From its Glasgow base, the Emergency Medical Retrieval Service (EMRS) provides secondary and primary critical care retrieval across Scotland. Over the past 24 months they have employed a team of five critical care practitioners (CCP), consisting of both paramedics and nurses. The multidisciplinary CCP team has been a great success, and as the team's experience grows, the role has progressed to advanced practitioner level, as per the Royal College of Nursing's (RCN) and College of Paramedics’ (COP) respective frameworks. This article will demonstrate this unique teams journey to advanced practice.
Background
EMRS has two teams available 24 hours a day. Each team comprises of two, the first person being a consultant with a specialty in emergency medicine, anaesthetics or intensive care, and the second person being either a senior registrar from the same specialities or one of the CCP team.
‘Retrieval can be described as the deployment of a critical care team to a seriously ill or injured patients’ location to undertake resuscitation and stabilisation prior to safe transfer to definitive care (Hearns, 2012).’
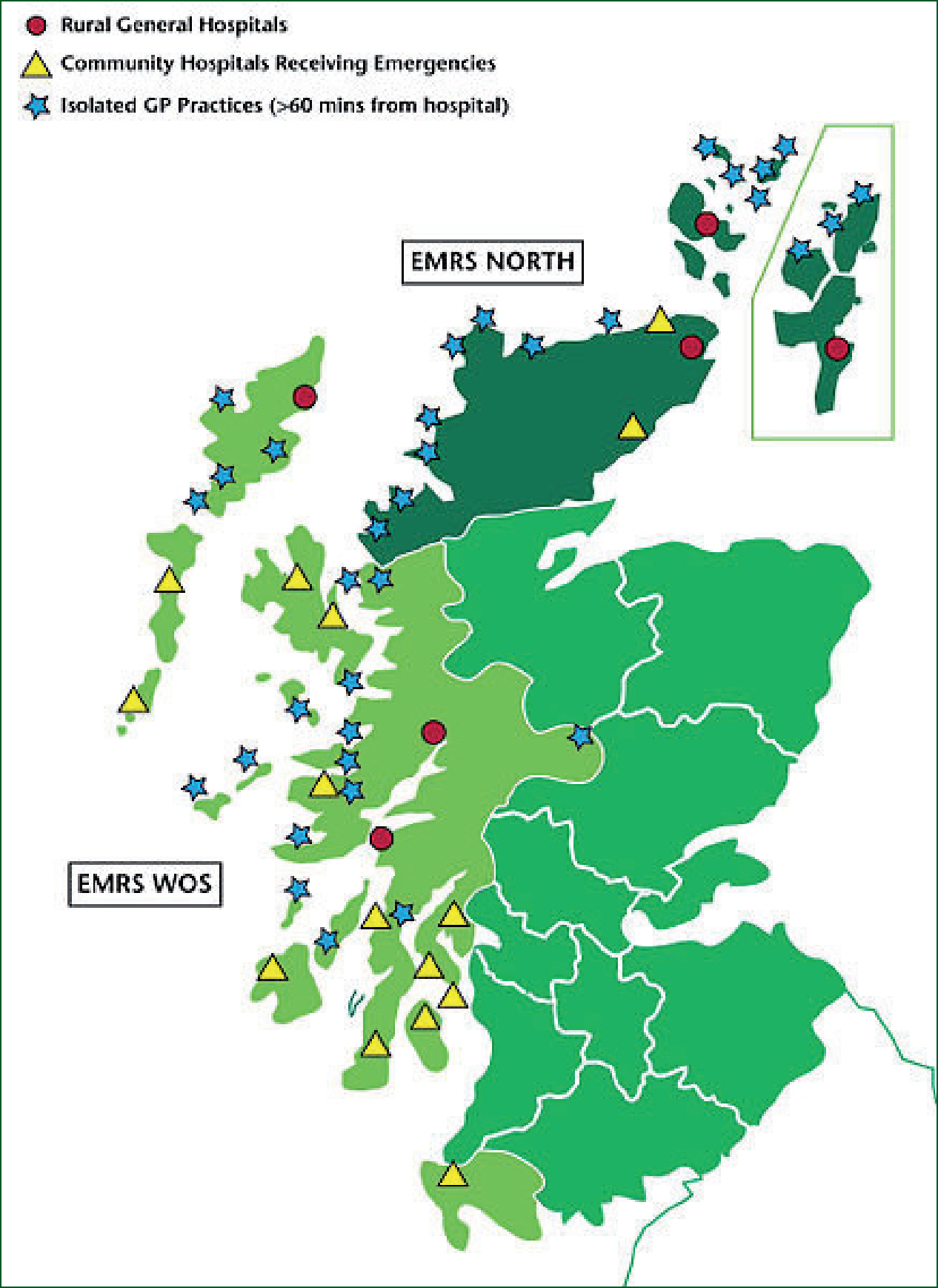
Secondary retrievals are necessary due to the unique geography of Scotland, as there are many remote healthcare sites situated on the west and north coast. These retrievals take place from a variety of healthcare facilities including district nurse practices, remote GP surgeries, community hospitals and rural general hospitals. The patients who arrive at these facilities are often critically ill and with limited equipment and specialist staff available at these facilities, patients can easily exceed the local critical care capability. The service ensures these patients have equal access to the appropriate level of care (Sturgeon, 2008) by bringing the emergency department resuscitation room or intensive care department skills to the patient, regardless of location.
In the pre-hospital environment, the service responds as the EMRS trauma team. This has provided a dedicated pre-hospital critical care team for the west coast of Scotland and the densely populated area of greater Glasgow, thus ensuring critical care support to the ambulance clinicians of the west of Scotland (Findlay et al, 2007). Within the Glasgow area, the service responds in one of their dedicated response vehicles, whilst further distances are reached by helicopter in a Helicopter Emergency Medical Service (HEMS) configuration with the Scottish Ambulance Service rotary aircraft Helimed5.
Due to the range of locations and geography, the service utilise various transport platforms to reach secondary locations. Transport is predominantly by air in association with the Scottish Ambulance Service rotary and fixed wing aircraft, although at times due to weather the service utilises the search and rescue rotary aircraft. Even with these multiple aviation options, there have been instances of severe weather or high demand where it has not been possible to get to the patient, which has seen the team utilising transport platforms such as ferries and lifeboats.
Critical care practitioner
In October 2011, the service launched a critical care practitioner project, which would see the CCP being the second team person, which historically had been filled by senior registrars, in a consultan-led clinical team. Along with the clinical involvement and responsibility, the CCPs have essential non-clinical roles that each of them lead for service provision and development.
A team of five were recruited from a multidisciplinary team of nurses and paramedics. At the time of recruitment, there was no specific retrieval medicine qualification that could be used as part of the selection process. The team brought a range of specialist practitioner degrees, post graduate diplomas and specialist qualifications in critical care. The team has a combined experience of over 50 years of pre-hospital, emergency department and critical care experience.
The team is a true multidisciplinary team, with both professions working together in the same role with the same job title. Every team member has a different clinical background and experiences, allowing the team to work and train together, closely pulling on each others’ experience and skills to become the most effective that we can.
More than the bag carrier?
What has been the outcome of this project at this point? Have the CCP team been there only to carry the bags and mop the doctors brow during retrievals?
In reality, it could not have been further from this. Due to the two person team configuration and at times, limited clinical resources at primary and secondary scenes, this is a fully involving role and there is literally nowhere to hide and full clinical involvement is absolutely necessary.
Secondary retrieval environments vary between many locations, in comparison to an urban tertiary hospital where these patients would be resuscitated by a large multidiscipline team. We aim to deliver the same level of care with a much smaller team in varying facilities. At times this might only be the two person retrieval team due to other demands on local clinical staff. This demonstrates the 100% hands-on learning which has been experienced by the CCP team.
The team has experienced a large exposure to critical care, completing over 600 retrievals and being involved in over 140 emergency anaesthetics.
The team configuration working one-on-one with a consultant, clinical situations and environments faced, has allowed the CCP team to undertake an apprenticeship in critical care retrieval medicine.
As a paramedic with a keen interest in critical care, I would compare the learning experience to a keen tennis player going out and playing every day with Andy Murray or Rafael Nadal. If you are keen, interested and have an open mind, you cannot help but learn at every stage of the working day. This learning has been unique and has been the richest experience of the CCP team's career, and we feel it would be difficult to replicate this learning from more traditional educational sources.
The configuration of the team allows the CCP team to undertake interventions and procedures under the consultants’ direct supervision, which would normally be out-with our scope of practice. This has provided a unique opportunity to gain experience in these advanced interventions in the safety of a supervised practice environment. The team regularly practice full critical care resuscitation, including emergency anaesthesia, ventilation, invasive monitoring, advanced chest intervention and vaso-active drugs, and much more.
The learning has continued in a non-clinical role. As we are aware that there is unpredictability in retrieval workload we have a twice daily teaching programme at the base consisting of:
Skills and knowledge are further maintained via the EMRS CCP currency programme, a peer-reviewed assessment of skills, knowledge and equipment which rotates over a 12 week period, keeping the team as effective as possible.
Non-clinical duties have proven to be surprisingly educational as well, as the team maintain the service electronic database, manually entering all handwritten mission run sheets and doing 24 hour patient follow ups. The team also review the hospital case notes of every patient retrieved at the receiving hospital to complete ICU and trauma scoring, a quick way to gain exposure and knowledge of physiological results and anatomy.
Progressing to advanced practice
As the team and the service progress, we are keen to mature the role to become as effective and knowledgeable practitioners as possible. With this, the CCP role is developing, moving to an advanced critical care practitioner level. The programme of development is going to consist of three elements: a postgraduate education programme, On-going and increased clinical exposure, and continual clinical mentorship. The team believe it is absolutely necessary to have a balance of all three to progress safely and effectively.
Education is going to be achieved in conjunction with a local university; the service has developed a bespoke Post Graduate Certificate (PGCert) course in Advanced Clinical Practice (Retrieval Medicine), to quantify and formalise the vocational education and practical skills which have taken place over the past 24 months. The course will streamline our underpinning knowledge of critical care at an advanced practice level.
Clinical exposure is going to be achieved by continual full-time involvement in primary and secondary retrieval medicine. This will be supplemented with further clinical placements in various clinical settings in local emergency, intensive care and anaesthetic departments.
Finally, clinical mentorship from working in the consultant-led retrieval service is one of the most important parts to the CCP team in this project. Having the ability to capitalise learning from a group of self-selecting retrieval experts has given the added advantage to succeed in the aim of advancing practice.


Understanding the bigger picture of retrieval medicine
This system of education will allow us to continue to grow and understand the bigger picture of retrieval medicine in Scotland in which we will practice. Progressing from the thought process of clinical assessment, diagnosis and treatment, to begin to consider other important confounding factors, which at times can be more challenging than the clinical picture alone.
Scottish weather and its geography can cause many problems and add many layers to the decision-making process before you have even seen the patient. Logistical decisions can play as big a part as the clinical decisions and so many factors need to be taken into consideration. We need to mature and grow as practitioners to a level which will allow us to function efficiently and safely, considering many logistical factors whilst delivering effective critical care in any environment.
Autonomous practice and the future
Autonomous practice and skills is a common theme for questions and interest around this project. We differ from some critical care nursing and paramedic pathways in the UK as at present we do not practice autonomously. We will continue to work as part of a medical team during our advanced training as this will be an essential part of our development and education. Our team configuration removes any need for having certain desire for autonomous skills, drug or intervention immediately, as we can practise the majority under direct supervision.
Autonomous interventions and skills will follow naturally into our skills set when we become experienced, knowledgeable and competent with them. As we progress into advanced practice we aim to deliver the same level of practitioner skill and knowledge which would be expected in the large hospital setting.
As we progress to become more experienced and knowledgeable, there will be opportunity for autonomous practice with CCP-led and CCP-only retrievals.
Although, as a team we have a healthy respect for the isolation which we face in our practice and how complex and challenging situations can be. In these situations you are the last line of clinical help. The team of clinicians that responds needs to be competent and be able to deal with whatever situation is faced.
The team need to progress to a level where we have a skill set to match any patient, rather than looking for a patient to match our skill set. It has become apparent to us over the last 24 months that it is at times more important what you can see in an overall clinical picture, rather than what you can do to correct a specific presentation or problem.
The EMRS CCP/ACCP pathway continues to provide an alternative and unique critical care retrieval medicine experience and education pathway in the UK.

