Of the approximately 60 000 out-of-hospital cardiac arrests (OHCA) in England per annum, roughly 30 000 receive resuscitation care by the emergency services (Hawkes et al, 2017), around 7500 attain return of spontaneous circulation (ROSC), and less than 5000 survive to discharge (Perkins et al, 2016).
Ventilation of the patient is a key factor in determining outcomes in cardiac arrest (Van Schuppen et al, 2021), respiratory depression (Rowe et al, 2022), and certain acute strokes (Popat et al, 2018). Ventilation with an accurate tidal volume (TV) is independently associated with favourable neurological outcomes and correlates with earlier weaning from mechanical ventilation (Beitler et al, 2017). Hyperventilation is also associated with impaired venous return, further limiting the efficacy of resuscitation efforts (O'Neill and Deakin, 2007). Therefore, it is imperative that patients receive lung-protective tidal volumes (LPTV) in the prehospital setting.
This systematic review aims to identify and assess tools currently used to calculate TV, typically by estimating or measuring weight and/or height in adult patients. The absence of validated tools in use within UK ambulance services underscores the need to identify an instrument adaptable to prehospital settings. Assessing the adaptability of each tool to diverse population groups is a further objective.
Background and rationale
TV refers to the volume of air entering the lungs during a respiratory cycle. This typically measures around 400 ml in an average healthy woman and 500 ml in a healthy man (Hallett et al, 2023). In the prehospital setting, manual ventilation requires the use of a standard 1500 ml, adult bag-valve-mask (BVM) (Prekker and Robinson, 2023). This is approximately three times the requirement for an average adult, posing a risk of inadvertent hyperinflation, and associated adverse outcomes.
Hyperinflation resulting from excessive TV has detrimental effects in both prehospital cardiac arrest and traumatic brain injury patients (Baez et al, 2022). The adverse effects of high TV ventilation include elevated intrathoracic pressure, reduced venous return, decreased preload, and hypotension (Pitts and Kellermann, 2004). There is a paucity of outcome-specific evidence; however, these impacts are hypothesised to affect patient outcomes, particularly by reducing the likelihood of ROSC in OHCA patients.
LPTVs are also linked to a reduced likelihood of pulmonary complications, including acute respiratory distress syndrome (ARDS), in ventilated patients (Neto et al, 2015; Stoltze et al, 2015). This is particularly pertinent in the prehospital setting, as nearly half of OHCA patients who survive at least 48 hours develop ARDS (Johnson et al, 2019). Acute lung injuries are also associated with hyperinflation (Mohr and Fuller, 2012). Although there is a paucity of evidence, the aforementioned adverse effects of high TV ventilation suggest that even short-term hyperinflation impacts the onset or diagnosis of ARDS during the patient's recovery.
TV is typically estimated in reference to the patient's weight. Weight measurements in clinical settings often vary, with several abbreviations used interchangeably. Actual body weight (ABW) and total body weight (TBW) are synonymous and represent the patient's actual weight (MacDonald et al, 2015). Ideal body weight (IBW) and predicted body weight (PBW) both use the individual's height to calculate their optimum weight; however, each uses a marginally different formula (MacDonald et al, 2015). Both IBW and PBW have gender-specific formulas to accommodate physiological differences between genders. In many studies, the terms IBW and PBW are used interchangeably (Mackenzie and Lever, 2007). Unless specified by a cited article, the terms IBW and PBW are considered synonymous throughout the current review, and PBW will be used to encompass both.
Height, used to calculate PBW, correlates with lung capacity more closely than ABW (Martin and Richards, 2017). TV has a slightly negative association with patient obesity (Erstad, 2021), underscoring the necessity of employing PBW for calculating TV. ABW typically exceeds PBW by over 30%, with an associated increase in the calculated TV (Bojmehrani et al, 2014). This underlines the necessity for a reliable PBW calculation tool.
The Joint Royal Colleges Ambulance Liaison Committee (JRCALC) national clinical guidelines recommend a ventilation volume of 6–7 ml/kg, with a further mention of approximately 600 ml for most adults (Association of Ambulance Chief Executives (AACE), 2022). The guidelines do not specify whether ABW or PBW should be used. However, given the absence of tools for height estimation in the prehospital setting, it is reasonable to assume that this calculation relies on a visual estimation of ABW.
While 6–7 ml/kg is widely practised as a lung-protective (LP) measure to mitigate hyperinflation and barotrauma (Hallett et al, 2023), the fixed volume of 600 ml may be excessive for many patients. The average UK male is 175 cm (NHS England, 2022), with a PBW of 71 kg. At 6–7 ml/kg, as per JRCALC guidelines, this patient requires 426–497 ml. If ventilated at 600 ml, most of the UK population would be receiving excessive TVs.
There is a paucity of evidence on the exact time it takes for the adverse effects of hyperventilation with high TVs to occur. However, given the substantial evidence demonstrating the harm hyperventilation can cause, the priority should be to always ventilate patients within safe parameters. TV during air ambulance transport has been shown to strongly predict intensive care unit (ICU) TV, with patients exposed to high prehospital TVs being more than three times as likely to also receive high TVs in the ICU (Moy et al, 2022). This underscores the importance of initiating LPTV treatment as early as possible, starting in the prehospital setting.
There is currently scant evidence relating to the use of validated tools for calculating weight/height in UK ambulance services. Consequently, paramedics rely on visual weight estimation, which is typically inaccurate (Wells et al, 2023a). Inaccurate PBW directly impacts the accuracy of the administered TV.
Methods
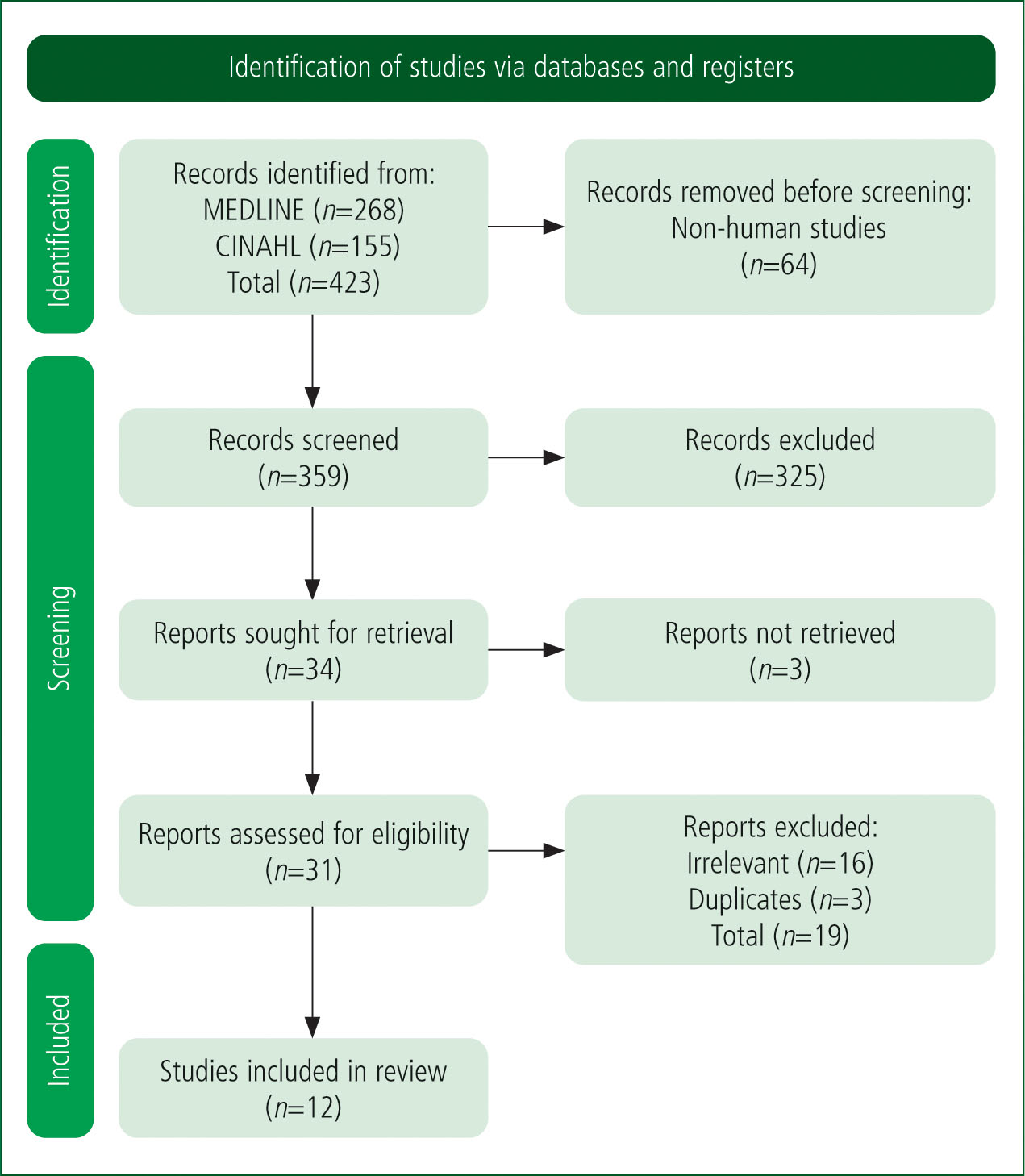
A Boolean search strategy was employed using the following terms: (tidal volume or PAWPER or Broselow) AND (estimat* or calculat*) AND (tape or tool or biometric). To ensure a comprehensive examination of weight-estimation tools, encompassing not only those specific to TV research but also paediatric tools adapted for adult use, the search terms (PAWPER or Broselow) were included. Animal studies were excluded.
A systematic literature search was conducted in MEDLINE (n=218) and CINAHL (n=141) databases. After reviewing 359 abstracts, 325 studies were excluded as not relevant. After subsequent full-text review, 12 studies were included (Figure 1)
All primary research papers (n=11) underwent quality assessment using the Newcastle-Ottawa Scale (NOS) as modified by Wells et al (2023a). This adaptation was designed to consider weight-estimation studies but is deemed suitable for evaluating height-estimation tools, making it suitable for use in this literature review. Scores from 6–10 indicate high quality; those from 4–5 suggest a moderate risk of bias; and 0–3 indicate a very high risk of bias.
The accuracy of each tool was assessed against a threshold accuracy level: 70% of estimations within 10% of actual weight (PW10>70%), and 95% within 20% of actual weight (PW20>95%). This criterion has previously been used in determining the accuracy of both height and weight estimations. The included categories for summarisation of results are as follows: authors and publication year; study size (N); country of study; weight-estimation techniques evaluated; weight-or height-based findings; TV-based findings; comments; modified NOS; limitations and gender split.
Results
The findings following the evaluation of each study are presented in Appendix 1 (online). The modified NOS score analysis revealed that 75% of the studies were classified as high-quality studies with a low risk of bias. Additionally, Deane et al (2008) was identified as having a moderate risk of bias, while Jurecki et al (2015) was deemed to have a very high risk of bias.
Several studies failed to achieve PW10>70% and PW20>95% accuracy and many failed to utilise robust reference weights or heights, thereby reducing the probability of achieving accuracy in their results.
The Modified PAWPER XL-MAC-2 (Wells et al, 2022), ulna length, and lower-leg length (Bojmehrani et al, 2014) all attained PW10>70%. Although Barbosa et al's (2012) study exploring ulna length did not record PW (n) data, the PW (n) data from Bojmehrani et al (2014) applies as the methods are identical. Additionally, the biometric tool based on DS (O'Brien et al, 2019) performed well, directly calculating TVs with ≤7 ml/kg PBW accuracy at 91%.
Discussion
Accuracy of height-or weight-estimation techniques
Several PBW studies demonstrated accuracy, including Bojmehrani et al (2014), where both forearm and lower-leg methods achieved PW10>70%. Additionally, Barbosa et al (2012) highlighted the effectiveness of ulna-length measurements, while Wells et al (2022) underscored the accuracy of the Modified PAWPER XL-MAC-2.
The majority of the tools focused on weight, facilitating subsequent calculation of TV. However, O'Brien et al (2019) created a biometric TV tape, enabling direct measurement of TV. This disposable tape displays gender-specific PBW and TV markings, eliminating the need for calculations. This tape demonstrated its efficacy in providing accurate estimates of LPTVs, with 91% compliance achieved for TVs ≤7 ml/kg. However, while this aligns with JRCALC guidance (AACE, 2022), this may still represent non-LPTVs. Barbosa et al's (2012) ulna-length tool, Wells et al's (2022) Modified PAWPER XL-MAC-2, and O'Brien et al's (2019) biometric TV tape have demonstrated good accuracy, so their suitability for the prehospital environment will be examined further.
Conversely, certain tools exhibited significant inaccuracies and should be disregarded for potential future use in prehospital settings. Visual estimation results in substantial deviations in predicted height or weight (Bojmehrani et al, 2014; Sasko et al, 2018; Ives Tallman et al, 2021), resulting in incorrect TVs.
The Broca and Buckley methods (Akinola et al, 2021) also demonstrate poor accuracy. The Broca formula estimates PBW using height measurements and the Buckley method estimates the less helpful TBW using arm and thigh circumference. Neither approach is suitable for practice. In the prehospital setting, access to patients' healthcare records could aid in accurate height estimation if data were precise; however, electronic health record (EHR) height data exhibited inaccuracies, rendering it unreliable (Jurecki et al, 2015; Mohamed et al, 2023). Patient self-estimation of height also proved inaccurate, with a PW20 of 86.1% (Akinola et al, 2021). The Modified PAWPER XL-MAC-2 displayed high accuracy (Wells et al, 2022) but subsequently calculated TBW, making it unsuitable for calculating TV.
In comparison to the ulna-length and lower-leg methods, the tape-measure method, despite its apparent simplicity, only marginally meets the PW10>70% criteria, with 25% of measurements resulting in errors over 10%, in contrast to 15% for both ulna-length and lower-leg measurements (Bojmehrani et al, 2014). The reduced accuracy makes it a suboptimal tool to be considered for use in the prehospital setting. Furthermore, the lower-leg measurement requires specialist equipment and for the patient to be seated.
TV calculation formulas
The estimation of TV using height involves the application of equations to determine PBW, subsequently utilised in calculating TV. However, the complexity of these formulas elevates the risk of calculation errors – a concern particularly pertinent in resource-constrained prehospital settings.
One effort to address the complexity issue introduced a formula noted for its simplicity and low error rate (Oh et al, 2021). The authors suggest that their formula holds promise for routine clinical application – serving not only as a primary method for calculating PBW, but also as a secondary tool for validating results obtained from more complex formulas or electronic devices (Oh et al, 2021). The introduction of simpler equations offers promise for accurate PBW calculations, potentially improving clinical practice and reducing errors.
Neither the Modified PAWPER XL-MAC-2 (Wells et al, 2022) nor the biometric TV tape (O'Brien et al, 2019) necessitate a formula, whereas the ulna measurement approach does (Barbosa et al, 2012; Bojmehrani et al, 2014). Even the simpler alternatives to the Devine formula (Erstad, 2021) should be confirmed by a wider team to mitigate risk. Therefore, tools that do not require these calculations may be better suited to the prehospital setting.
Applicability to different ethnic groups
While several of these tools demonstrated accuracy within their study, many lacked robust testing across diverse ethnic backgrounds. Demi-span (DS) (from the middle of the sternal notch to the tip of the middle finger with the arm abducted 90o) measurements across various ethnic groups differ significantly, indicating potential anatomical variations among different populations (Lahner et al, 2017). This finding could undermine studies such as Deane et al (2008) and O'Brien et al (2019), which used DS. The former had a small sample size with limited ethnic diversity, while the latter did not collect ethnicity data. Therefore, the tools in these studies may not be generalisable across ethnic groups without modification.
Studies investigating the correlation between ulna length and height in South African (Van den Berg et al, 2016) and Greek populations (Pafili et al, 2018) have demonstrated inaccuracies in this method for both groups. Given the widespread usage and extensive study of the tool, it is presumed that these discrepancies arise because the initial development of the tool was based on studies involving participants from different ethnic backgrounds. Bojmehrani et al (2014) and Barbosa et al (2012) focused on ulna length. However, neither study encompassed a sufficiently diverse ethnic population to determine the transferability of ulna-length measurements to different ethnic groups.
One UK study (Madden et al, 2020) sought to address the paucity of accurate equations for calculating height based on anthropometric measurements among non-white ethnic backgrounds. Measurements were collected from a diverse cross-section of the UK population; this was used to develop new equations for predicting height from ulna length. Comparison with a historic dataset revealed that these new equations offer mean predicted height values closer to measured height than the currently employed malnutrition universal screening tool (Madden et al, 2020). Implementing these findings would enable clinicians to calculate a more accurate TV, across ethnicities, although the clinician would need to select the appropriate formula. However, the Modified PAWPER XL-MAC-2 exhibited a PW10 of 99.9% across all ethnic groups (Wells et al, 2022), indicating its adaptability to diverse patient populations in the prehospital setting. This finding highlights its utility as a universal tool, eliminating the complexity and potential for increased risk of human error associated with switching formulas between patients of various ethnic backgrounds.
Applicability to different subgroups
Female patients are at elevated risk of receiving excessive TVs (Fernandez-Bustamante et al, 2011). There is a gender disparity in initial ventilation settings, with a significantly higher proportion of females (56%) initially ventilated with TVs ≥8 ml/kg compared with males (9%) (Isenberg et al, 2020). It has been suggested that frequent overestimation of shorter heights leads to higher PBWs and subsequently, higher TVs (Sasko et al, 2018).
In future studies evaluating these tools, achieving gender balance is critical – particularly as many of the evaluated studies were skewed towards male participants. By ensuring adequate representation of female participants, researchers can comprehensively evaluate the accuracy of weight-or height-estimation techniques across diverse populations. Obese patients are at high risk of receiving excessive TVs (Lellouche et al, 2012) owing to larger disparities between ABW and PBW. It is therefore important to use PBW to calculate TV in these patients.
The Modified PAWPER XL-MAC-2 demonstrated the highest level of accuracy in both sub-groups with a large study population (n=5926) (Wells et al, 2022). These findings carry even greater significance when considering the relatively small study sizes of O'Brien et al (2019) (n=82), Bojmehrani et al (2014) (n=100) and even Barbosa et al (2012) (n=507).
Practical considerations
There is a paucity of evidence relating to the use of these tools in time-critical situations, and no studies were undertaken in the prehospital setting. For prehospital environments, the ideal method should be accurate, rapid, and straightforward to use (Wells et al, 2023b). In scenarios where ventilation is required, there may only be two clinicians present, with limited additional resources available. Therefore, the ability to readily employ these tools is paramount.
Among the three identified tools, two demonstrate evidence of rapid usability: ulna-length measurement typically takes less than a minute and the Modified PAWPER XL-MAC-2 can be completed within 40 seconds (Wells et al, 2022). It has been indicated that the DS measurement for the tidal tape can also be obtained rapidly (Frid et al, 2013); however, the absence of a definitive time frame renders this conclusion subjective.
Two of the three tools (ulna length and Modified PAWPER XL-MAC-2) require the clinician to make some form of calculation (Table 1). Ulna length is used to calculate PBW; this is reliant on the clinician using the correct formula for the patient's ethnicity. Both tools subsequently require the clinician to calculate TV using the guideline of 6–7 ml/kg (AACE, 2022); again, this has been shown to be problematic. Conversely, the DS tidal tape directly provides TV, obviating the requirement for further calculations.
| Tool | Method |
|---|---|
| Ulna length (Barbosa et al, 2012; Bojmehrani et al, 2014) | Distance between olecranon process and ulnar styloid process with arm folded across chest |
| Modified PAWPER XL-MAC-2 (Wells et al, 2022) | Recumbent length |
| Biometric tidal tape (O'Brien et al, 2019) | DS from sternal notch to finger roots with arm outstretched laterally |
Abbreviations: PBW=predicted body weight; TV=tidal volume; DS=demi-span
While the tidal tape negates calculations, the physical environment must be considered, particularly in terms of restricted space. Acquiring the DS reading requires two clinicians and adequate space to laterally outstretch the patient's arm. Thus it may not be feasibly adaptable for prehospital use. Conversely, ulna length can be measured by one clinician and height can be measured with brief assistance from a second person. As the Modified PAWPER XL-MAC-2 directly calculates PBW, eliminating the extra step required with ulna length, it should be considered the preferred tool when considering accuracy, ease, and speed of use.
Limitations
Limitations within reviewed studies
Overall, several limitations were consistently observed across the studies; primarily, the lack of a diverse sample population, particularly regarding ethnicity. An exception to this was the Modified PAWPER XL-MAC-2 tool, which demonstrated accuracy across all ethnic groups.
Numerous studies exhibited a skewed gender ratio. Given that females are at heightened risk of high TVs, this gender disparity warrants attention in future research to promote gender equality and bridge this research gap.
There is a significant paucity of prehospital research or evidence. Consequently, while the evaluated tools may demonstrate accuracy under controlled conditions, their prehospital efficacy remains uncertain.
Limitations within this systematic literature review
The paucity of evidence regarding the use of TVs, and the use of weight/height tools on adults in the prehospital setting posed limitations to this review. Although the tools found to be accurate in hospital settings were assessed for adaptability to the prehospital setting, their suitability is uncertain without further research.
Additionally, there is a risk of subjectivity as both the ulna length and the Modified PAWPER XL-MAC-2 deemed suitable for use in the prehospital setting by the authors of this paper – one of whom was a student paramedic at the time of writing, and the other who has been a registered paramedic since 2008. The Modified PAWPER XL-MAC-2 was deemed by the authors to likely be quicker and easier to use. However, in practice, ulna length may prove superior; further studies are needed for certainty.
Conclusions
In prehospital settings, LP volumes of 6–7 ml/kg are recommended by JRCALC guidelines (AACE, 2022). However, there are currently no tools available to determine adult patients' weight or height. Subsequently, TVs are calculated by unreliable visual estimations of ABW. This highlights the need for a tool in prehospital settings to accurately calculate LPTVs to prevent adverse outcomes.
Three tools – ulna length, tidal tape, and Modified PAWPER XL-MAC-2 – demonstrated good accuracy. The Modified PAWPER XL-MAC-2 tool was identified as most likely to yield accurate results in the prehospital setting. However, evidence of its efficacy in treating acutely unwell, prehospital patients is lacking. Given the potential impact of hyperinflation in OHCA, a reliable, prehospital TV calculation tool is required as a matter of urgency. It is further suggested that the JRCALC guidelines (AACE, 2022) be reviewed to better reflect the findings of the present review.
Ambulance services using ventilators could rapidly benefit from a tool like the Modified PAWPER XL-MAC-2, once its effectiveness is validated in prehospital care. However, BVMs are more commonly available and used in UK ambulance settings, creating an additional challenge for delivering LPTVs to patients. To ensure accurate TVs with BVM use, a feedback monitoring device is essential. A further literature review is required to identify the most suitable device for this purpose.


