rogers and Gaba, 2011).
Simulation or simulator?
Perhaps our emphasis should shift from simulation equipment (i.e. mannequins) to scenario-based learning which integrates with the use of simulation equipment. High-fidelity simulation equipment (i.e. which represent a high degree of realism) is only one of many tools available to develop clinical and teamworking skills (Beaubien and Baker, 2004). With this in mind we should look at ways of building our educational activities with learners around a more integrative approach which is augmented or complemented, not replaced, by simulation equipment.
Fidelity in simulation
A pivotal issue, worthy of discussion is the concept of fidelity in simulation. Fidelity is the term frequently used to describe the degree to which the simulator replicates the real thing. Traditionally, simulators have been labelled high-fidelity (like the fight simulators used by airlines) or low-fidelity (such as Resusci Anne).
However, simulation, in its broader sense, is much more complex. The effectiveness of simulation has a number of dimensions, which is best summarized by the work of Quinones and Rehman (1995) which despite its age, still holds some important meanings and value:
Figure 1 illustrates the interface between these levels of fidelity as applied to the education of emergency care personnel.
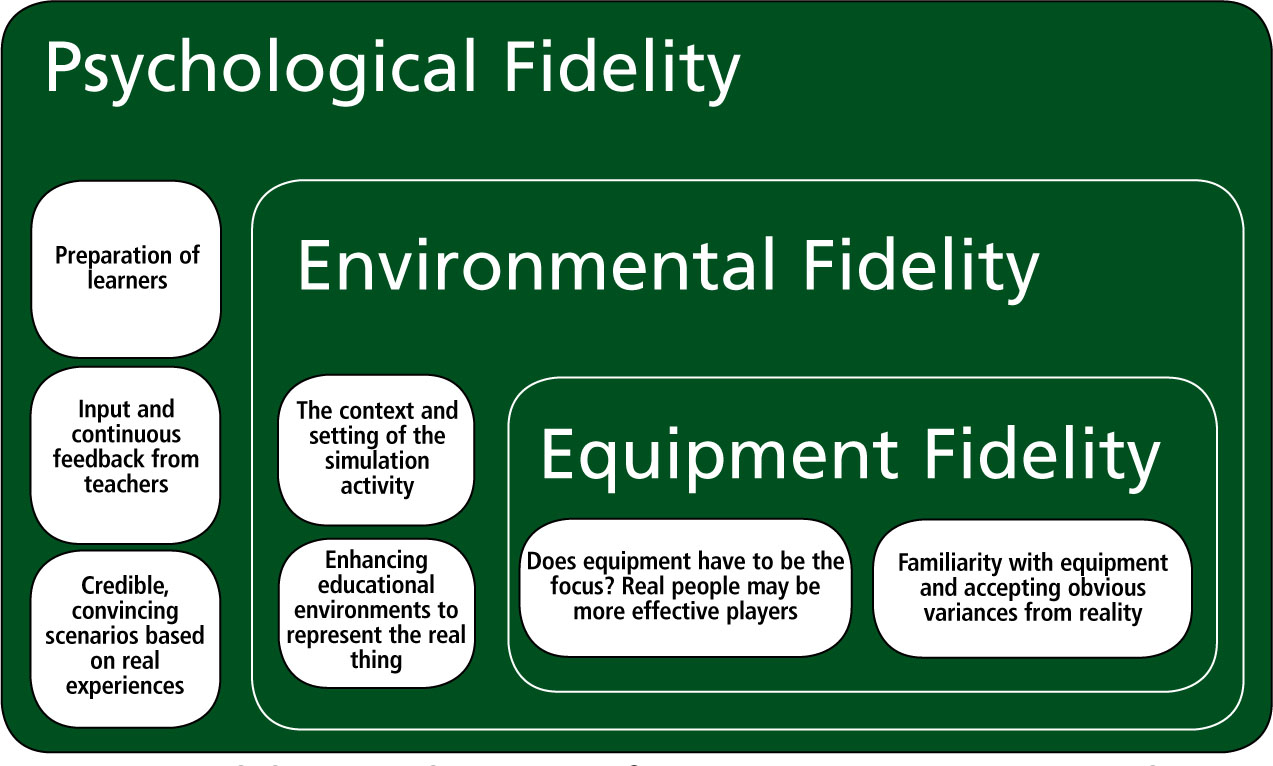
Equipment fidelity
Equipment fidelity may be compromised in prehospital care education by a lack of life-like mannequins and other simulation equipment such as vascular access arms, catheterization simulators and airway training heads. Many learners may feel that the equipment lacks realism because of the inability to replicate real qualities such as skin temperature, texture, and hydration state.
While there is an ethical argument for ‘practising clinical skills’ such as cannulation and catheterisation on patients, there are many skills such as history-taking and clinical examination which can be learned using fellow students or the employment of NHS service users to act as patients. A study by Jones (2006) demonstrated positive benefits of the use of ‘simulated or standardized patients’ for learners and service users in this respect.
It is also possible that equipment fidelity is compromised by the fact that learners need to become familiar with how it works, operates or feels. It is perhaps these elements which are least like the real thing, and a frequent source of loss of realism.
Environmental fidelity
The compromise of environmental fidelity is one of the biggest challenges faced by health educators. The simulated environment is extremely important in assisting in the process of learning as it should represent the real working environments of the learner. For example, even a very expensive high-fidelity simulation mannequin bristling with the latest technology will not create the level of realism required, if it is placed on a floor in a university classroom when the scenario is meant to take place in a hospital context.
The environment clearly requires adjustment to augment any potential benefits from the equipment. Re-creating rooms which look like trauma receiving rooms, resuscitation bays in an A&E department, and the inside of an ambulance is all but reserved for prestigious ‘simulation centres’, forcing many university departments to create and develop more ‘universal clinical areas’ in their teaching facilities, which can be used for a variety of disciplines.
Psychological fidelity
Psychological fidelity is one area where educators can have an important impact on the quality of the educational experience for learners. Scenarios based on real situations are likely to be accepted by novice clinicians who lack the experience of their educators. It is important to make the learner feel that the simulated experience is laudable and appropriate to their level of experience, complemented further by how the student is prepared for the event.
Typically in the assessment of clinical skills and competence in prehospital or resuscitation training, students are asked to wait outside a room and are then called in and given a brief in the simulated area—this of course would not happen in reality.
The evolution of high fidelity simulation in education: considerations for practice
As we continue to embrace multi-definition methods of simulation, the authors suggest that there is a need to review how the curriculum in HEIs is formulated. Individuals given the responsibility of timetabling and scheduling throughout the duration of a pre-registration programme in prehospital care should be mindful of how best to allow full student development with the options available.
As previously suggested, the authors feel that in order to benefit fully, the environment in which learning takes place and the equipment that they use for that learning needs to replicate, as close to practice as possible, those which are in used in real clinical practice. This places many university faculties and departments under considerable spatial and financial pressure.
We recognize that this produces a dilemma given the economically challenging situations HEIs face today. Costly investment into what would be considered ‘high-fidelity simulation’ requires obvious evidence of value for money by maximization of learning opportunities for students. However, we would argue that simulation plays an important part in enabling HEIs to deliver healthcare practitioners who are equipped with decision-making abilities and psychomotor skills ft for purpose in prehospital care. The cost benefits of this can then be fully appreciated.
Importantly, one barrier to the opportunities for learning may be the entrenched interpretation of simulation as being predominately a resource intensive way of acquiring psychomotor skills. The authors suggest a shift from this traditional model towards a model fostering learning development opportunities for students via a multitude of simulated activities including:
The introduction of role play offers students learning opportunities within an emergent scenario or clinical dynamic situation. This approach has the potential to extend decision-making capabilities over a period of time which develops with each re-enactment. Thus the skilful combination of strategies which incorporate some or all of the above potentially enabling the facilitator to provide an experiential learning environment which is clearly safe for the student where rehearsal for both psychomotor skill acquisition and decision-making strategies can be maximized without compromising client care.
Refection on, and during, practice enables the learner to re-evaluate their ability, knowledge and responses as part of a novice to expert continuum (Benner, 1984; Larew, 2006). The expenditure of time in planning and delivery comes from HEI's attempts to create a convincing illusion that the simulated situations are real; in our experience the key elements of this incorporate those outlined in Box 1.
As far back as 1968, Tansey and Unwin noted that once created, the same simulation activities can be repeated for future cohorts with minimal modifications as new evidence becomes available. This model recognizes that there may be an initial heavy investment of time and planning, but then this workload reduces for future cohorts or intakes of students. Additionally a key feature of this approach is how it seems to change the role of the educational facilitator.
According to Morgan and Cleave-Hogg (2000), the use of simulation puts the educator into a new role, a role that is the inevitable result of evolution. Most teaching staff recognize that their role is no longer that of a presenter of information and that students are no longer passive recipients of new knowledge.
There is a realization, supported by evidence, that by transposing these simulated educational experiences into practice improves levels of patient safety (Grady et al, 2006; Murray et al, 2008). Moreover, Schoening (2006) identified that learners exposed to simulation felt that their learning needs were met and, in turn, this improved their confidence and competence to practice. This therefore has the potential to increase motivation and retention of students on healthcare programmes, thereby impacting positively on controlling rates of attrition.
Conclusion
The argument in this article is that debate around simulation principally focuses on ‘high equipment fidelity’. However, for many HEIs, operating in times of austerity, this is a luxury they can ill afford. By moving away from the purely assessment focused simulation experience, to a combination of strategies which include scenario and role play and continuous feedback techniques, a simulation environment may be created enabling learning opportunities which focus on process not product.
